Abstract
Introduction Leukemic relapse is reduced following cord blood transplantation (CBT) compared to other cell sources with improved survival in those with residual disease. In xenograft models, cord CD8 T cells exert a superior graft-vs-leukemia effect compared to adult T cells, but T cell reconstitution after CBT is CD4 biased. We have previously observed early, CD8 T cell expansion in children transfused with third party granulocytes for infection following CBT that induced sustained remission without chronic graft-vs-host disease (GVHD).
We now report data from an investigator-led clinical trial to assess the effects of granulocyte transfusions following CBT (ClinicalTrials.Gov NCT05425043), in a study cohort of children with relapsed, refractory leukemia after a previous transplant.
Methods Single-centre study of children with post-transplant relapsed, refractory leukemia, who received T-replete, HLA-mismatched (5/8-7/8) CBT and 7 doses of granulocytes (up to 200ml). Granulocytes were a pooled component derived from whole blood (NHS Blood and Transplant). Tolerability of granulocytes, cytokine release syndrome (CRS) and outcome data including disease response, transplant related mortality and GVHD were recorded. A historical cohort of 28 T-replete CBT recipients without granulocytes was used for comparison. Mann-Whitney test used to compare study group with controls.
Multi-parameter flow cytometry was performed during T cell expansion to characterise immunophenotypic profile. T cell receptor sequencing and serum cytokine analysis is ongoing.
Results 9 patients are enrolled and evaluable to date. All 9 patients had refractory, relapsed acute myeloid leukemia (AML) after a previous transplant. 8 patients (88.9%) had detectable disease, including frankly relapsed (n=4), at the time of transplant. Granulocytes were started between days - 4 and +16. Granulocyte transfusions were well tolerated.
Disease response and GVHD
1 patient without T cell expansion had primary graft failure and died with detectable leukemia. 1 patient with T cell expansion and engraftment had detectable disease at day 28. The remaining 7 patients (77.8%) with expansion and engraftment achieved remission. 1 died in remission with disseminated, drug-resistant HSV, 1 relapsed 6 months after transplant, and 5 patients (55.6%) are alive and in molecular or flow remission with a median follow up of 6 months (range 3- 6 months). Grade II-IV GVHD seen in 4 patients (44.4%).
T cell expansion
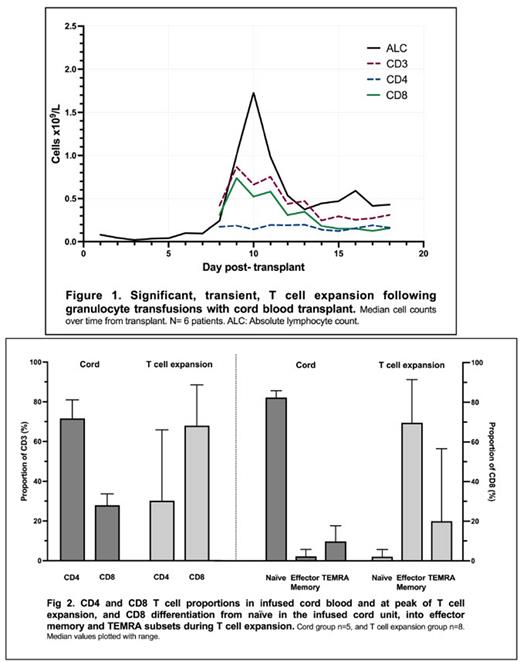
T cell expansion was seen in 8 patients (88.9%). The peak absolute lymphocyte count (ALC) in the 7 days post-granulocytes was higher than the peak between days 7-13 in the control group (1.49 x109/L vs 0.1 x109/L (p<0.0001)). The median time to peak ALC was 10 days (range 9- 26 days), and to subsequent nadir was 3.5 days (range 2- 6 days) in the study group, Fig 1. T cells were predominantly CD8+ (median 68%, range 32.6- 88.5%), of CCR7-/CD45RA- effector memory phenotype (median 67.3%, range 32.1- 91.4%), Fig 2. These cells displayed markers of activation with increased HLA-DR and CD38 expression (median 30.3%, range 15.4- 78.5%), cytotoxic potential with granzyme B (median 86.6%, range 64.8- 93.9%) and perforin (median 6.43%, range 0.54- 40.6%) expression and production of interferon gamma (median 38.6%, range 13.1- 61%) and tumour necrosis factor alpha (median 1.2%, range 0.1- 4.8%) on stimulation.
Engraftment
There was no significant difference between groups in the time to neutrophil engraftment (median 18.5 vs 20 days). Platelet engraftment was delayed (median 90.5 vs 40 days (p=0.037)) with consumptive thrombocytopenia.
CRS
Grade 1-2 CRS seen in all patients. Granulocyte infused patients had more days of fever within first 7 days post-CBT (median 5.5 vs 2 days (p=0.0002)), a higher maximum temperature, (median 40.3oC vs 39.0oC (p=0.0021)), and an earlier onset of fever (median day 2 vs day 5 (p=0.0129)). The peak c-reactive protein in the first week was greater in the treated than control group (median 200 mg/L vs 32 mg/L (p=0.0005)).
Conclusions We confirm induction of remission and CRS in patients with very high-risk AML and reproducible, massive, effector memory CD8+ T-cell expansion after CBT, induced by granulocytes. This expansion and disease response is likely secondary to mismatched HLA and antigen presentation by the product and augments the utility of CBT in such high risk leukemia.
Disclosures
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.