In this issue of Blood, Ruggeri et al identify a novel mechanism by which donor NK cells in an allograft accelerate posttransplant immune reconstitution.1 In allogeneic bone marrow transplantation, a critical question has been how donor hematopoietic cells can eliminate cancer and restore normal blood counts with limited off-target graft-versus-host immune pathology. Twenty years ago, the Perugia team published a seminal report in Science that showed donor alloreactive NK cells reduce graft-versus-host disease (GVHD) in allogeneic transplants by ablating recipient antigen-presenting cells.2 Now the team, led by Loredana Ruggeri and Andrea Velardi, has addressed the issue of how transplantation may lead to accelerated immune reconstitution. This question is of particular importance in the context of allo-transplant using grafts consisting of CD34+ donor hematopoietic progenitor cells depleted of donor T cells, B cells, and NK cells.
In the 1990s, the Perugia team built on earlier work from Memorial Sloan Kettering Cancer Center using T cell-depleted allografts in children.3 Massimo Martinelli adopted the strategy of using high-dose T cell-depleted blood stem cell grafts from donors mismatched at multiple HLA loci to transplant pediatric and adult recipients.4 Recipients of a T cell-depleted, CD34+ cell-selected graft had marked and early expansion of donor-derived NK cells that had antileukemia activity based on mismatches between donor KIR and recipient HLA molecules that led to NK cell activation.2 Applying CD34+ cell-selected transplants in adult patients resulted in a very low incidence of acute and chronic GVHD, but transplants were complicated by delays in T-cell reconstitution, higher infection rates, and increased treatment-related mortality compared with the same approach in pediatric patients. These observations led to hypothesis that compromised thymic function from age-dependent involution contributed to impaired thymopoiesis in adults.5 The technical complexity of CD34-cell selection and the perceived deficits in posttransplant immune reconstitution using grafts depleted of T cells has led to the adoption of a strategy of in vivo T-cell depletion using posttransplant administration of high-dose cyclophosphamide6 and clinical trials of cytokines such as keratinocyte growth factor and interleukin-22 to support the growth of thymic epithelial cells.7 Although using either ex vivo or in vivo T-cell depletion in allogeneic transplantation has allowed transplantation across HLA barriers and expanded the donor pool to include haploidentical related donors previously excluded because of unacceptably high rates of GVHD, progress is still needed to achieve the goal of rapid restoration of blood counts without GVHD. Alternative methods that deplete or inhibit activated and alloreactive donor T cells using antithymocyte globulin or alemtuzumab serotherapy, or the use of costimulatory blockade with abatacept are relatively simple. However, anti-T-cell serotherapy and CD34 cell selection of the graft are associated with delays in T-cell reconstitution and the potential for increased relapse8,9 compared with standard GVHD prophylaxis. The question of how to accelerate immune reconstitution following depletion of donor T cells remains a pressing question for the transplant field.
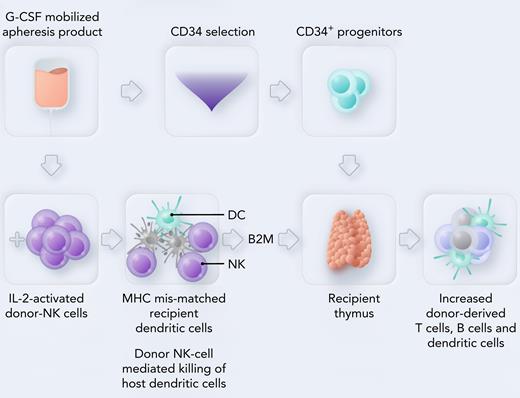
The new report from Perugia shed some light on this issue in a study that represents the culmination of years of persistence from the team in unraveling how major histocompatibility complex (MHC) mismatched donor NK cells mediate favorable clinical outcomes. Ruggeri et al noted accelerated immune reconstitution in murine recipients of MHC mismatched marrow cells and interleukin-2 activated NK cells. Using an elegant series of mouse transplants into radiation chimeras, they identified direct interactions between donor NK cells and MHC mismatched recipient dendritic cells as necessary for enhanced donor T-cell regeneration posttransplant. They demonstrated that the supernatant from cocultures of alloreactive donor-type NK cells and host-type dendritic cells promoted thymic epithelial cell proliferation. Biochemical studies show the factor(s) secreted from cocultures of alloreactive donor-type NK cells and recipient-type dendritic cell (DC) is newly synthesized, trypsin-sensitive, absent when alloreactive NK cells are cocultured with beta2 microglobulin knock-out/knock-down DC, partially depleted by anti-beta2 microglobulin antibodies, and has the molecular weight and mass spectroscopy signature of beta2 microglobulin. Confirmation of the identity of beta2 microglobulin as the most likely candidate of the “immune rebuilding factor” was supported by a combination of chromatography, gel electrophoresis, mass spectrometry, and the activity of recombinant human B2M in enhancing thymic epithelial cell proliferation. Together, these data support a model by which donor NK cells kill recipient-type DC in the first days after allo-transplant, releasing beta2 microglobulin that enhances immune reconstitution by sustaining the proliferation of thymic epithelial cells (see figure).
Mechanism that activated donor NK cells facilitate T-cell reconstitution in allogeneic hematopoietic stem cell transplant recipients by killing host-type dendritic cells and releasing beta2 microglobulin. Professional illustration by Somersault18:24.
Mechanism that activated donor NK cells facilitate T-cell reconstitution in allogeneic hematopoietic stem cell transplant recipients by killing host-type dendritic cells and releasing beta2 microglobulin. Professional illustration by Somersault18:24.
The paper by Ruggeri et al adds to our knowledge of the intricacies of posttransplant immune reconstitution. It supports current efforts in graft engineering to select the optimal combination of donor cells. These data suggest opportunities for new therapeutic interventions to promote thymic regeneration and enhance immune reconstitution, as well as “graft engineering” strategies that select specific subsets of donor cells for transplantation. The selection of CD34+ cells combined with defined numbers of conventional T cells, T-regulatory, iNK cells, or NK cells represents strategies successfully developed in murine bone marrow transplantation models and currently being evaluated in clinical trials.10 The study by Ruggeri et al thus provides novel mechanistic insights into the facilitation of T-cell reconstitution by transplant strategies involving graft engineering with donor NK cells. These new data will likely lead to therapeutic interventions to enhance T-cell reconstitution in HLA-mismatched allogeneic transplant recipients.
Conflict-of-interest disclosure: E.K.W. declares no competing financial interests.