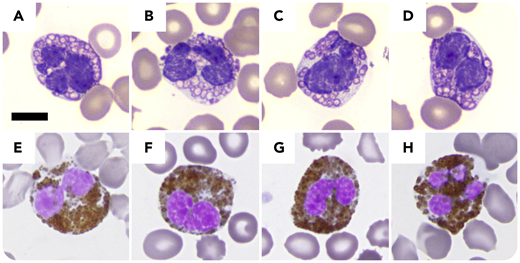
A 72-year-old woman with chronic myelomonocytic leukemia, recently progressed to acute myeloid leukemia and extensive tinea pedis, presented with fever (38.1°C) shortly after a third cycle of decitabine. Workup revealed normocytic anemia (hemoglobin, 6.9 g/dL; mean corpuscular volume, 100 fL), thrombocytopenia (platelets, 16 × 103/µL), leukopenia (white blood cells, 3.7 × 103/µL), neutropenia (0.74 × 103/µL), increased (1-3)-β-d-glucan (309 pg/mL), and normal chest radiograph, lactate, urinalysis, blood culture, and galactomannan. Peripheral blood smear identified 11% neutrophils containing unevenly distributed cytoplasmic spherical forms with peripheral rimming and occasional central dots, which, after a microbiology consultation, were deemed morphologically compatible with intracellular yeast forms of histoplasma (panels A-D: original magnification ×100, Wright-Giemsa stain). Subsequent urine histoplasma antigen was negative. Furthermore, the cytoplasmic “yeast forms” were positive for myeloperoxidase (panels E-H: original magnification ×100, myeloperoxidase stain). Taken together with bone marrow findings of increased blasts and dyspoiesis, the cytoplasmic findings were recognized as markedly dysplastic neutrophilic granules.
Invasive fungal infections occur in ∼10% of patients with myeloid neoplasms during treatment with hypomethylating agents. This case illustrates that markedly dysplastic neutrophilic granules can mimic yeast forms and pose a diagnostic challenge, especially in patients with myeloid neoplasms in the setting of febrile neutropenia. A myeloperoxidase cytochemical stain can be helpful to differentiate them.
A 72-year-old woman with chronic myelomonocytic leukemia, recently progressed to acute myeloid leukemia and extensive tinea pedis, presented with fever (38.1°C) shortly after a third cycle of decitabine. Workup revealed normocytic anemia (hemoglobin, 6.9 g/dL; mean corpuscular volume, 100 fL), thrombocytopenia (platelets, 16 × 103/µL), leukopenia (white blood cells, 3.7 × 103/µL), neutropenia (0.74 × 103/µL), increased (1-3)-β-d-glucan (309 pg/mL), and normal chest radiograph, lactate, urinalysis, blood culture, and galactomannan. Peripheral blood smear identified 11% neutrophils containing unevenly distributed cytoplasmic spherical forms with peripheral rimming and occasional central dots, which, after a microbiology consultation, were deemed morphologically compatible with intracellular yeast forms of histoplasma (panels A-D: original magnification ×100, Wright-Giemsa stain). Subsequent urine histoplasma antigen was negative. Furthermore, the cytoplasmic “yeast forms” were positive for myeloperoxidase (panels E-H: original magnification ×100, myeloperoxidase stain). Taken together with bone marrow findings of increased blasts and dyspoiesis, the cytoplasmic findings were recognized as markedly dysplastic neutrophilic granules.
Invasive fungal infections occur in ∼10% of patients with myeloid neoplasms during treatment with hypomethylating agents. This case illustrates that markedly dysplastic neutrophilic granules can mimic yeast forms and pose a diagnostic challenge, especially in patients with myeloid neoplasms in the setting of febrile neutropenia. A myeloperoxidase cytochemical stain can be helpful to differentiate them.
For additional images, visit the ASH Image Bank, a reference and teaching tool that is continually updated with new atlas and case study images. For more information, visit http://imagebank.hematology.org.