Key Points
The rate of symptomatic postdischarge VTE following hospitalization with COVID-19 is low.
Abstract
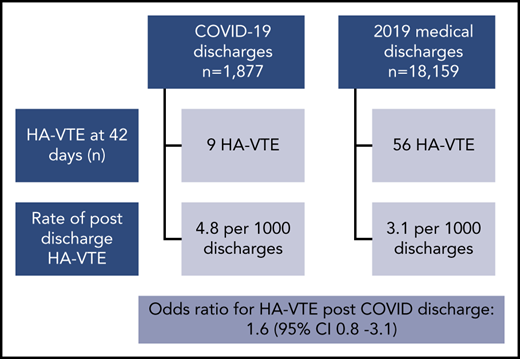
The association of severe coronavirus disease 2019 (COVID-19) with an increased risk of venous thromboembolism (VTE) has resulted in specific guidelines for its prevention and management. The VTE risk appears highest in those with critical care admission. The need for postdischarge thromboprophylaxis remains controversial, which is reflected in conflicting expert guideline recommendations. Our local protocol provides thromboprophylaxis to COVID-19 patients during admission only. We report postdischarge VTE data from an ongoing quality improvement program incorporating root-cause analysis of hospital-associated VTE (HA-VTE). Following 1877 hospital discharges associated with COVID-19, 9 episodes of HA-VTE were diagnosed within 42 days, giving a postdischarge rate of 4.8 per 1000 discharges. Over 2019, following 18 159 discharges associated with a medical admission; there were 56 episodes of HA-VTE within 42 days (3.1 per 1000 discharges). The odds ratio for postdischarge HA-VTE associated with COVID-19 compared with 2019 was 1.6 (95% confidence interval, 0.77-3.1). COVID-19 hospitalization does not appear to increase the risk of postdischarge HA-VTE compared with hospitalization with other acute medical illness. Given that the risk-benefit ratio of postdischarge thromboprophylaxis remains uncertain, randomized controlled trials to evaluate the role of continuing thromboprophylaxis in COVID-19 patients following hospital discharge are required.
Introduction
Severe acute respiratory syndrome coronavirus 2 and the resultant coronavirus disease 2019 (COVID-19) are responsible for an ongoing pandemic. Although pneumonia and respiratory failure are the prominent presentations in those requiring hospitalization, venous thromboembolism (VTE) has emerged as a common complication, particularly in the critically ill.1-5 This led to publication of expert guidance documents, but with a limited evidence base and, therefore, conflicting recommendations for prevention of VTE in COVID-19.6,7 The need for postdischarge thromboprophylaxis is an area of conflict due to a lack of data reporting the incidence of VTE following hospitalization for COVID-19, and the limited evidence of overall benefit following medical admission in pre-COVID studies.8 We report the rates of postdischarge VTE and compare with rates following medical admission in the pre-COVID era.
Study design
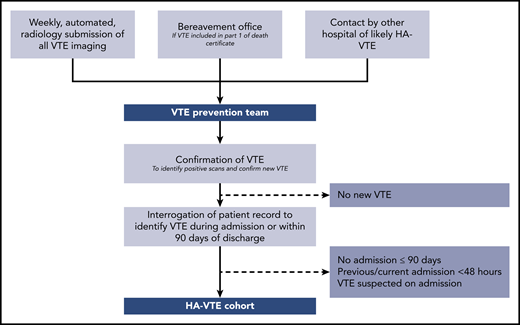
King’s College Hospital consists of 2 hospital sites providing acute medical care in south London in the United Kingdom: Denmark Hill and Princess Royal University Hospital. Both sites have established VTE prevention programs incorporating documented VTE risk assessment of all patients on admission since 2010,9 and a unified approach to thromboprophylaxis since 2014. A continuous quality improvement program incorporating root-cause analysis of all episodes of hospital-associated VTE (HA-VTE) was established in 2010 and 2014 at Denmark Hill and Princess Royal University Hospital, respectively. VTE imaging is performed following clinical assessment using pretest probability (and d-dimer when appropriate).10 Routine screening of asymptomatic patients is not performed. Any VTE diagnosed during/following a medical admission of >48 hours, or postoperatively and occurring up to 90 days of discharge, is considered HA-VTE. An automated weekly list of all patients with any VTE imaging (computed tomography pulmonary angiogram, ventilation/perfusion scans, upper- and lower-limb deep vein thrombosis [DVT] scans) is generated by radiology and e-mailed to the VTE prevention team. The VTE prevention team reviews all imaging reports to identify those confirming VTE and then cross-references with electronic patient records to identify events meeting these criteria as previously described and summarized in Figure 1.11 Of note, VTE imaging can only be performed in the hospital setting and patients presenting to primary care are referred for evaluation at the hospital using well-established pathways for suspected VTE. Additionally, the bereavement office provides details of any VTE-related deaths, and links have been established between VTE prevention teams throughout south London to communicate potential HA-VTE to the primary admitting site. Our thromboprophylaxis guidance includes weight-based enoxaparin for all patients at high risk of VTE in the absence of bleeding risk factors (Table 1). From 22 April 2020, for patients admitted to critical care with COVID-19, thromboprophylaxis was intensified to intermediate-dose enoxaparin (until discharge back to a ward setting; supplemental Table, available on the Blood Web site). Thromboprophylaxis is withdrawn on hospital discharge. All patients receive the following written information regarding VTE risk as part of their discharge summary: “A possible complication of being admitted to hospital is blood clots in the leg or the lung (deep vein thrombosis or pulmonary embolism). After going home, if you experience leg pain or swelling or any chest pain or breathlessness, you should seek medical advice.”
We report all HA-VTE events associated with a medical admission from 3 March to 7 May 2020 and, specifically, postdischarge HA-VTE events following an admission with COVID-19 diagnosed up until 17 June 2020 (and occurring within 6 weeks of a previous admission). We also report a comparison cohort of postdischarge HA-VTE following a medical admission in 2019. The odds ratio (OR; with 95% confidence intervals [CIs]) for postdischarge VTE associated with COVID-19 compared with the 2019 cohort was calculated using a 2 × 2 contingency table and the χ2 test. Further ORs, to evaluate the effect of missing events in each time period, were similarly calculated after inflating the actual number of HA-VTE events by 10%, 25%, or 50%. Statistical analysis was performed with SPSS v24 (IBM, Chicago, IL). As data collection was part of an ongoing quality improvement project, ethics approval was not required.12 The study was conducted in accordance with the Declaration of Helsinki.
Results and discussion
Over the period of interest, there were 2863 COVID-19 admissions: 1877 of these patients were discharged on or before 7 May 2020, including 208 admitted to critical care. Of the 84 HA-VTE episodes, 9 (11%) occurred postdischarge at a median of 8 days (range, 3-33 days). The proportion of discharged patients who developed HA-VTE was 4.8 per 1000 discharges (within 42 days of discharge); of these, 2 had proximal DVT and 7 experienced pulmonary embolism (PE). One patient required critical care admission during a previous hospital stay. Eight patients received inpatient anticoagulant thromboprophylaxis (including 2 on long-term anticoagulation for atrial fibrillation). One patient did not receive anticoagulant thromboprophylaxis due to active bleeding.
Over 2019, 18 159 hospital discharges followed a medical admission and 85 experienced postdischarge HA-VTE, at a median of 29 days (interquartile range, 16-51 days) postdischarge. Fifty-six episodes (66%) of HA-VTE occurred within 42 days of discharge, giving a rate of 3.1 per 1000 discharges. Of these, 8 events were proximal (14%), 10 were distal (18%), and 5 were line-associated upper-limb DVT (9%), with 33 experiencing PE (57%). Four patients (7%) required critical care admission during their previous hospital stay. Forty-seven patients received inpatient thromboprophylaxis, including 4 patients on long-term anticoagulation for preexisting indications. Nine patients did not receive thromboprophylaxis due to contraindications (acute stroke, n = 2; severe thrombocytopenia, n = 2; active bleeding, n = 5). The OR for postdischarge HA-VTE following hospitalization with COVID-19, compared with 2019 medical admissions, was 1.6 (95% CI, 0.77-3.1; P = .2). Excluding patients diagnosed with VTE during hospitalization did not significantly alter this finding (data not shown). Because it is possible cases of HA-VTE were missed due to patients not returning to the hospital with new symptoms, we considered the effect of having missed 10%, 25%, or 50% of HA-VTE events. The OR for HA-VTE only reached significance if the number of HA-VTE events was 50% higher in the COVID cohort (with no missed events in 2019) (OR, 2.4; 95% CI, 1.3-4.7). OR did not change for a 10% to 25% increase in event numbers in COVID only, or if the numbers were increased by a similar proportion across both time periods. In the scenario of 50% missed cases in the COVID cohort, the estimated rate of HA-VTE becomes 7.5 per 1000 discharges.
With a number of patients not yet 90 days postdischarge, we compared historic case numbers with the same follow-up period. Our 2019 data support those that have been previously published11,13 : the majority of postdischarge HA-VTE events occur within the first 6 weeks. Overall incidence, in both the COVID-19 and 2019 medical admissions, is lower than the rate of symptomatic VTE reported in the placebo arm of previous studies investigating extended thromboprophylaxis postmedical admission (1.2% to 1.7%).8,14 However, these studies included events occurring during hospitalization and up to 90 days postdischarge. Our findings suggest that the potentially increased thrombotic risk associated with COVID-19 is limited to the acute illness in those with severe disease requiring critical care admission. Even this association remains controversial, with some arguing that the incidence is as expected for critical care admission if PE localized to segmental/subsegmental vasculature is considered “immunothrombosis” rather than true PE.5,15 Additionally, published rates of VTE in patients with COVID-19 admitted to the hospital and not requiring critical care are comparatively lower, 3.3% to 6.6%, and not dissimilar to rates reported in studies of medical thromboprophylaxis.2,4,10,16 We previously reported a PE rate of 5.4% in patients with COVID-19 from the Denmark Hill site (16.7% in critical care admissions, 3.6% in ward admissions), with 44% of all PE events present on admission.10 Of our postdischarge events, the majority occurred early, with potential for a short course of extended thromboprophylaxis to reduce the incidence by 40% to 50%.8 However, existing data suggest that this approach is associated with a twofold to threefold increase in bleeding and it is therefore not the current standard of care in the United Kingdom.8,14,17 Prescription of extended thromboprophylaxis to all patients with COVID-19 on hospital discharge would add a significant burden to both patients and to the health system with increased costs, without clear evidence for benefit.
Limitations of this study include the lack of systematic follow-up of all patients (for both time periods). Imaging was only performed following physician assessment and suspicion of VTE in patients presenting to the hospital for a second time (or additional times) or following referral from primary care. Therefore, our data will underestimate the total burden of VTE as many events are asymptomatic.18 However, the clinical significance of asymptomatic VTE remains uncertain. In our previously published cohorts from 2010 and 2012, 20% of VTE events were detected incidentally (on imaging performed for other reasons).10 In the COVID cohort, none of the post discharge events were asymptomatic; in the 2019 cohort, there were 4 asymptomatic events (7.1%). Although all patients receive written information regarding VTE that encourages them to seek medical review in the event of suggestive symptomatology, those with COVID-19 may not have sought medical attention for milder symptoms due to fear or isolation. Additionally, patients may have presented again elsewhere for diagnostic investigations. However, due to travel restrictions in place during the lockdown period (23 March 2020 to 1 June 2020), patients most likely would have presented back to their local or a neighboring hospital, where established practices are in place for reciprocal exchange of details regarding potential HA-VTE events. Historically, only a small proportion of HA-VTE (<1% in 2019) are identified from other hospitals. Patients presenting again to other hospitals is likely to have been more common in the 2019 cohort prior to travel restrictions. We performed additional analysis to estimate the effect of having missed 10% to 50% of HA-VTE events and only found a significant increase in VTE risk in the postdischarge COVID cohort if 50% of cases had been missed (with no missed events in 2019). Of note, even in this scenario, the absolute incidence of postdischarge VTE remains low at 0.8%. We do not have data for thromboprophylaxis provision to those without HA-VTE; however, monthly hospital-wide audits suggest that appropriate use is high (94% of 386 medical patients audited in 2019).
Although there are inherent limitations with observational data, our findings provide reassurance that the rate of postdischarge HA-VTE following hospitalization with COVID-19 is low, in contrast to that seen during critical care admission. Our data suggest that empiric postdischarge thromboprophylaxis is not necessary, thereby supporting the American College of Chest Physicians (ACCP) recommendation of not offering postdischarge thromboprophylaxis.7 Further randomized controlled trials are required to evaluate the role of thromboprophylaxis postdischarge.
Data-sharing requests may be e-mailed to the corresponding author, Lara N. Roberts, at lara.roberts@nhs.net. PE data from 1 hospital (Denmark Hill) are presented in greater detail in Whyte et al.10 This includes 2 of the postdischarge PE events presented in this paper.
The online version of this article contains a data supplement.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 USC section 1734.
Acknowledgments
The authors acknowledge Stephanie Rivera for contributing to the collection of 2019 data, and Tatiana Izmaylova for assisting with the discharge data.
Authorship
Contribution: L.N.R. conceived the idea, collected and analyzed the data, and wrote the manuscript; M.B.W., L.G., G.G., and E.G. collected the data; and all authors critically reviewed and approved the final manuscript.
Conflict-of-interest disclosure: L.N.R. has received speaker fees and a travel grant from Bayer, and an investigator-initiated research grant and a travel grant from Sanofi. J.C. has received a travel grant from Mitsubishi Pharma and honoraria from Bayer and Sanofi. C.R. has received unrestricted research grants from Baxter, SOBI, BioMarin. B.V. has received travel grants and event sponsorship from Boehringer-Ingelheim and Bayer. R.K.P. has received speaker fees from Bayer. E.G. has received honoraria from Bayer. R.A. reports grants from Bayer; personal fees from Bayer, Pfizer, Medtronic, and Sanofi; and nonfinancial support from Bayer, Pfizer, and Sanofi. The remaining authors declare no competing financial interests.
Correspondence: Lara N. Roberts, King’s Thrombosis Centre, Department of Haematological Medicine, King’s College Hospital NHS Foundation Trust, Denmark Hill, London, SE5 9RS, United Kingdom; e-mail: lara.roberts@nhs.net.