Abstract
Introduction: Human T-cell lymphotropic virus (HTLV) is a retrovirus that has been associated with adult-T cell leukemia/lymphoma (ATLL) and other inflammatory conditions. Pulmonary involvement has not been widely associated to HTLV infection; however, high rates of imaging abnormalities in patients with and without ATLL have been reported. Okada reported 30%, 69% and 94% of abnormalities in HTLV1 carriers, ATLL and patients that transformed into ATLL. Whether these abnormalities follow a pattern related to each condition individually has not been defined. Hence, we undertook a retrospective study in ATLL and HTLV infected patients to determine the lung abnormalities which could be due to ATLL involvement rather than HTLV infection.
Objectives: To compare the CT pulmonary findings among patients with HTLV infection with and without ATLL diagnosed at Montefiore Medical Center between 2004 and 2017.
Methods: Patients diagnosed with HTLV infection by ICD9 were identified using the software Clinical Looking Glass and those with an available chest CT scan were selected. Data regarding demographics, smoking history, prior pulmonary conditions, HTLV and ATLL-associated characteristics was collected by chart review. CT chest was reviewed by an expert radiologist who was unaware of the patient diagnosis (ATLL versus non-ATLL) and findings were compared among groups. The staging CT scan was used to determine baseline pulmonary findings in patients with ATLL and the first CT chest around HTLV diagnosis was used for HTLV patients.
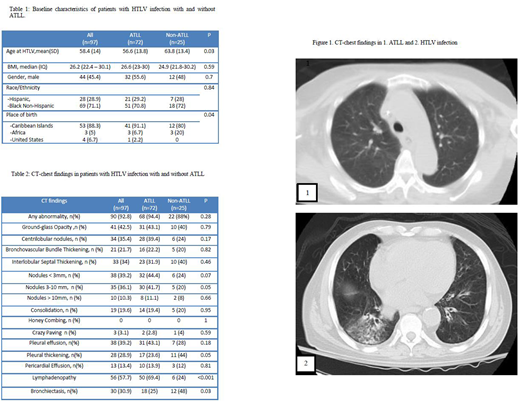
Results: A total of 97 patients (72 with ATLL and 25 with HTLV alone) were identified. Mean age at HTLV diagnosis was 58.4 years (range: 33-88), 54.6% were females, 72.2% were Black Non-Hispanics while 27.8% were Hispanic. 88.3% were from Caribbean origin. Smoking history was similar between ATLL and non-ATLL groups (12% vs 8%, p=0.07) with no cases of prior active TB infection. Abnormal CT chest findings were present in 92.8%, 94.4% and 88% for the total cohort, ATLL and non-ATLL patients.
Among patients with ATLL, 52.1% had acute and 43.7% had lymphomatous types; while only 1.4% and 2.8% had smoldering and chronic type. The most common CT chest findings were lymphadenopathy (50, 69.4%); followed by 3-10 mm nodules (32, 44.4%), ground-glass opacity, pleural effusion (31, 43.1% each), centrilobular nodules (28, 39.4%), thickening of interlobular septum (23, 31.9%) and bronchiectasis (18, 25%). Compared to the acute subtype, patients with lymphomatous subtype had higher rates of lymphadenopathy (83.9% vs 64.9, p=0.07) and lower rates of bronchiectasis (16.1% vs 35.1%, p=0.07).
Among patients with non-ATLL, HTLV infection was diagnosed at an older age (63.8 vs. 56.6 years, p=0.03); HTLV-associated comorbidities were found in 16 cases (64%). Of these, myelopathy was the most frequent (10, 40%), followed by strongyloides (4, 16%). After HTLV diagnosis, CT chest was indicated in 28% patients for otherwise unexplained respiratory symptoms and to evaluate lung nodules or other chest X-ray abnormalities in 24% of cases. Bronchiectasis was the most common finding (12, 48%) followed by pleural thickening (11, 44%), ground-glass opacity and thickening of interlobular septum (10, 40%, each). Persistent abnormalities on follow-up imaging were present in 86.7% of the cases. Among patients with HTLV infection, those with ATLL were more likely to have nodules and lymphadenopathy (41.7% vs 20%, p=0.05 and 69.4% vs 24%, p<0.001, respectively) while bronchiectasis and pleural thickening was more likely in patients without ATLL (48% vs 25%, p=0.03 and 44% vs 23.6%, p=0.05; respectively).
Conclusions: Pulmonary findings are highly prevalent in CT chest of patients with HTLV infection with and without ATLL. Bronchiectasis and pleural thickening was more frequently encountered in non-ATLL patients while lymphadenopathy and nodules were common finding in patients with ATLL. Pulmonary involvement in lymphoma is usually characterized by nodules and lymphadenopathy but patients with ATLL had a higher incidence of findings including ground glass opacities, bronchiectasis and interlobular septal thickening possibly due to their underlying HTLV infection. Based on this data, nodules and lymphadenopathy should be classified as ATLL involvement of the lung while other findings described here could be due to HTLV infection. These findings are important in staging and response criteria for ATLL.
Janakiram:Seatle Genetics: Membership on an entity's Board of Directors or advisory committees.
Author notes
Asterisk with author names denotes non-ASH members.