Abstract
INTRODUCTION: Post-transplant relapse is a major obstacle to successful allogeneic stem cell transplantation (allo-SCT) in hematologic malignancies. Failure to maintain an effective graft versus leukemia effect (GVL) is one mechanism responsible for post-transplant relapse. There is recent interest in PD-1 and other T cell exhaustion markers as therapeutic targets in cancer immunotherapy, however PD-1 inhibitors might induce graft versus host disease (GVHD) after allo-SCT. Therefore, understanding PD-1 kinetics in allo-SCT is needed before using check point inhibitors to prevent or treat relapse. Here we evaluated the relationship between leukemia relapse and the kinetics of T-cell exhaustion markers during the early post-transplant period. We further analyzed the functions of leukemia associated antigen (LAA) specific T-cells from relapsed subjects and sought for the mechanism of post-transplant relapse at a single cell level.
METHODS: Eighty-five patients with various hematologic malignancies received ex-vivo T-cell depleted HLA matched related sibling allo-SCT at a single center between 2006 and 2015. All subjects were treated with a myeloablative conditioning regimen of cyclophosphamide, fludarabine, and total body irradiation with GVHD prophylaxis of low-dose cyclosporine for 21 days. Peripheral blood mononuclear cells (PBMCs) were collected from donors and recipients at 30, 60, and 100 days following transplant and at relapse to characterize regulatory T cells and T cell exhaustion markers by flow cytometry. Samples from six relapsed subjects with acute leukemias were evaluated for 5LAAs (WT1, PRAME, NY-ESO1, MAGEA3, AURAK) by RT-PCR and LAA specific T-cells by Elispot and flow cytometry. LAA specific T cells in one subject were further analyzed for single cell RNAseq.
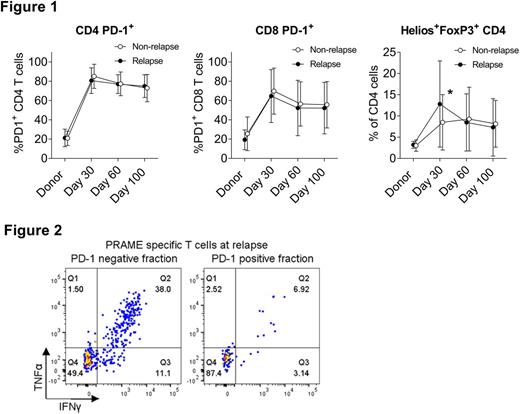
RESULTS: At a median follow up of 3.4 years, 35 patients had relapsed with a 5-year cumulative relapse incidence of 44% at a median time of 226 days. Post-relapse survival was poor among subjects relapsing before 180 days post allo-SCT (median post-relapse survival 126 days vs. 329 days for patients relapsing after 180 days; P=0.004). In the early post-transplant period, PD-1 expression in CD4 and CD8 T-cells was significantly and comparably elevated in both relapsed and non-relapsed cohorts as compared to donors. No association was observed between relapse incidence and pattern of PD-1 expression. In contrast, Helios+Tregs frequency was significantly higher in the relapsed cohort at day 30 (Figure 1). Among six relapsed subjects, at least one LAA was detected in PBMCs before and after relapse. LAA specific T-cells were observed in four subjects, however all samples eventually expressed new LAA different from the ones targeted by their own LAA specific T-cells suggesting immunological escape of leukemic blasts. Of note, LAA specific T-cells were predominantly enriched in the PD-1 negative fraction (Figure 2). Single cell analysis in one patient revealed a distinct cluster with the other exhaustion marker, LAG3 in PRAME specific T-cells in comparison to CMV specific T-cells.
CONCLUSION: Our findings contradict the prevailing view that PD-1+ T cell exhaustion is a prominent feature of leukemic relapse after SCT. We found that PD-1 was overexpressed in T-cells during the early post-transplant period in all patients and PD-1 expression patterns did not identify patients destined to relapse. Furthermore, the leukemia antigen specific T-cells did not overexpress PD-1, instead single cell analysis revealed LAG3 overexpression in one patient at relapse. These findings do not support PD-1 is the predominate marker for leukemia specific T cell exhaustion in relapsing patients but point to other exhaustion markers or suppressor Treg cells as causes of relapse. Further studies are required to identify predictive biomarkers for check point inhibitors in hematologic malignancies and the patterns of LAA expression in residual disease following allo-SCT.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.