Abstract
Background: Analyses in lower risk myelodysplastic syndromes (MDS) suggest inferior survival in patients (pts) with transfusional iron overload (IOL). Some studies suggest an increased incidence of infections and infection related mortality in transfused MDS pts. Reducing IOL with iron chelation therapy (ICT) appears to give clinical benefit. The literature suggests that IOL can predispose to bacterial, fungal and viral infections, as organisms use iron for metabolism and cell division, and IOL can adversely affect neutrophil function. There are no clinical studies examining infection risk in MDS pts with IOL in the non-stem cell transplant (SCT) setting, and whether this risk can be attenuated with ICT.
Methods: We performed a retrospective analysis of pts with a bone marrow biopsy confirmed diagnosis of lower International Prognostic Scoring System (IPSS) risk MDS receiving red blood cell (RBC) transfusions. Pts were identified from the clinical database and charts reviewed. Clinical data extracted included baseline characteristics, serum ferritin level (SF), treatment, and infectious episodes requiring antibiotics, antifungal or antiviral medications. Statistical analyses were performed using SPSS for Windows, version 24.
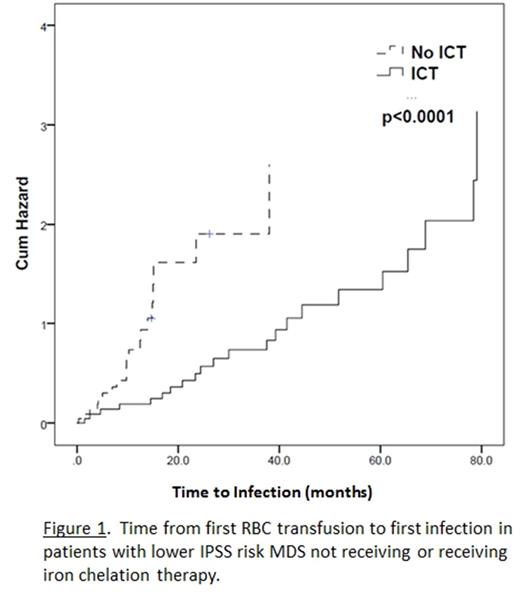
Results: Of 182 transfused MDS pts, 138 were lower IPSS risk. 44 pts were excluded for: not transfused as lower risk, n=19; higher IPSS risk, or received hypomethylating agent or SCT, n=13; and inadequate information, n=12. The median (range) age at first RBC transfusion was 72.5 (31-93) years and 78 (57%) pts were male. 59 pts received ICT: deferasirox (DFX), n=45 (76.3%); deferoxamine (DFO), n=13 (22.0%); and deferiprone, n=1 (1.7%); and 79 did not receive ICT. Median (range) time from 1st RBC transfusion to ICT was 22.5 (1.4-209) months and duration of ICT 13 (1-75) months. Clinical factors differing between ICT and non-ICT pts, respectively, were (median [range]): age at 1st RBC transfusion, 67 (31-88) and 75 (43-93) years; number of RBC units (U) transfused while lower risk, 76 (10-675) and 24 (2-200); number of RBCU/4 weeks, 2.2 (0.5-9.1) and 2.0 (0.1-5.4); SF 914 (49-15608) and 266 (12-5009) ng/mL; and other treatments received, 18 (30.5%) and 5 (6.3%); p</=0.04 for all. Factors not differing between groups were: gender; French American British or World Health Organization MDS diagnosis; marrow blast count; IPSS or IPSSR cytogenetic risk; IPSS or IPSSR risk; neutrophil count at first RBC transfusion or at first infection; and causes of death, p=NS for all. Infections included: bacterial, n=88; viral; fungal; and mycobacterial; n=2 each. In ICT and non-ICT pts, respectively, infections while lower IPSS risk were (number [%]): pts, 23 (40.0%) and 22 (27.8%); episodes (median [range]), 2 (1-6) and 2 (1-5); hospitalizations, 16 (27.1%) and 8 (10.1%); and infectious deaths, 0 (0%) and 1 (1.3%), p=NS for all. In ICT pts, infections occurred pre-ICT in 9 (15.3%); on DFX, n=10 (22.2%), and on DFO, n=4 (30.8%), p<0.0001. Median overall survival (OS) from 1st RBC transfusion while lower IPSS risk was not reached at 105, and 50.1 months for ICT and non-ICT pts, respectively, p=0.01. ICT remained significant for OS in a multivariate analysis (MVA) including: ICT; IPSS cytogenetic risk; and hospitalization for infection; (all p</=0.06 in univariate analysis), p=0.003, hazard ratio (HR) 0.3, 95% confidence intervals (CI) 0.2-0.7, and lost significance when number of RBCU received (p<0.0001) was added to the MVA. However, OS was significantly superior for ICT pts receiving >20 and >50 RBCU (p=0.02, and <0.0001, respectively). Median time to first infection (TTI) was 27 and 7.8 months for ICT and non-ICT pts, respectively, p<0.0001 (Figure 1). ICT remained significant for TTI in an MVA including: age; IPSS cytogenetic risk; marrow blast count; and number of RBCU received (p=0.03, HR 0.3, 95% CI 0.09-0.9). For TTI, marrow blast count was also significant in the MVA (p=0.04). TTI remained significantly longer for ICT pts with blast count <5% (p=0.004).
Conclusions: In this retrospective, non-controlled analysis, for lower IPSS risk MDS patients receiving RBC transfusions, receiving iron chelation therapy was associated with superior overall survival. Though number and type of infections were similar between groups and despite similar neutrophil counts, time to first infection was significantly longer in ICT patients. These results should be confirmed in larger, prospective analyses.
Leitch: Celgene: Honoraria, Membership on an entity's Board of Directors or advisory committees, Research Funding; Novartis: Honoraria, Membership on an entity's Board of Directors or advisory committees, Research Funding; Exjade: Speakers Bureau; Abbvie: Research Funding; Alexion: Honoraria, Membership on an entity's Board of Directors or advisory committees, Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.