In this issue of Blood, Zerra et al demonstrate the involvement of splenic marginal zone (MZ) B cells in initiating immune responses of naive hemophilia A mice to infused factor VIII (FVIII).1
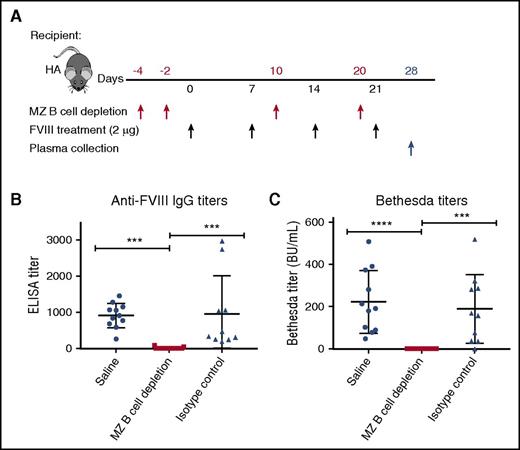
Depletion of splenic MZ B cells prevents development of anti-FVIII antibodies. (A) FVIII-KO mice were treated with MZ B-cell–depleting antibodies, an isotype control antibody, or saline (red arrows) beginning 4 days before initial exposures to intermediate doses of FVIII (black arrows). Plasma was collected 1 week after the fourth weekly FVIII infusion (blue arrow) and analyzed by enzyme-linked immunosorbent assay (ELISA) (B) and Bethesda assay (C) to determine total and inhibitory anti-FVIII antibody titers, respectively. MZ B-cell depletion completely ablated the primed anti-FVIII antibody response, indicating a key role for MZ B cells in initiating the naive anti-FVIII immune response. Mice receiving subsequent FVIII injections following a delay to allow MZ B-cell reconstitution developed anti-FVIII antibodies (not depicted here), indicating that MZ B-cell depletion alone was insufficient to achieve peripheral tolerance to FVIII. BU, Bethesda units. ***P < .0002, ****P < .0001, 1-way analysis of variance, post hoc Tukey test. This figure has been adapted from Figure 3A-C in the article by Zerra et al that begins on page 2559.
Depletion of splenic MZ B cells prevents development of anti-FVIII antibodies. (A) FVIII-KO mice were treated with MZ B-cell–depleting antibodies, an isotype control antibody, or saline (red arrows) beginning 4 days before initial exposures to intermediate doses of FVIII (black arrows). Plasma was collected 1 week after the fourth weekly FVIII infusion (blue arrow) and analyzed by enzyme-linked immunosorbent assay (ELISA) (B) and Bethesda assay (C) to determine total and inhibitory anti-FVIII antibody titers, respectively. MZ B-cell depletion completely ablated the primed anti-FVIII antibody response, indicating a key role for MZ B cells in initiating the naive anti-FVIII immune response. Mice receiving subsequent FVIII injections following a delay to allow MZ B-cell reconstitution developed anti-FVIII antibodies (not depicted here), indicating that MZ B-cell depletion alone was insufficient to achieve peripheral tolerance to FVIII. BU, Bethesda units. ***P < .0002, ****P < .0001, 1-way analysis of variance, post hoc Tukey test. This figure has been adapted from Figure 3A-C in the article by Zerra et al that begins on page 2559.
The development of neutralizing anti-FVIII antibodies, termed inhibitors, is a serious unintended consequence of FVIII replacement therapy that affects up to one-third of severe hemophilia A (HA) patients and a smaller but still significant number of patients with mild to moderate HA. Inhibitors are likeliest to appear after the first 10 to 15 FVIII infusions, although they may occur later, for example, following surgery, or in concert with other inflammatory conditions. The reasons why some patients develop this deleterious immune response while others achieve peripheral tolerance to FVIII are unknown, and this conundrum is an area of active research. The current approach to eradicate inhibitors is immune tolerance induction via intensive FVIII therapy, which succeeds in ∼70% of cases. Alternatively, inhibitors may be avoided/bypassed by infusing patients with a plasma-derived procoagulant complex or emicizumab, a recently developed bispecific antibody that mimics FVIII cofactor activity by localizing and orienting components of the intrinsic tenase complex to increase its catalytic efficiency.2 Zerra et al now introduce a novel approach to explore anti-FVIII immune responses by manipulating cellular components of the spleen marginal zone (MZ) in FVIII-knockout (FVIII-KO) mice.
Blood-borne antigens are filtered by the spleen, which can initiate immune responses shortly after antigen uptake.3 Several studies have demonstrated FVIII accumulation in the marginal sinus of the spleen after its administration to FVIII-deficient4 or von Willebrand factor (VWF)–deficient5 mice, and splenectomy of FVIII-KO mice prior to FVIII exposure significantly attenuated the anti-FVIII antibody response.4 Interestingly, VWF, which functions as a chaperone for FVIII in the circulation, localizes to the splenic red pulp following uptake, whereas FVIII preferentially locates to the MZ, where it colocalizes with MZ antigen-presenting cells. Depletion of macrophages and CD11c+CD8α− dendritic cells attenuated the naive anti-FVIII antibody response in FVIII-KO mice,4 indicating important roles for these antigen-presenting cells in inhibitor formation. The murine spleen MZ is a distinct microenvironment surrounding the white pulp, containing resident dendritic cells, MZ and metallophilic macrophages, and MZ B cells. In addition to these unique resident cells, circulating cells, including dendritic cells, macrophages, and T cells, pass through the MZ as part of ongoing immune surveillance for pathogens. All cells migrating to the splenic white pulp must pass through the MZ.
MZ B cells have properties of both innate and adaptive immune cells, and unlike follicular (FO) B cells, they can potently activate naive CD4+ T cells.6 They may respond to antigens on macrophages, dendritic cells, or neutrophils by differentiating into immunoglobulin M (IgM)–producing plasma cells or, alternatively, into antigen-presenting cells. MZ B cells can also produce lower levels of IgG and IgA. They may act as “shuttles” by transferring antigens to follicular dendritic cells. In mice, MZ B-cell retention requires binding of integrins αLβ2 and α4β1 to the adhesion molecules ICAM1 and VCAM1, respectively. Many murine MZ B cells express both polyreactive B-cell receptors capable of binding multiple microbial determinants and Toll-like receptors; dual engagement of these receptors stimulates low-affinity antibody generation in advance of specific, high-affinity antibodies subsequently produced by follicular and extrafollicular pathways. Murine MZ B cells also recognize complement opsonins and microbial lipids, as well as protein antigens, via surface major histocompatibility complex class II, CD80, and CD86.
In the present study, FVIII-KO mice received FVIII injections in the presence of polyinosinic:polycytidylic acid (PIC), to induce a proinflammatory state, or in its absence. As expected, anti-FVIII antibody titers in mice exposed to PIC were higher. Another group of FVIII-KO mice were given serial intraperitoneal injections of antibodies specific for integrin proteins αL and α4, thereby releasing the MZ B cells from the MZ, prior to priming with FVIII. This MZ B-cell depletion significantly decreased initial anti-FVIII IgG titers and Bethesda (inhibitory antibody) titers (see figure), as well as subsequently boosted total anti-FVIII IgG and Bethesda titers. After allowing the MZ B cells to repopulate and rechallenging with FVIII, the mice developed inhibitors, although titers were lower than those in control mice with a boosted anti-FVIII response. This indicated that MZ B-cell depletion prevented initial inhibitor development but did not induce peripheral tolerance to FVIII. However, these results, together with the observed colocalization of FVIII with MZ B cells, suggest an important role for MZ B cells as initiators of the naive anti-FVIII immune response.
Minor caveats include the possibility that the antibodies used to block integrin binding also interfered with other relevant binding interactions and/or cellular signaling pathways. Also, the depletion of one cell type may well affect interactions and phenotypes of neighboring cells, complicating interpretations. The respective roles in inhibitor development of MZ B cells, dendritic cells, macrophages, and other cells, including metallophilic macrophages (which also colocalize with FVIII in the MZ but are murine specific), are active areas of research. It is possible that FVIII is transported to follicular dendritic cells by both macrophages and MZ B cells, and nonexclusive mechanisms of antigen shuttling and presentation may prevail according to the animal’s immune status and the MZ microenvironment.
It is intriguing to compare the present results with an earlier study by Zhang et al in which follicular B cells or follicular and MZ B cells were depleted after FVIII priming; depletion of follicular B cells alone followed by intensive FVIII administration increased splenic regulatory T-cell levels, decreased subsequent inhibitor titers, and upregulated B7 costimulatory molecules on MZ B cells, suggesting MZ B cells may play a tolerogenic role under some conditions.7
Overall, this report by Zerra and colleagues highlights the importance of the splenic MZ in initiating anti-FVIII immune responses and focuses attention on the roles of splenic MZ B cells, which are fascinating, polyfunctional cells bridging innate and adaptive immunity. Further studies of FVIII uptake, processing, and presentation in both naive and antigen-experienced FVIII-KO mice are warranted, along with complementary studies of accessible cells from patient blood samples. The roles of VWF in FVIII immunogenicity,8 and possible differences in presentation/processing of new FVIII products (eg, proteins modified to extend their half-lives) are under study in multiple laboratories. Additional manipulation of the naive anti-FVIII immune response, building on results of the present study, seems a particularly promising approach to identify novel therapeutic targets that could prevent inhibitor development.
Conflict-of-interest disclosure: The author reports no competing financial interests. The opinions or assertions contained herein are the private ones of the author and are not to be construed as official or reflecting the views of the Department of Defense or the Uniformed Services University of the Health Sciences.