In this issue of Blood, Guo et al show that interleukin-4 (IL-4) upregulates surface immunoglobulin M (IgM) expression and B-cell receptor (BCR) signaling capacity of chronic lymphocytic leukemia (CLL) cells, providing an explanation of how anergic CLL cells from the peripheral blood become signal competent when they enter the lymph nodes.1
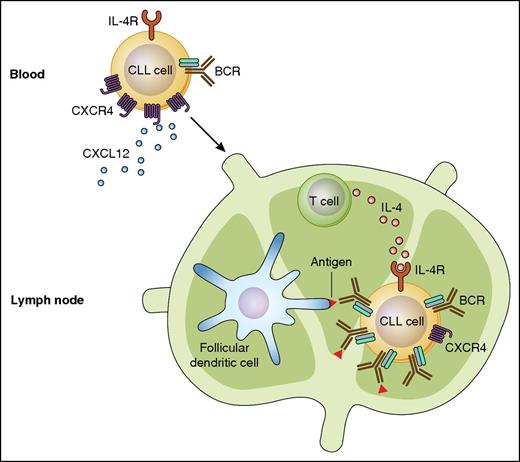
Regulation of BCR expression on CLL cells by IL-4. CLL cells in peripheral blood have downmodulated BCRs, presumably to prevent inappropriate activation by antigen in the absence of co-stimulatory signals. In response to CXCL12 and other chemokines, these cells migrate to the lymph nodes, where locally secreted IL-4 induces CD79b and increases translocation of the BCR complex to the leukemic cell surface. This mechanism increases the likelihood that CLL cells encounter and interact with antigen in the appropriate context. IL-4R, IL-4 receptor. Professional illustration by Patrick Lane, ScEYEnce Studios.
Regulation of BCR expression on CLL cells by IL-4. CLL cells in peripheral blood have downmodulated BCRs, presumably to prevent inappropriate activation by antigen in the absence of co-stimulatory signals. In response to CXCL12 and other chemokines, these cells migrate to the lymph nodes, where locally secreted IL-4 induces CD79b and increases translocation of the BCR complex to the leukemic cell surface. This mechanism increases the likelihood that CLL cells encounter and interact with antigen in the appropriate context. IL-4R, IL-4 receptor. Professional illustration by Patrick Lane, ScEYEnce Studios.
The recent approval of the Bruton tyrosine kinase (BTK) inhibitor ibrutinib and the phosphatidylinositol 3-kinase δ (PI3Kδ) inhibitor idelalisib represent major breakthroughs in the treatment of CLL. Although these drugs can inhibit various signaling pathways, they are believed to function primarily by inhibiting signals that the leukemic cells receive through their BCRs.2 This mechanism of action is supported by numerous lines of evidence supporting a major role for the BCR pathway in the development and progression of CLL, including the expression of BCRs with particular structural and antigen-binding properties, the expression of high levels of BCR-target genes in lymph node-derived CLL cells, and the significant association between clinical course and certain BCR-related features, such as the mutational status of the immunoglobulin heavy chain variable (IGHV) region genes.3 This evidence, however, is difficult to reconcile with the relatively impaired capacity of CLL cells in the peripheral blood to respond to BCR engagement. Reduced BCR signaling capacity is a general feature of CLL, but is particularly prominent in the CLL subset with IGHV-mutated genes (M-CLL), where the malignant B cells are often completely anergic.4
In the article published in this issue of Blood, Guo et al investigate the mechanism(s) responsible for the impaired BCR signaling capacity of freshly isolated peripheral blood CLL cells. They show that the reduced signaling capacity of the leukemic cells is at least in part caused by deficient expression of the CD79b component of the BCR, which is expressed at much lower levels in CLL than normal peripheral blood B cells. The relative deficiency of CD79b leads to inefficient assembly of the BCR complex and results in reduced translocation of the BCR to the leukemic cell surface. Importantly, Guo et al show that CD79b expression and BCR assembly can be rescued by IL-4, which is a cytokine that is abundantly produced by T cells of patients with CLL.5 T cells interact with CLL cells in the lymph node proliferation centers,6 suggesting that BCR expression and signaling capacity could be restored in CLL cells in lymph nodes by locally produced IL-4 (see figure).
Although the above described mechanism needs to be further validated by analyzing paired peripheral blood and lymph node CLL samples, it is supported by the observation of the authors that recently egressed CLL cells express higher levels of surface IgM than CLL cells that have migrated from the lymph nodes into the peripheral blood at an earlier time point. A prominent feature of the latter cells are the high levels of the chemokine receptor CXCR4,7 which drives the migration of CLL cells in response to the chemokine CXCL12. Interestingly, another study that was recently published in Blood reported that CXCR4 surface expression is downmodulated on CLL cells by IL-4.8 This suggests that IL-4 could promote interaction of CLL cells with antigen by 2 mechanisms, ie, by upregulating CD79b and thus increasing surface IgM expression and BCR signaling capacity, and by downmodulating CXCR4 and promoting leukemic cell retention within the lymph node microenvironment.
Another important finding of the Guo et al study is the observation that IL-4 restores to a much greater extent surface IgM expression and BCR signaling capacity in the CLL subset with IGHV-unmutated genes (U-CLL), compared with M-CLL cells. Considering that the capacity to respond to stimulation with external ligand is directly correlated with more aggressive disease both in human CLL9 and in the Eμ-TCL1 murine model,10 this observation could provide additional insight into the mechanisms responsible for the more aggressive behavior of U-CLL than M-CLL. The reason for the greater capacity of U-CLL than M-CLL cells to upregulate CD79b in response to IL-4 is unclear at present and will require further study.
In conclusion, the study by Guo et al provides an explanation on how anergic CLL cells can be activated and induced to expand by antigen stimulation, a question that has puzzled CLL investigators for many years. The finding that surface IgM expression and BCR signaling capacity can be restored in CLL cells by IL-4 underscores the importance of signals from the microenvironment in determining the behavior of the leukemic cells, and further points to the BCR pathway as the primary target of BTK and PI3Kδ inhibitors in CLL.
Conflict-of-interest disclosure: The author declares no competing financial interests.