Abstract
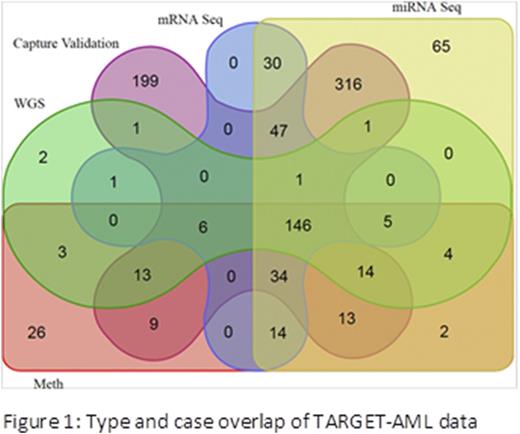
The age distribution of acute myeloid leukemia is unusual among malignancies, with onset spanning from early infancy until past the 9th decade. Despite similar histology, cytogenetic abnormalities and recent identification of somatic mutations (e.g., DNMT3A mutations) have highlighted differences in the events driving adult compared to childhood de novo AML. However, the full extent of these differences remains unknown and is likely to have relevance to treatment approaches. The TARGET AML initiative is an effort of the Children's Oncology Group (COG) and the National Cancer Institute to comprehensively characterize the molecular abnormalities of pediatric AML. The dataset comprises 1) whole genome sequencing (WGS) of AML and matched remission bone marrow in 197 cases, 2) mRNA transcriptome sequencing of 284 cases, 3) miRNA sequencing of 692 cases, 4) methylation array data on 289 cases, and 5) targeted capture sequencing of 174 candidate genes identified from WGS in 800 diagnostic samples, including 182 with WGS (Figure 1). The majority of patients (93%) studied were uniformly treated on COG study AAML0531 or its pilot safety precursor study, AAML03P1. Relapsed specimen data (not shown) are available for a subset of these cases. All patient samples were obtained by written consent upon enrollment in the clinical trial.
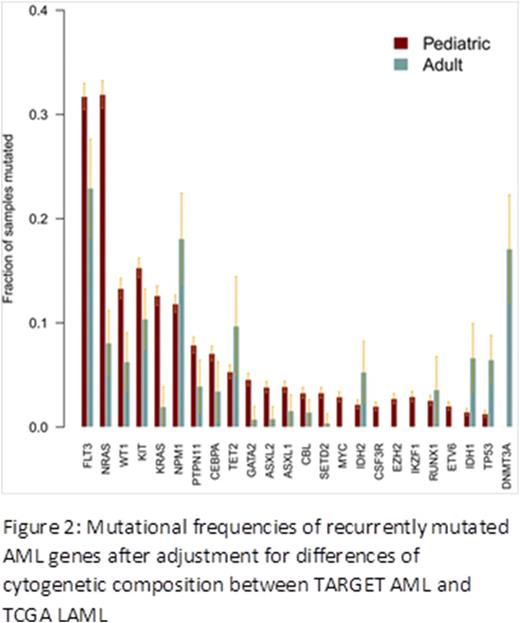
Consistent with adult studies, we identified a relatively low mutational burden, with 2206 somatic tier 1 mutations resulting in a coding change in 1682 genes (median 6 per patient) from the WGS discovery data. We successfully verified 70-90% of variant calls by secondary methods. Also as with adult data, there were relatively few recurrently mutated genes, with fewer than 40 genes altered in >2% of samples. However, there were marked differences in somatic mutation frequencies in comparison to adult TCGA data, both by raw frequency and after adjustment for cytogenetic subtypes present among the two cohorts (Figure 2). Mutations in TP53, NPM1, IDH1, IDH2, TET2 and DNMT3A are more frequent in adult compared to pediatric disease; in contrast, mutations in NRAS, KRAS, WT1, FLT3, PTPN11, GATA2, ASXL2, MYC, SETD2, EZH2 and IKZF1 appear more common in pediatric AML. Mutations of several genes, including CEBPA, ASXL2 and KRAS are not only more common in pediatric AML, they show peak prevalence within specific pediatric age groups. In addition, several genes, including FLT3, WT1, and KIT show significant differences in mutational hotspots compared to adults.
Pediatric-adult differences in AML were not limited to somatic gene mutations, but extended to focal and chromosomal copy number alterations (CNA), translocations, miRNA expression, and methylation-induced gene silencing. We identified recurrent focal CNAs in multiple regions not reported in adult AML including 15 heterozygous focal deletions impacting ELF1, an ETS-family transcriptional regulator of hematopoiesis and leukemia driver as well as deletions of the splicing regulator MBNL1 in 10 cases, 8 of which co-occurred with focal deletions of the hematopoietic transcriptional regulator, ZEB2. De novo assembly of mRNA sequencing data identified fusion transcripts in 63% of cases compared to 45% of TCGA LAML. In addition to cytogenetically evident fusions with well-described enrichment for MLL translocations in pediatrics, we identified 29 diagnostic samples (10%) with nucleoporin family fusions (NUP98 with NSD1, KDM5A, PHF23, HOXD13, HMGB3, BRWD3, and CLINT; NUP214 with DEK and SET), CBFA2T3-GLIS2 fusions in 5, and rare fusions of ETS transcription factor genes (FUS-FEV, ETV6-INO8D). Comparison of miRNA expression patterns between adult and pediatric specimens similarly showed marked differences in expression of key regulatory miRNAs including let-7 family members. Finally, analysis of mRNA expression and DNA methylation for the identification of epigenetically silenced genes suggested that, although specific events favor silencing in adults or children, an overall pattern of gene silencing was more prevalent in pediatric compared to adult cases.
This work extends our understanding of the heterogeneity of AML, demonstrates fundamental differences in the biology of pediatric- and adult-onset disease, and suggests important age-related differences within "pediatric" AML. This rich dataset should provide a foundation for the establishment of biologically-guided treatment in children with AML.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.