Abstract
Background: Venous thromboembolism (VTE) is an uncommon but clinically significant postoperative complication in children. Incidence of VTE in pediatric patients ranges from 34-58 per 10,000 hospitalized children1. Due to rarity of these events, there is limited information about the factors predisposing children to VTE after surgery. We queried a national surgical database to identify risks and outcomes associated with VTE in pediatric surgical patients.
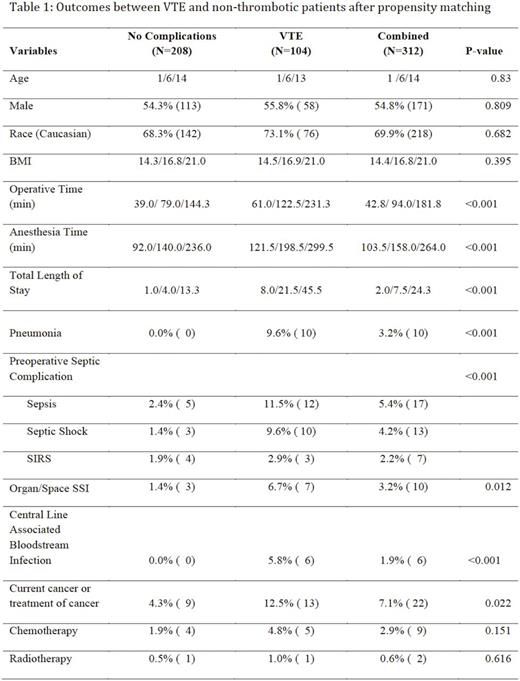
Methods: The National Surgical Quality Improvement Program-Pediatric (NSQIP) is a prospectively collected database that records pediatric surgical information, surgical approaches, and 30 day patient outcomes. The database was queried for the years 2012-2013 to identify pediatric patients (age < 18) who had received surgical intervention and were diagnosed with postoperative VTE. Because of their separate coding in NSQIP, we defined VTE as including venous thromboembolism, or pulmonary embolism (PE) diagnosed radiographically within 30 days of operation. To reduce non-random differences between patients we used propensity scores based on age, sex, race, BMI, and ASA classification to match patients in a 1:2 ratio using the nearest neighbor method. Using univariate and multivariate analysis, we identified preoperative risk factors associated with VTE.
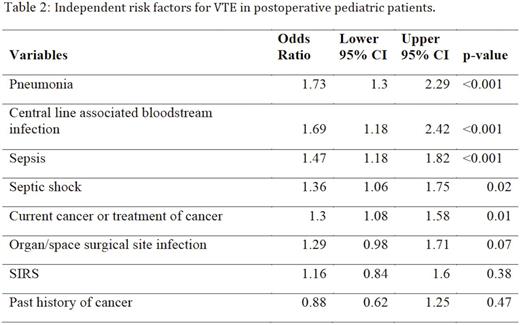
Results: In total, 130 patients were identified who developed VTE postoperatively (VTE n=122, PE n=7, BOTH PE + VTE n= 1) from this database of 114,395 patients. There were 104 patients with VTE that also had complete entries and were subsequently analyzed in this study. Surgical specialties treating patients in this analysis included cardiothoracic surgery, general surgery, neurosurgery, orthopedic surgery, otolaryngology, plastic surgery, and urology. Eighty-one unique operative CPT codes were identified for patients with VTE. Patients who developed VTE had increased operative time, anesthesia time, and total length of stay (all p < 0.001). Multivariate analysis demonstrated that pneumonia (odds ratio [OR] 1.73, 95% confidence interval [CI] 1.3 - 2.29), Central Line Associated Bloodstream Infection (CLABSI) (OR 1.69, 95% CI 1.18 - 2.42), sepsis (OR 1.47, 95% CI 1.18 - 1.82), septic shock (OR 1.36, 95% CI 1.06 - 1.75), and current solid or hematologic malignancy or active treatment of malignancy (OR 1.30, 95% CI 1.08 - 1.58) were all statistically significant risk factors associated with development of VTE (all p < 0.05).
Conclusions: Postoperative VTE risk is significantly increased in children with malignancy or severe infections. Further research is needed to understand the mechanism between malignancy, systemic inflammation, and VTE risk in children. These findings may help to identify patients in need of prophylactic treatment in order to reduce postoperative thrombotic risk in pediatric patients.
References:
1. Raffini L, Huang YS, Witmer C, Feudtner C. Dramatic increase in venous thromboembolism in children's hospitals in the United States from 2001 to 2007. Pediatrics. 2009;124(4):1001-1008.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.