Abstract
Introduction: Sickle cell disease (SCD) is a chronic illness associated with frequent medical complications and hospitalizations. Importantly, approximately ninety percent of hospitalizations are for pain events, and 30-day re-hospitalization rates are alarmingly high. Factors influencing the high rates are poorly understood; however, close follow-up and continued titration of pain medications have been shown to decrease re-hospitalization rates. Mobile technology has become an increasingly integral part of health care management. We have recently developed SMART (Sickle cell Mobile Application to Record symptoms via Technology) to assist with documentation of pain and interventions. We propose using this current mobile technology as a tool for both patients and providers to monitorand manage symptoms and health interventions. We hypothesize that this technology will lead to an increase in follow up, a significant decrease in readmission rates, as well as overall disease burden.
Methods: We randomized SCD patients who presented to the day hospital for pain control to either standard of care or an iPad with SMART. Patients were enrolled upon discharge from the day hospital and expected to return for a visit at 12 and 30 days after hospitalization. They were followed for a total of 30 days to determine re-utilization rates. Re-utilization was defined as a return for pain management to the day hospital, emergency department (ED), or admission to the hospital. Patients with more than 10 acute care visits in the past 12 months or who were on chronic transfusions were excluded.
Standard of care (SOC) included a review of instructions, discharge medications, upcoming appointments and phone numbers for contact. SMART was programmed with the patient's scheduled medications, upcoming appointments and allowed patients and the medical team to communicate via text. Patients were provided a reminder through the app to record their symptoms and interventions (medication or non-pharmacologic) twice daily. The medical team reviewed symptoms recorded by patients at least once daily and texted patients who were indicating significant changes in pain.
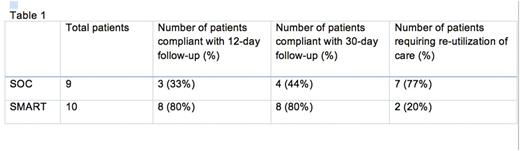
Results: We enrolled 19 SCD patients and randomized 10 to SMART and 9 to SOC (52% male, mean age 31.2 ± 6.6 years). Patients using SMART were more likely to return for their scheduled follow-up visit at 12 days (80% vs. 33%) and 30 days (80% vs. 44%). Thirty-day re-utilization of care was lower for patients using SMART compared to patients receiving SOC (20% vs. 77%, see Table 1). Furthermore, re-utilization for patients using SMART was limited to 2 visits to the day hospital, which occurred 10 and 24 days post discharge. This is in contrast to 8 visits to the ED and 3 to the day hospital among 7 of the 9 patients receiving SOC, with re-utilization occurring a median of 2 days post discharge (range 1-23).
Of the patients using SMART, one patient did not make any entries into the application, while the other 9 patients made almost 1 entry per day for 30 days (median entries 28.9, range 5-107). The medical team texted all patients with SMART (range 2-19 times over 30 days); 60% returned texts to the medical team (range 2-11 times over 30 days). Interestingly, the two patients with SMART who returned within 30 days to the day hospital for further pain treatment had not returned any texts to the medical team.
Conclusion: Our pilot study used an innovative mobile application to improve care for SCD patients who were discharged following day hospital treatment for pain crisis. Patients using SMART were more likely to return for their scheduled follow-up appointments. In addition, 30-day re-utilization of care was much higher for patients receiving SOC than SMART and was similar to previously observed institutional re-utilization rates. In contrast, only 20% of patients given SMART returned for re-utilization of care within 30 days, and they were the patients who did not use the texts for communication. We plan to expand the use of SMART to improve decision-making by medical providers through access to symptoms recorded by patients following discharge and, ultimately, to decrease re-utilization of care.
Jonassaint:Sicklesoft: Other: officer of Sicklesoft. Shah:Novartis: Speakers Bureau.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal