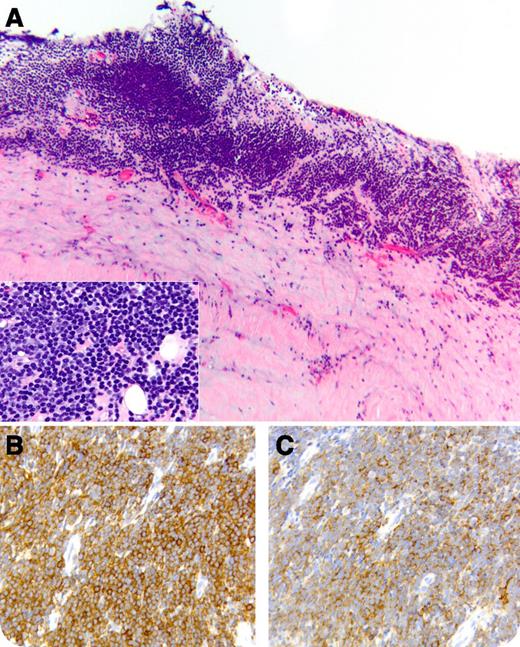
A 71-year-old male presented with fatigue, progressive dyspnea, weight gain, and anasarca. The complete blood count showed a white blood cell count of 7,000/μL with a normal differential count and no cytopenias. Imaging studies revealed bilateral pleural effusions, pericardial effusion with thickened pericardium, and constrictive heart physiology, ascites, and scattered lymphadenopathy without pathological enlargement. Fluid obtained during thoracentesis, pericardiocentesis, and paracentesis was negative for malignancy by microscopic examination (immunophenotyping was not performed). Following rapid recurrence of anasarca, the patient underwent a total pericardiectomy. Examination of pericardial tissue showed fibrous pericarditis and an extensive bandlike infiltrate consisting of small lymphocytes with round nuclei and scant cytoplasm (panel A and inset). Cells expressed CD5 (panel B), CD19, CD20 (weak) (panel C), and CD23. The bone marrow biopsy showed a small population of monoclonal B cells, consistent with chronic lymphocytic leukemia (CLL)/small lymphocytic lymphoma (SLL). Despite receiving prednisone, the patient had recurrent pleural effusions, immunophenotypically positive for CLL. He received therapy with fludarabine and rituximab; however, he succumbed to infectious complications. A postmortem examination revealed no residual CLL.
Pericardial invasion is an extremely unusual initial presentation for CLL/SLL. Although a “passenger effect” cannot be ruled out, the absence of a concurrent inflammatory process speaks in favor of pathological leukemic involvement, which needs to be included in the differential diagnosis of lymphocytic infiltrates of the serosal surfaces.
A 71-year-old male presented with fatigue, progressive dyspnea, weight gain, and anasarca. The complete blood count showed a white blood cell count of 7,000/μL with a normal differential count and no cytopenias. Imaging studies revealed bilateral pleural effusions, pericardial effusion with thickened pericardium, and constrictive heart physiology, ascites, and scattered lymphadenopathy without pathological enlargement. Fluid obtained during thoracentesis, pericardiocentesis, and paracentesis was negative for malignancy by microscopic examination (immunophenotyping was not performed). Following rapid recurrence of anasarca, the patient underwent a total pericardiectomy. Examination of pericardial tissue showed fibrous pericarditis and an extensive bandlike infiltrate consisting of small lymphocytes with round nuclei and scant cytoplasm (panel A and inset). Cells expressed CD5 (panel B), CD19, CD20 (weak) (panel C), and CD23. The bone marrow biopsy showed a small population of monoclonal B cells, consistent with chronic lymphocytic leukemia (CLL)/small lymphocytic lymphoma (SLL). Despite receiving prednisone, the patient had recurrent pleural effusions, immunophenotypically positive for CLL. He received therapy with fludarabine and rituximab; however, he succumbed to infectious complications. A postmortem examination revealed no residual CLL.
Pericardial invasion is an extremely unusual initial presentation for CLL/SLL. Although a “passenger effect” cannot be ruled out, the absence of a concurrent inflammatory process speaks in favor of pathological leukemic involvement, which needs to be included in the differential diagnosis of lymphocytic infiltrates of the serosal surfaces.
For additional images, visit the ASH IMAGE BANK, a reference and teaching tool that is continually updated with new atlas and case study images. For more information visit http://imagebank.hematology.org.