Abstract
Background: c-Myc is one of the most frequently altered genes across a vast array of human cancers. Overexpression of c-Myc is observed in up to 30% of cases of diffuse large B-cell lymphoma (DLBCL), the most common type of aggressive lymphoma. Although DLBCL can be cured in 60-70% patients, a substantial minority of patients with DLBCL still die from their lymphoma. There is emerging evidence that c-Myc expression is an adverse risk factor independent of the cell-of-origin classification. To date no drugs that directly target c-Myc have been approved for the treatment of any cancer. In fact, since c-Myc is involved in many normal cellular functions, direct c-Myc inhibitors may be associated with significant toxicity. The goal of our study is to develop novel strategies targeting c-Myc that will have an improved therapeutic index. The c-Myc protein has a very short half-life of less than 30 minutes, and its translation is highly dependent on the eukaryotic initiation factor 4F (eIF4F). eIF4F is activated by the mammalian target of rapamycin (mTOR), which is regulated not only by the PI3K-AKT pathway but also the proteasome pathway. These observations led us to hypothesize that if the proteasome and PI3K pathways cooperate in the activation of mTOR and its downstream target eIF4F, then combinations of proteasome and PI3K inhibitors should potently suppress eIF4F dependent translation of c-Myc and the growth of c-Myc dependent lymphoma.
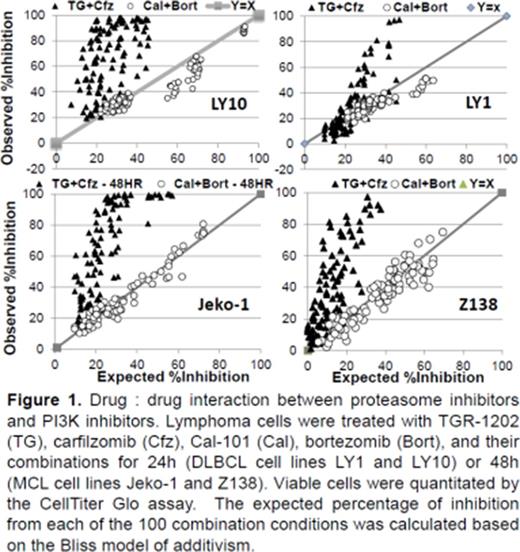
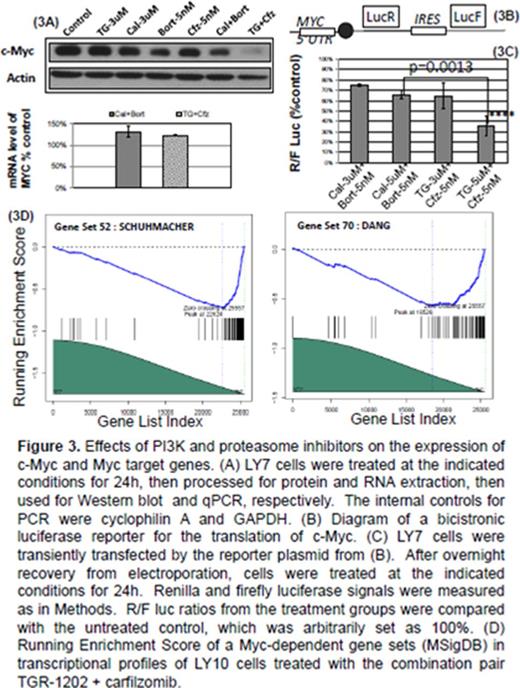
Methods: Cytotoxicity was studied in lymphoma cell lines and primary lymphoma cells using Cell TiterGlo. The Bliss additivism model was used to determine the expected inhibition of cell growth. The difference of the expected and observed levels of inhibition was used to calculate the excess over Bliss (EOB) values. EOB values above 0 indicate synergy, with higher values indicating higher levels of synergy. Mechanisms of synergy were determined through interrogation of PI3K/AKT/mTOR pathway and its downstream targets. Expression of c-Myc was investigated at the translation and transcription levels, using a combination of Western blot, qPCR, and a bi-cistronic luciferase reporter we developed to study cap dependent translation. Gene expression profiling (GEP) studies were conducted using RNAseq, and analyzed by the Fisher t-test and running enrichment score (RES) between different treatment groups.
Results: We used a high-throughput platform to screen the cytotoxicity of two PI3Kdelta inhibitors (TGR-1202 & idelalisib/Cal-101), two proteasome inhibitors (bortezomib & carfilzomib), and four combination pairs using these drugs. We found that TGR-1202 and Cal-101 caused only minimal to mild inhibition of lymphoma cells, while bortezomib and carfilzomib caused potent inhibition as single agents. The combination of TGR-1202 and carfilzomib was consistently the most synergistic doublet, while the combination of Cal-101 and bortezomib the least synergistic in numerous lymphoma cell lines studied to date (Figure 1). TGR-1202 and carfilzomib were also highly synergistic in primary lymphoma cells, while Cal-101 and bortezomib were not. Importantly, normal lymphocytes were resistant to the combination of TGR-1202 and carfilzomib. At the molecular level, only the combination of TGR-1202 and carfilzomib potently inhibited mTORC1 dependent phosphorylation of 4E-BP1, leading to marked reduction of c-Myc protein (Figures 2 & 3). In contrast, the combination of TGR-1202 and carfilzomib produced no reduction of the mRNA level of c-Myc (Figures 3). A luciferase reporter demonstrated that the synergistic combination TGR-1202 and carfilzomib specifically inhibited the translation downstream of the 5'UTR of c-Myc (Figure 3). GEP studies confirmed that the canonical c-Myc target genes were potently downregulated at the level of transcription by the combination of TGR-1202 and carfilzomib (Figure 3). These results demonstrate that TGR-1202 and carfilzomib in combination potently inhibited the translation of c-Myc and the c-Myc transcriptional program, which appears to be primarily through disruption of the PI3Kdelta and proteasome pathways that converge on mTOR. Ongoing experiments are focused on confirmation of these observations in vivo. Further, a phase I/II clinical trial evaluating this combination regimen in aggressive c-Myc driven lymphomas is being planned.
Deng:TG Therapeutics: Research Funding; Gilead: Research Funding; Amgen/Onyx: Research Funding. Lentzsch:Celgene: Consultancy; BMS: Consultancy; Novartis: Consultancy; Janssen: Consultancy; Axiom: Honoraria. O'Connor:Celgene: Consultancy, Honoraria, Membership on an entity's Board of Directors or advisory committees, Research Funding; Mundipharma: Consultancy, Research Funding; Acetylon: Consultancy, Other: Consultancy fee; Spectrum Pharmaceuticals: Consultancy, Honoraria, Research Funding; Bristol-Myers Squibb Company: Consultancy, Other: Consultancy fee; Takeda Millenium: Consultancy, Honoraria, Other: Consultancy fee, Research Funding; Novartis: Consultancy, Honoraria, Other: Consultancy fee; Seattle Genetics: Research Funding; Bayer: Consultancy, Honoraria.
Author notes
Asterisk with author names denotes non-ASH members.