Abstract
Introduction: Systemic light chain (AL-) amyloidosis is a rare protein deposition disorder which is caused by a monoclonal plasma cell or B cell disorder with poor prognosis if the heart is severely affected. In a retrospective EBMT analysis allogeneic stem cell transplant (allo-SCT) performed from 1991 until 2003 has emerged as an effective treatment but was associated with a high non-relapse-mortality (NRM) (Schönland et al., Blood 2006).
Patients and Methods: We performed a prospective non-interventional study (NIS) within the EBMT using allo-SCT in AL amyloidosis patients. Primary endpoint was efficacy (best hematologic remission (HR) and organ response). Secondary endpoints were acute and chronic Graft-versus-host-disease (GvHD), NRM, non-hematologic toxicity, event-free and overall survival (OS). We selected those centres that had performed any allogeneic HSCT for AL amyloidosis in the past. We approached 24 centres, of which 6 participated. Fourteen patients have been included and were transplanted between 2006 and 2014. Median age at allo-SCT was 50 years (range, 41 - 60). Five patients had cardiac and 10 patients kidney involvement at diagnosis. As underlying hematologic disease one patient had a M. Waldenström, the other 13 patients had a clonal plasma cell dyscrasia. All but one patient were in a good performance status (80-100%) assessed by Karnofsky Index at allo-SCT. Previous chemotherapy included high-dose melphalan (HDM) with autologous stem cell transplantation in 11 patients as well as bortezomib, lenalidomide, melphalan, rituximab and steroids. Disease stages at allo-SCT were as follows: 2 CRs, 1 VGPR, 6 PRs, 3 no responses and 1 with progression. Two patients received myeloablative and 12 reduced intensity conditioning (RIC, TBI 2 Gy / fludarabine in 10 patients, TBI 6 Gy in one patient). Three patients received T cell depletion (2 with ATG, one with Campath). HDM 200 mg/m2 was applied prior to the one syngeneic SCT. Donors were: 8 identical siblings, 1 mismatched relative, 1 syngeneic, 3 matched unrelated donors and 1 mismatched unrelated donor (MMUD). Source of stem cells was peripheral blood in 13 and cord blood in 1 patient, respectively. Time from diagnosis to allo-SCT was 23 months in median (range, 4-61).
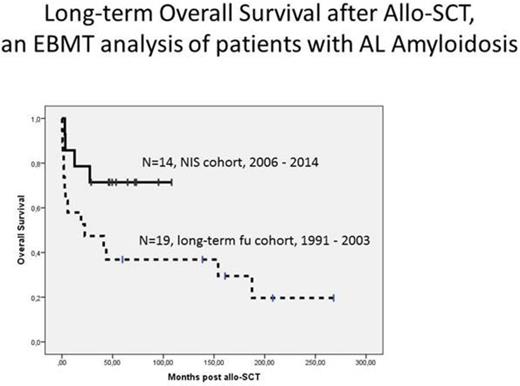
Results: All but one patient engrafted. Acute GvHD grade II-IV occurred in 4 patients and chronic GvHD in 9 patients (4 patients with limited and 5 with extensive disease, respectively). NRM occurred in 3 patients (GvHD, infection and suicide). One patient died due to progressive disease. 1- and 2-year-mortality was 14 and 21%, respectively. Best HR after allo-SCT was CR in 9 (64%). Ten patients were alive after an estimated median follow-up of 53 months (figure, continuous line) with an OS plateau beginning at 28 months post allo-SCT of 70%. Four patients relapsed or progressed and 7 patients were alive and relapse-free.
In addition, we updated the 19 AL patients of our published cohort (Schönland et al., Blood 2006). 1- and 2-year-mortality was 42 and 53%, respectively. Five (26%) patients were still alive after a cumulative median follow-up of 208 months, four of these living longer than 10 years after allo-SCT (figure, dashed-line).
Conclusion: Preliminary analysis of our NIS shows that allo-SCT is nowadays feasible and highly effective in selected patients with AL amyloidosis. In opposite to our retrospective analysis we observed a rather low NRM using mostly reduced-intensity conditioning with TBI 2 Gy and fludarabine. Furthermore, both analyses revealed rewarding long-term survival suggesting very good disease control. Therefore, allo-SCT might be a reasonable treatment option in young, medically fit and heavily pretreated patients (e.g. relapse or non-response after HDM).
Schönland:Prothena: Consultancy; Janssen: Consultancy, Honoraria, Research Funding. Hegenbart:Janssen: Honoraria. Schipperus:Novartis: Consultancy. Garderet:Bristol-Myers Squibb: Consultancy.
Author notes
Asterisk with author names denotes non-ASH members.