Abstract
Introduction: Based on combination of the three markers (CD10, Bcl6 and MUM1), Hans algorithm could divide DLBCL into two groups (GCB and non-GCB subtype). Although MUM1 is used as a post GC marker, cases with coexpression of CD10 and MUM1 (CD10+ MUM1+, double positive or DP), which was classified as GCB subtype according to Hans algorithm, do exsit. However, the differences of clinical characteristics and prognosis between DP and other GCB (GCB excluding DP) is unknown. Additionally, DLBCL without any positive staining of these three markers (CD10¨C Bcl6¨C MUM1¨C, triple negative or TN) were also noted. These cases, based on Hans algorithm, are classified as non-GCB subtype. However, little was known about the difference between TN cases with GCB or other non-GCB (non-GCB excluding TN).
Patients and methods: Immunohistochemistry was appiled in this study with the antibodies as follows. CD10 (clone 56C6, Dako), CD20 (clone L26, Abcam), Bcl6 (clone LN22, Dako), and MUM1 (clone MUM1p, Dako), FOXP1 (clone JC12, Abcam), GCET1 (clone RAM341, Abcam), LMO2 (clone 1A9-1, Santa Cruz), Myc (clone Y69; Abcam, cut-off: 40%) and Bcl2 (clone 124; Dako, cut-off: 50%). Fluorescence in situ hybridization (FISH) was carried out according to manufacturer¡¯s instructions on with the following probes: MYC dual-color, break apart translocation probe (Vysis LSI) and IGH/BCL2 dual-color, and dual fusion translocation probe (Vysis LSI). For cases with MYC translocation, BCL6 dual-color break apart rearrangement probe (Vysis LSI) wasfurtheranalyzed. A total of 601 cases were included in the study. Among these, 306 cases were treated with rituximab based chemoimmunotherapy and well follow up. The median follow up time was 24.3 months (1 to 115.4 months).We analyzed the clinical features of different groups: GCB vs. non-GCB; DP vs. other GCB (GCB*) or non-GCB; TN vs. other non-GCB (non-GCB*) or GCB. Besides, we further analyzed the survival differences among above groups in patients who were treated with rituximab based chemoimmunotherapy and well followed up.
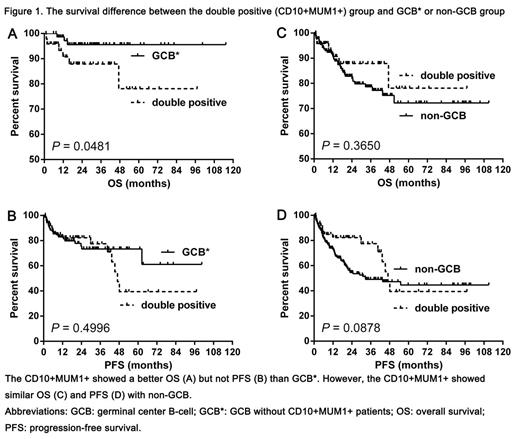
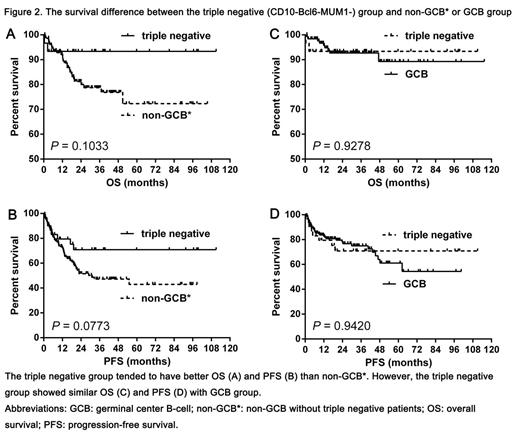
Results: The incidence of the DP patients was 13.3% (80/601, 95%CI: 10.7%-16.3%). The DP phenotype was more likely to occur in elderly patients (P =0.0432) and associated with poor PS status (P =0.0192) than GCB* phenotype. Additionally, although not statistically significant, the DP group showed higher incidence of double hit lymphoma (DHL) than GCB* patients (10.7% vs 2.9%, P =0.139). However, the DP group showed more frequent incidence of double expression lymphoma (DEL, Myc and Bcl2 coexpression) (P =0.044), MYC rearrangement (P =0.016) and DHL (P =0.029) than non-GCB group. The incidence of the TN patients was 8.8% (53/601, 95%CI: 6.7%-11.4%). There was no difference in any of clinical characteristics between the TN and GCB group. However, advanced Ann Arbor stage (III or IV) (P =0.0442), better PS status (P =0.0321), high-risk IPI (P =0.0042) Myc expression as well as BCL2 rearrangement were significantly more common in the non-GCB* group than the TN group. The DP group showed similar overall survival (OS) (median OS: both not reached, P =0.3650) and progression-free survival (PFS) (median PFS: 47.0 vs. 32.7 months, P =0.0878) with the non-GCB group while the TN group showed similar OS (median OS: both not reached, P =0.9278) and PFS (median PFS: both not reached, P =0.9420) with the GCB group (Fig 1-2).
Conclusion: Cases in the DP and TE group might hinder the intrinsic power of Hans algorithm in other studies. More detailed classification of DLBCL based on Hans algorithm may help to identify patients with distinct clinical characteristics and prognosis, thereby improving the stratification of patients for risk-adjusted therapies.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.