Abstract

Background
Therapy-related Myelodysplastic Syndromes (t-MDS) are those MDS occurring after cytotoxic and/or radiation therapy administered for a prior neoplastic or non-neoplastic disorder. Their prognosis is generally very poor. The commonly used risk prognostic models for MDS (IPSS and IPSS-R) are not validated in this entity as they were developed after the exclusion of therapy-related cases (Greenberg et al. Blood 1997; Greenberg et al. Blood 2012).
Aims
The main aims of this study are: a) to report clinical findings and overall survival on 233 patients with t-MDS, and to compare them with a large series of de novo cases; b) to test if IPSS-R is applicable to t-MDS patients.
Patients and methods
The study is based on the Spanish Registry for MDS, a retrospective database that includes more than 10000 cases. The investigators were asked to fill in a questionnaire regarding prior disease (PD) and prior therapy in those cases reported to be t-MDS. Herein are described the clinical features and overall survival of the first 233 cases with the required information, and compared with patients with de novo MDS from a single center series (n=725). Log Rank test was applied to asses IPSS-R in t-MDS group.
Results
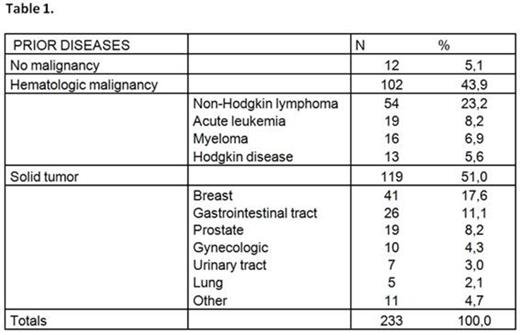
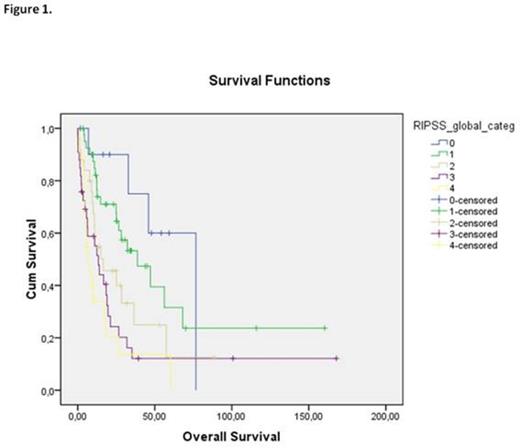
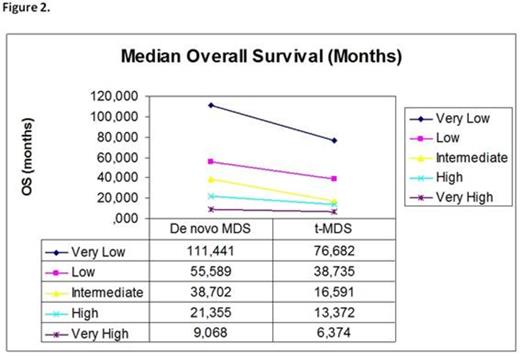
The 233 reported patients were diagnosed between January 1993 and February 2014. The series includes 104 women (44,6%) and 129 men (55,4%). One hundred and two patients (43.9%) had a primary hematologic malignancy, 119 (51%) had a solid tumor, and 12 (5.1%) received cytotoxic therapy for autoimmune disorders. Ninety eight patients (42.6%) received only chemotherapy (CT), 45 (19.6%) received only radiotherapy (RT), 44 (19.1%) received combined modality treatment (CMT), and 43 (18.6%) received an autologous stem cell transplantation (ASCT). The median time of latency between PD and diagnosis in t-MDS group was 4.56 years (range: 0.03-29.63) in patients previously treated with CT or CMT, significantly lower than the observed after RT (8.54; range 0.83-23.02) or ASCT (8.64; range 2.87-28.32) groups (p=0.023 and p<0.0001, respectively). Median age, hemoglobin concentration, platelet count and absolute neutrophil count at diagnosis were significantly lower in t-MDS compared with de novo MDS, while bone marrow blast cell count was significantly higher. A higher proportion of high risk karyotypes (intermediate, poor and very poor categories of R-IPSS for cytogenetics) in t-MDS than in de novo MDS was observed (45.5% versus 25.6% respectively, p<0.0001). Within t-MDS cases, those patients who had received CT, CMT or ASCT also presented a higher proportion of high risk karyotypes compared with t-MDS after RT (52.1 vs 24.1% respectively, p=0.006). There was a significantly shorter median overall survival in patients treated with CT/CMT or ASCT in comparison with de novo patients or t-MDS patients treated with RT (14.88 versus 25.06 versus 47.18 months, respectively (log rank test < 0, 0001). In contrast, no difference between de novo and t-MDS after RT was found (median survival 53.6 months vs. 47.17 months, respectively, n.s). These findings are in concordance with previously published data (Nardi et al, JCO 2012) suggesting that some t-MDS after RT may not be truly t-MDS, but just coincidental. The IPSS-R prognostic score could separate t-MDS patients into five risk groups in terms of overall survival, with a median survival of 76.68 months, 38.73 months, 16.59 months, 13.3 months and 6.37 months, respectively (p<0.0001; Figure 1). A shorter overall survival for each category was found in t-MDS in comparison with de novo MDS, reaching statistical significance in the intermediate and high risk category and showing a trend towards significance in the very low and low risk categories (Figure 2).
Conclusions
In conclusion, our data supports the notion that t-MDS may contain entities with heterogeneous prognosis due to a diverse biological basis. The capacity of the IPSS-R for separating good prognostic from bad prognostic cases shown in this study could be very useful in the clinical setting in order to offer risk-adapted treatments to patients, although the development of a specific prognostic score for these entities would be needed.
<![if !vml]><![endif]>
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This icon denotes a clinically relevant abstract