Abstract
Background and Objective: The advent of plasma exchange has led to a dramatic improvement in the survival of patients with thrombotic thrombocytopenic purpura (TTP). Recovery from TTP is usually complete, but may be complicated by a significant rate of relapse, particularly in the first year after the acute episode. Recent reports also suggest that survivors of TTP may have a poorer health related quality of life than previously estimated. We followed a cohort of 100 patients diagnosed with TTP to estimate the burden of chronic renal impairment, hypertension, diabetes, stroke, depression and other psychiatric and neurologic conditions in this group.
Patients and Methods: A total of 100 consecutive patients treated for TTP at the Cleveland Clinic from January 2000 to March 2012 were identified. Nine patients died and the remaining 91 patients were followed until death or date of last clinical contact. The point prevalence of chronic kidney disease, hypertension, diabetes, stroke, major depression and other neurologic and psychiatric conditions was compared to expected values in the reference US population [based on National Health and Nutrition Examination Survey (NHANES) data] adjusted for age and sex.
Results: Of the 91 patients who survived a first episode of TTP, 69 (75.8%) were female, with an age range of 16 to 79 years (median 44 years). Fifty one percent of patients were Caucasian, 45% African American and 2% Hispanic. Sixty three percent of cases occurred without predisposing conditions while 12.1% were associated with autoimmune disease (5 with SLE, 2 with rheumatoid arthritis, one with SLE and rheumatoid arthritis, and one each with Sjogren's syndrome, dermatomyositis and mixed connective tissue disorder), 8% with pregnancy or the postpartum state, 6.6% with cancer and 5.5% with solid organ transplant.
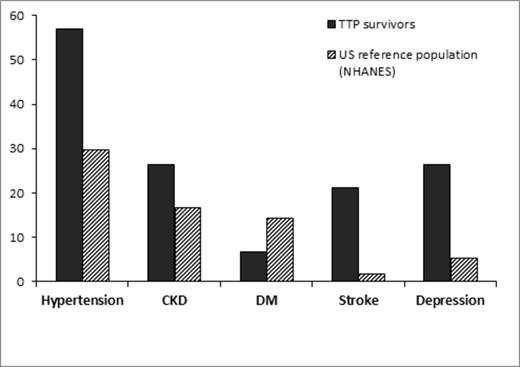
The median follow up time was 59 months (range 1-117 months). During this period, 18 patients suffered relapses (11 patients had 1 relapse, 6 patients had 2 relapses, and 1 had three relapses). Compared to the reference US population, survivors of TTP had a higher prevalence of hypertension (61.5% versus 29.8%), chronic renal disease (26.4% versus 16.8%) and stroke (12.1% versus 1.87%). TTP survivors also had a high prevalence of neurologic disorders including migraines (n=9), multiple sclerosis (n=1), fibromyalgia (n=1) and restless leg syndrome (n=2). There was a five-fold higher incidence of major depression requiring pharmacologic treatment compared to the reference population (26.4% versus 5.4%). We also noted a significant prevalence of other mental health disorders such as anxiety disorders (n=15), bipolar disorder (n=2), adjustment disorder (n=1) and conversion disorder (n=1). The incidence of diabetes was lower than seen in the reference population (6.6% versus 14.4%).
Conclusion: Survivors of TTP are at higher risk for poor health outcomes including chronic cardiovascular disease, neurologic disease and psychiatric conditions, all of which impair quality of life. These may be related to persistent organ damage from microvascular dysfunction during the acute episode of TTP, or from co-morbid conditions such as auto-immune diseases that are independent risk factors for poor outcomes. Our results highlight the importance of continued follow up in order to address the long-term health problems associated with TTP survivorship.
Prevalence of health outcomes in TTP survivors compared to the US reference population.
Prevalence of health outcomes in TTP survivors compared to the US reference population.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.