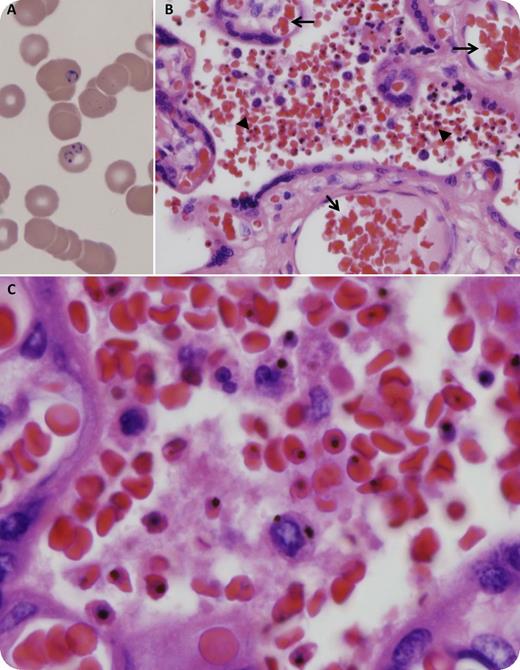
A 26-year-old, gravida 1, para 0, 37-week-pregnant immigrant from Burkina Faso presented with a 1-week history of intermittent fevers, headache, and myalgia. She had a past medical history of malaria (10 years before admission) in Burkina Faso, where she most recently visited on a 2-week trip about 2 months prior to admission. A complete blood count showed anemia and thrombocytopenia (hemoglobin 7.4 g/dL, reticulocytes 7.4%, platelets 70 × 109/L). A peripheral smear demonstrated intraerythrocytic ring forms of Plasmodium falciparum (panel A) and an estimated parasitemia rate of 3.6%. Treatment with intravenous quinine and clindamycin was initiated and the patient underwent emergent cesarean delivery (1.5 hours after the first dose of quinine) for nonreassuring fetal tracing. Histologic sections of the placenta showed acute low-grade intervillousitis with numerous maternal red blood cells containing malaria pigment (panel B arrowheads and panel C) and unremarkable fetal vascular circulation (panel B arrows). The final diagnosis was acute malaria in the mother with parasite sequestration in the villous chamber. The patient completed a 7-day course of quinine and clindamycin. Both she and her son had an uneventful recovery. When readily available (unlike in our case), intravenous artesunate is the preferred treatment of severe malaria.
A 26-year-old, gravida 1, para 0, 37-week-pregnant immigrant from Burkina Faso presented with a 1-week history of intermittent fevers, headache, and myalgia. She had a past medical history of malaria (10 years before admission) in Burkina Faso, where she most recently visited on a 2-week trip about 2 months prior to admission. A complete blood count showed anemia and thrombocytopenia (hemoglobin 7.4 g/dL, reticulocytes 7.4%, platelets 70 × 109/L). A peripheral smear demonstrated intraerythrocytic ring forms of Plasmodium falciparum (panel A) and an estimated parasitemia rate of 3.6%. Treatment with intravenous quinine and clindamycin was initiated and the patient underwent emergent cesarean delivery (1.5 hours after the first dose of quinine) for nonreassuring fetal tracing. Histologic sections of the placenta showed acute low-grade intervillousitis with numerous maternal red blood cells containing malaria pigment (panel B arrowheads and panel C) and unremarkable fetal vascular circulation (panel B arrows). The final diagnosis was acute malaria in the mother with parasite sequestration in the villous chamber. The patient completed a 7-day course of quinine and clindamycin. Both she and her son had an uneventful recovery. When readily available (unlike in our case), intravenous artesunate is the preferred treatment of severe malaria.
For additional images, visit the ASH IMAGE BANK, a reference and teaching tool that is continually updated with new atlas and case study images. For more information visit http://imagebank.hematology.org.