To the editor:
In the paper by Resnick et al, the authors clearly defined lymphoma, lung impairment, hepatitis, and gastrointestinal disease as the main causes of mortality in 411 subjects with common variable immunodeficiency (CVID) followed over 4 decades in New York.1 This careful analysis prompted us to assess the complications associated with poor survival over the same period of 4 decades in our cohort of 353 adult Italian CVID subjects (174 males, 179 females). The diagnosis of CVID was made by standard criteria.2 All data have been collected during the patient's monthly visits at the time of Ig replacement that, in Italy, occurs only during hospital settings. For mortality analysis, the time since diagnosis was determined starting from the age of CVID diagnosis. Probabilities of survival after diagnosis of CVID were estimated from Kaplan-Meier analysis. The median age at diagnosis was 40 years for females and 36 years for males.
Sixty-nine of 353 patients (19.5%) died, a percentage overlapping that were found in the New York cohort (93 of 473, 19.6%). The median age at death was 53 years for males and 54 years for females. Differently from the New York cohort that included also CVID patients with a pediatric age of onset, in adult onset CVID, the age at death did not correlated with early age at symptom onset and age at diagnosis.
Seventy-three of 353 patients (20.7%) developed cancers, a percentage higher than that reported in the New York cohort (72 of 473, 15.2%). In both cohort relevant causes of death included respiratory failure from chronic lung disease, and lymphoma. Death for respiratory failure from chronic lung disease accounted for 30.4% in Italy, and 36% in New York. However, despite the same percentages of cumulative deaths, in the Italian CVID patients, deaths from cancers occurred in 36 patients (10.2%) who developed a malignancy, while in the New York cohort it occurred in 27 patients (5.7%). In Italy, we found a higher percentage of death because of malignancies other than lymphomas (33.3% vs 10.7% in New York), while the percentage of patients died for lymphomas was similar (18.8% vs 18.3%).
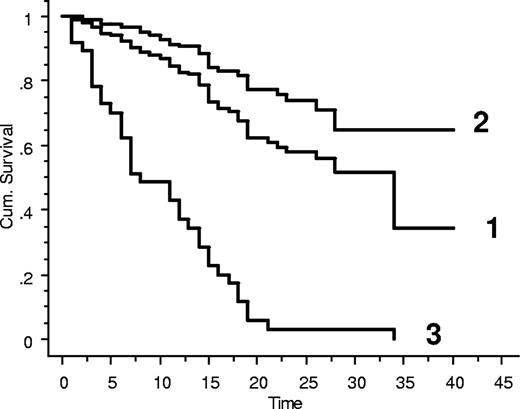
Lymphoma types were: non-Hodgkin lymphoma, not further classified (24% in Italy vs 59% in New York); diffuse large B-cell lymphoma (40% vs 7%); Hodgkin disease (8% vs 10%); MALT (12% vs 12%); marginal zone lymphoma (4% vs 2%); monoclonal B lymphocytosis (8% vs 2%); and T cell–rich B-cell lymphoma (4% vs 2%). Diffuse large B-cell lymphomas, non-Hodgkin lymphoma not further classified, and T cell–rich B-cell lymphoma had the highest mortality in both cohorts. The importance of cancers as CVID-associated diseases is further underlined by the observations that in 5 patients an intestinal adenocarcinoma was the first clinical presentation of CVID; and that in 9 patients (2.7%) 2 distinct primary malignancies occurred. The overall survival over 40 years was 36%, not different for males and females. As shown in Figure 1, the Kaplan-Meier survival curves demonstrated that the poor long-term survival of adult CVID patients is because of cancers.
Kaplan-Meier curves for patients with CVID. (1) Cumulative; (2) without cancers; and (3) with cancer complications.
Kaplan-Meier curves for patients with CVID. (1) Cumulative; (2) without cancers; and (3) with cancer complications.
Our mortality data are higher than we previously reported (6%) analyzing data from an Italian CVID cohort followed both in pediatric and adult clinics for a much shorter period of 11 years3 and cited by Resnick and coworkers.1 Noteworthy, the survival data we reported in 2007 included also patients with a CVID paediatric onset, excluded from the present analysis.
In conclusion, since its introduction in the early 1980's Ig replacement did a great job in that the mortality for infections at present does not represent a major clinical problem. Rather, attention must be paid to early diagnosis of nonlymphoid and lymphoid cancers.
Authorship
Conflict-of-interest disclosure: The authors declare no competing financial interests.
Correspondence: Isabella Quinti, Department of Molecular Medicine, Sapienza University of Rome and Fondazione Elenora Lorillard Spencer Cenci., Viale dell'Università 37, Rome 00185, Italy; e-mail: isabella.quinti@uniroma1.it.