Abstract
Polymorphonuclear neutrophil (PMN) extravasation requires selectin-mediated tethering, intercellular adhesion molecule-1 (ICAM-1)–dependent firm adhesion, and platelet/endothelial cell adhesion molecule 1 (PECAM-1)–mediated transendothelial migration. An important unanswered question is whether ICAM-1–activated signaling contributes to PMN transmigration mediated by PECAM-1. We tested this concept and the roles of endothelial nitric oxide synthase (eNOS) and Src activated by PMN ligation of ICAM-1 in mediating PECAM-1–dependent PMN transmigration. We observed that lung PMN infiltration in vivo induced in carrageenan-injected WT mice was significantly reduced in ICAM-1−/− and eNOS−/− mice. Crosslinking WT mouse ICAM-1 expressed in human endothelial cells (ECs), but not the phospho-defective Tyr518Phe ICAM-1 mutant, induced SHP-2–dependent Src Tyr530 dephosphorylation that resulted in Src activation. ICAM-1 activation also stimulated phosphorylation of Akt (p-Ser473) and eNOS (p-Ser1177), thereby increasing NO production. PMN migration across EC monolayers was abolished in cells expressing the Tyr518Phe ICAM-1 mutant or by pretreatment with either the Src inhibitor PP2 or eNOS inhibitor L-NAME. Importantly, phospho–ICAM-1 induction of Src signaling induced PECAM-1 Tyr686 phosphorylation and increased EC surface anti–PECAM-1 mAb-binding activity. These results collectively show that ICAM-1–activated Src and eNOS signaling sequentially induce PECAM-1–mediated PMN transendothelial migration. Both Src and eNOS inhibition may be important therapeutic targets to prevent or limit vascular inflammation.
Introduction
Tissue polymorphonuclear neutrophil (PMN) infiltration is required for effective host defense, but the recruitment and activation of PMNs, if unchecked, can also produce inflammation and injury.1 For PMNs to cross microvessels, they must first adhere firmly to endothelial cells (ECs),2 which form a cup-like structure surrounding adherent leukocytes to direct the cell through the barrier.3,4 Intercellular adhesion molecule-1 (ICAM-1)–mediated firm adhesion of leukocytes to ECs is a requisite step in PMN transmigration.2 Platelet/endothelial cell adhesion molecule 1 (PECAM-1) expressed in the EC plasma membrane is also critically involved in the mechanism of PMN transmigration.5,6 Based on the key roles of both ICAM-1 and PECAM-1, a fundamental question is whether these adhesive proteins cooperate in the mechanism of PMN transmigration.
Activation of ICAM-1, as defined by ICAM-1 phosphorylation,7,8 induces ICAM-1 clustering and its association with the actin cytoskeleton.9,10 Multiple signaling pathways, such as Ca2+,11 RhoA,12,13 RhoG,4 MAPK (p38),14 and Src,11,15-17 have been invoked to explain the mechanism of ICAM-1 activation and clustering. Recently, it was also shown that ICAM-1 ligation-dependent endothelial nitric oxide synthase (eNOS) activation via the AMPK pathway in rat brain endothelial cells signals lymphocyte transmigration.18 However, although Src and eNOS activation have been demonstrated to play key roles in leukocyte transmigration,16 their mechanism of action is still not known. We have shown8 Src-dependent ICAM-1 phosphorylation at Tyr518. However, it is also possible that ICAM-1, on activation, can itself stimulate Src kinase activity placing Src both upstream and downstream of ICAM-1. Here we addressed the question whether the initial firm ICAM-1–mediated PMN adhesion can induce PECAM-1–dependent PMN transmigration and whether activation of Src and eNOS signaling downstream of ICAM-1 is an essential requirement of the PECAM-1–dependent inflammatory response.
There is precedence for invoking Src activation downstream of ICAM-1. The interaction of ICAM-1 with fibrinogen was shown to induce ICAM-1 phosphorylation on Tyr5187 as well as monocyte transmigration.19 Tyrosine phosphatase SHP-2 interacting with Tyr518 in the ICAM-1 C-terminal domain ITAM motif (I/V/L)XYXX(l/V)7 may regulate endothelial cell Src activity. An engineered SHP-2 mutant targeted to the plasma membrane was shown to stimulate Src activity,20 suggesting a role of SHP-2 in mediating ICAM-1 dependent Src signaling. Src is thus a potentially important target that may be the key to understanding PMN transmigration. Src also induces PI3K-dependent Akt phosphorylation and eNOS activation by phosphorylating eNOS at Ser117.7,21 Thus, ICAM-1 activation-dependent eNOS signaling downstream of ICAM-1 activation may also be involved in PMN transmigration.
Methods
Mice
Wild-type (WT) C57BL/6 and knockout strains (ICAM-1−/− and eNOS−/−) in the same background were purchased from The Jackson Laboratory. Mice weighing 20-30 g and 10-12 weeks of age were used. All animal procedures were approved by the University of Illinois Animal Care and Use Committee in accordance with Association for Assessment and Accreditation of Laboratory Animal Care guidelines.
Materials
Polyclonal ICAM-1, c-Src, and GAPDH antibodies and monoclonal PECAM-1 and SHP-2 antibodies were from Santa Cruz Biotechnology. Phospho-Tyr518 ICAM-1 antibody was from Abcam. Active phospho-Src (mouse Y418 or human Y419), Src inactive site phospho-Tyr (mouse Y529 or human Y530), phospho-eNOS (S1177), phospho-Akt (T473), and total Akt were from Cell Signaling. Monoclonal anti-eNOS was from EMD Biosciences. Monoclonal anti–mouse ICAM-1 antibody (YN1/1.7.4), FITC-480–labeled YN1/1.7.4, and control rat IgG2b used in ICAM-1 crosslinking studies were from eBioscience. Phospho–PECAM-1 (Tyr686) polyclonal antibody was from Assay Biotechnology Company. Monoclonal M2 anti-Flag antibody and secondary anti–rat antibody used in crosslinking studies were from Sigma-Aldrich. PP2, wortmannin, and L-NAME were from Calbiochem. Carrageenan, protease inhibitor cocktail, and all other chemical reagents were from Sigma-Aldrich. AMP kinase inhibitor 5-iodotubercidin was from Biaffin GmbH & Co KG.
Cell culture and mouse ICAM-1 expression model
HUVECs were used between passage 5 ad 7 and transiently transfected with mouse ICAM-1 cDNA by Lonza Nucleofector kit according to the manufacturer's instructions.8 Expression of mouse ICAM-1 in human endothelial cell monolayers was used to assess downstream signaling mechanisms evoked by ICAM-1 ligation per se compared with phospho-defective ICAM-1 mutant in the absence of cytokine stimulation known to activate similar signaling pathways.8 For coimmunoprecipitation assay, HEK cells cultured in DMEM with 10% FBS were used for transfection of ICAM-1.
ICAM-1 crosslinking
ICAM-1 was crosslinked as described.22,23 Briefly, HUVECs expressing mouse ICAM-1 were washed once with EBM-2 and incubated with 15 μg/mL rat anti–mouse ICAM-1 monoclonal antibody at room temperature for 20 minutes. Rat IgG2b was used as a control antibody. The cells were then washed twice and anti–rat IgG (50 μg/mL) was added to crosslink ICAM-1 for 20 minutes at 37°C.
Communoprecipitation and Western blotting
After ICAM-1 crosslinking, HEK or HUVECs were placed on ice and lysed in buffer containing 50mM Tris-HCl, pH7.5, 150mM NaCl, 1% Triton X-100, 1mM PMSF, and Sigma protease inhibitor. After low-speed centrifugation (100g, 10 minutes, 4°C), the supernatants were collected for coimmunoprecipitation and Western blot. Protein concentration was determined with Bio-Rad Dc protein assay solution (Bio-Rad). For coimmunoprecipitation, SHP-2 antibody was incubated with the lysates overnight at 4°C and Protein A beads were added and incubated for 1 hour at 4°C. The precipitated proteins were eluted by sample buffer. SHP-2 and ICAM-1 in the precipitated proteins were analyzed with Western blot.
MPO activity assay
To determine PMN infiltration, myeloperoxidase (MPO) activity of lung lysates was measured and used as a marker of PMN accumulation. Four hours after intrapleural injection of 0.2 mL of 1% carrageenan or saline, mouse lungs were homogenized in 0.5% hexadecyl-trimethylammonium bromide dissolved in 10mM potassium phosphate buffer (pH 7). After centrifugation for 20 minutes at 20 000g at 4°C, aliquots of the supernatant were assessed for total protein concentration and MPO activity. A 10-μL aliquot of each sample (supernatant) was loaded per well of a 96-well plate, and then O-dianisidine dihydrochloride with 0.0005% hydrogen peroxide in phosphate buffer (190 μL per well) was added to the samples. Absorbance readings were measured at 460 nm for 3 minutes. MPO activity was expressed as the change in absorbance per minute per gram of tissue.
NO measurements
After ICAM-1 crosslinking or addition of activated PMNs to EC monolayers, NO produced by HUVECs in 12-well plates was measured using a porphyrinic NO electrode as described.21 Briefly, the electrode is created by coating carbon fibers with a metalloporphyrinic conductive polymer and subsequently sealed with Nafion. Each electrode is calibrated using a stock solution of NO-saturated water. NO diffusion into the Nafion membrane is oxidized to a nitrosyl ion, and the electron is transferred to the porphyrin of the conductive polymer, proceeding along the copper wire to a detector. The NO electrode is placed onto the surface of an EC monolayer, and 2 additional electrodes are added to the solution to generate a 650-mV potential. The system is coupled to a FAS1 femtostat and personal computer with electrochemical software (Gamry Instruments). Electrode current, which is proportional to NO concentration, is measured as a function of time. The cell culture medium temperature is maintained at 37°C.
PMN isolation, adhesion, and transendothelial migration
PMNs were isolated from WT C57BL/6 mouse blood. After blood sedimentation, the PMNs were collected from the plasma layer by centrifugation. After removal of red blood cells by hypotonic shock, PMNs were further isolated with Ficoll-Pacque PLUS (GE Healthcare) gradient centrifugation. The yield of PMNs was approximately 3 × 106 PMNs/mouse with a purity of > 90% and viability of > 95% as determined by Trypan blue exclusion.23 Isolated PMNs were labeled with fluorescent LeukoTracker solution (Cell Biolabs) according to the manufacturer's protocol and used immediately in adhesion and transendothelial migration assays.
To determine PMN adhesion, we used the CytoSelect Leukocyte-endothelium adhesion assay kit (Cell Biolabs). Briefly, confluent monolayers of transfected HUVECs were seeded onto gelatin-coated 24-well plates in 300 μL of EBM-2 medium supplemented with 2% FBS. Peripheral blood PMNs were labeled with fluorescent LeukoTracker for 60 minutes at 37°C and then added to the EC monolayer for 30 minutes. After washing with PBS, the remaining adherent PMNs were lysed and fluorescence measured with a fluorometer (FlexStation II; Molecular Devices) at excitation and emission wavelengths of 485 and 535 nm, respectively. To determine PMN transmigration, we used the CytoSelect Leukocyte Transmigration Assay kit (Cell Biolabs). HUVECs transfected with empty vector, WT mouse ICAM-1, and mutant mouse ICAM-1 cDNA were cultured in 24-well inserts (3 μm pore size) until confluent. After overnight 0.1% FBS incubation, LeukoTracker-labeled PMNs were added to ECs at a ratio of 10:1 and the inserts were placed in each well of a 24-well plate with culture medium containing PMN activator fMLP (1μM) for 3 hours. PMNs that transmigrated to the bottom chamber were collected, lysed, and the fluorescence level of supernatants determined with a fluorometer.
PECAM-1 antibody binding assay
After ICAM-1 crosslinking of transfected HUVECs in 96-well plates for 1 hour, the cells were subjected to PECAM-1 mAb binding assay. Cells were washed with serum-free medium and incubated with the PECAM-1 mAb diluted in medium (10 μg/mL) at 4°C for 1 hour. Cells were then fixed with 4% paraformaldehyde for 15 minutes at 4°C followed by PBS washing and incubation with HRP-labeled secondary Ab. After incubation with substrate TMB (3,3′,5,5′-tetramethylbenzidine), the optical density at 450 nm was measured and recorded.
Statistical analysis
All data are expressed as the mean ± SD unless otherwise indicated. Statistical differences between groups were determined using ANOVA or Student t test depending on group size. P values less than .05 were considered significant.
Results
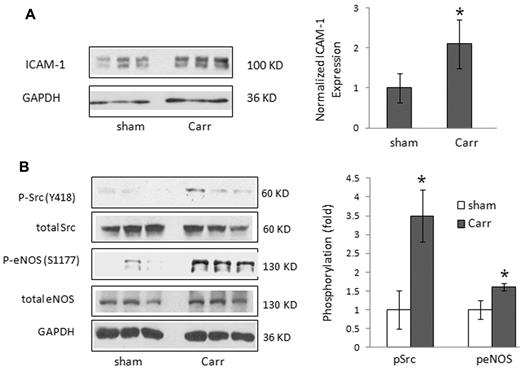
Carrageenan-induced PMN infiltration in mouse lungs is associated with an increase in ICAM-1 expression and activation of Src and eNOS
We used the mouse model of carrageenan-induced lung inflammation24 to address the role of ICAM-1–activated signaling in PMN extravasation. The initial phase of the carrageenan response involves secretion of TNF-α and IL-1β during the first 1 hour, followed by PMN infiltration over the next 2-6 hours.24 Thus, C57BL/6 mice were injected with 1% carrageenan or saline (sham) into the pleural space; then, lungs were collected and analyzed after 4 hours. Carrageenan injection induced a 2-fold increase in ICAM-1 expression (Figure 1A). Using phospho-specific antibodies, we also observed increased phosphorylation of Src and eNOS in lung tissue of carrageen-challenged mice compared with the saline-injected control mice (Figure 1B).
ICAM-1 expression, neutrophil (PMN) infiltration into the lung, and activation of Src and eNOS in carrageenan-treated mouse lungs. (A) Mice were injected in the pleural space with 1% carrageenan or saline (sham); and after 4 hours, lung tissue was collected and analyzed. ICAM-1 expression was determined by Western blot and densitometry (mean ± SD; n = 3, lung tissues from 3 mice in each group). *P < .05 versus sham. (B) Activation of Src and eNOS was determined by Western blot analysis. Tyrosine phosphorylation of Src at Y418 and serine phosphorylation of eNOS at S1177 were detected (triplicates are shown) by Western blotting mouse lung homogenates. *P < .05 versus sham.
ICAM-1 expression, neutrophil (PMN) infiltration into the lung, and activation of Src and eNOS in carrageenan-treated mouse lungs. (A) Mice were injected in the pleural space with 1% carrageenan or saline (sham); and after 4 hours, lung tissue was collected and analyzed. ICAM-1 expression was determined by Western blot and densitometry (mean ± SD; n = 3, lung tissues from 3 mice in each group). *P < .05 versus sham. (B) Activation of Src and eNOS was determined by Western blot analysis. Tyrosine phosphorylation of Src at Y418 and serine phosphorylation of eNOS at S1177 were detected (triplicates are shown) by Western blotting mouse lung homogenates. *P < .05 versus sham.
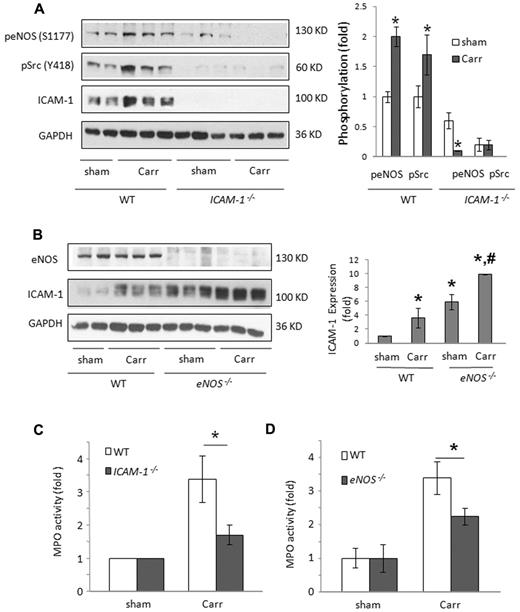
Leukocyte firm adhesion requires several adhesion molecules, such as ICAM-1, ICAM-2, and VCAM-1.25 Here we focused on the role of ICAM-1, which is essential for PMN firm adhesion to ECs26 and thus also thought to be required for subsequent PMN transmigration. We examined whether carrageenan-induced phosphorylation of Src and eNOS was dependent on ICAM-1 expression. Western blotting showed that auto-phosphorylation of mouse Src on Tyr418 and eNOS at Ser1177 was markedly reduced in ICAM-1−/− lungs basally and after carrageenan challenge (Figure 2A).
PMN lung infiltration and Src and eNOS activation are partially dependent on ICAM-1. (A) Carrageenan-induced Src and eNOS activation was partially dependent on ICAM-1 expression. Tyrosine phosphorylation of Src at Y418 and serine phosphorylation of eNOS at S1177 were reduced in carrageenan-treated ICAM-1−/− mice. (B) Enhanced basal lung ICAM-1 expression in eNOS−/− mice was further induced on carrageenan treatment. #P < .05 versus sham eNOS−/−; *P < .05 versus sham WT. (C) PMN lung infiltration induced by 4-hour carrageenan was reduced in ICAM-1−/− mice. (D) Carrageenan-induced PMN infiltration in the lung (after 4 hours) was reduced in eNOS−/− mice. PMN infiltration in the lung was determined by measuring MPO activity. (C-D) Data are mean ± SD (n = 5). *P < .05 (WT versus ICAM-1−/− or eNOS−/−) of the fold increase over sham treatment.
PMN lung infiltration and Src and eNOS activation are partially dependent on ICAM-1. (A) Carrageenan-induced Src and eNOS activation was partially dependent on ICAM-1 expression. Tyrosine phosphorylation of Src at Y418 and serine phosphorylation of eNOS at S1177 were reduced in carrageenan-treated ICAM-1−/− mice. (B) Enhanced basal lung ICAM-1 expression in eNOS−/− mice was further induced on carrageenan treatment. #P < .05 versus sham eNOS−/−; *P < .05 versus sham WT. (C) PMN lung infiltration induced by 4-hour carrageenan was reduced in ICAM-1−/− mice. (D) Carrageenan-induced PMN infiltration in the lung (after 4 hours) was reduced in eNOS−/− mice. PMN infiltration in the lung was determined by measuring MPO activity. (C-D) Data are mean ± SD (n = 5). *P < .05 (WT versus ICAM-1−/− or eNOS−/−) of the fold increase over sham treatment.
eNOS is required for carrageenan-induced PMN infiltration in mice
To address in vivo relevance of eNOS activation downstream of ICAM-1, we assessed carrageenan-induced pleurisy in eNOS knockout mice (eNOS−/−). WT or eNOS−/− mice were injected with carrageenan and ICAM-1 expression, and MPO activity was measured after 4 hours. Interestingly, we observed a 6-fold increase in basal ICAM-1 expression in eNOS−/− mice, which increased further on carrageenan challenge (Figure 2B), suggesting that eNOS, in addition to being essential for PMN sequestration and transmigration, may also negatively regulate ICAM-1 expression. PMN lung infiltration determined by MPO activity was increased 3-fold at 4 hours in WT control mice, whereas ICAM-1 knockout mice (ICAM-1−/−) showed 70% less MPO activity in lungs 4 hours after injection of carrageenan compared with WT control (C57BL/6) mice (Figure 2C). The increase in lung MPO activity induced by carrageenan injection in eNOS−/− mice was also 50% less than in WT mice (Figure 2D). Consistent with these data, we observed 50% fewer PMNs in bronchoalveolar lavage samples from carrageenan-treated ICAM-1−/− and eNOS−/− mice (supplemental Figure 3C, available on the Blood Web site; see the Supplemental Materials link at the top of the online article). Thus, regardless of the increase in ICAM-1 expression observed in eNOS−/− mice, PMN transmigration was reduced, suggesting that NO production plays a critical role in the mechanism of PMN extravasation in mouse lungs.
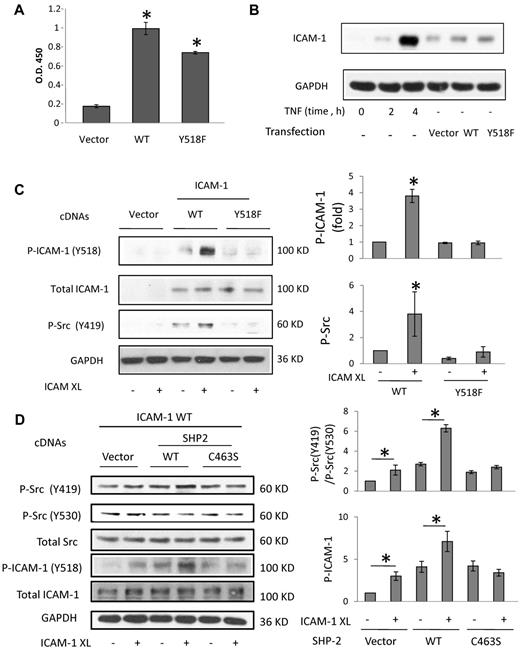
ICAM-1–mediated Src activation is dependent on SHP-2
As carrageenan-induced activation of Src and eNOS is attenuated in ICAM-1−/− mice, we next examined the role of ICAM-1 and its phosphorylation in the mechanism of Src and eNOS activation and signaling. WT and Y518F phosphorylation-defective mouse ICAM-1 mutant were expressed in HUVECs. Mouse ICAM-1 cDNA transfection resulted in equivalent cell surface expression of WT- and Y518F–ICAM-1 as evidenced by Western blotting and whole-cell ELISA assays (Figure 3A,C). Flow cytometric analysis demonstrated that ∼ 50% of HUVECs expressed the WT and mutant ICAM-1 at the similar levels (supplemental Figure 1A). In addition, expressed mouse WT and mutant ICAM-1 levels were comparable with endogenous ICAM-1 expression in HUVECs treated with TNF-α for 2 to 4 hours (Figure 3B), suggesting that the level of expression of WT and mutant mouse ICAM-1 in HUVECs was similar to endogenous ICAM-1 expression during the early stages of inflammation.
ICAM-1 activation-dependent stimulation of Src in HUVECs. (A) Mouse WT and phosphorylation-defective ICAM-1 mutant (Y518F) expressed in HUVECs were detected by ELISA. (B) Comparison of TNF-induced endogenous ICAM-1 expression and mouse ICAM-1 expression in transfected HUVECs. (C) ICAM-1 crosslinking (XL) was performed using a rat anti–mouse ICAM-1 mAb (YN1/1.7.4) against the mouse ICAM-1 extracellular LFA-1 binding domain. The expression of flag-tagged mouse WT and mutant ICAM-1 in human ECs was equivalent. Phosphorylation of Src at Y418 (human) and ICAM-1 at Y518 was determined using phospho-specific antibodies and Western blot analysis. Summarized results of protein phosphorylation assays are based on 3 or 4 experiments (mean ± SD). (D) HUVECs were cotransfected with mouse ICAM-1 and WT or phosphatase-dead C463S SHP2 mutant. Phosphorylation of Src Y419 (active site) increased and of Y530 (inactive site) decreased in the cells after ICAM-1 crosslinking. Phosphorylation of ICAM-1 Y518 was enhanced in the presence of WT SHP2. *P < .05 versus noncrosslinked control.
ICAM-1 activation-dependent stimulation of Src in HUVECs. (A) Mouse WT and phosphorylation-defective ICAM-1 mutant (Y518F) expressed in HUVECs were detected by ELISA. (B) Comparison of TNF-induced endogenous ICAM-1 expression and mouse ICAM-1 expression in transfected HUVECs. (C) ICAM-1 crosslinking (XL) was performed using a rat anti–mouse ICAM-1 mAb (YN1/1.7.4) against the mouse ICAM-1 extracellular LFA-1 binding domain. The expression of flag-tagged mouse WT and mutant ICAM-1 in human ECs was equivalent. Phosphorylation of Src at Y418 (human) and ICAM-1 at Y518 was determined using phospho-specific antibodies and Western blot analysis. Summarized results of protein phosphorylation assays are based on 3 or 4 experiments (mean ± SD). (D) HUVECs were cotransfected with mouse ICAM-1 and WT or phosphatase-dead C463S SHP2 mutant. Phosphorylation of Src Y419 (active site) increased and of Y530 (inactive site) decreased in the cells after ICAM-1 crosslinking. Phosphorylation of ICAM-1 Y518 was enhanced in the presence of WT SHP2. *P < .05 versus noncrosslinked control.
On ICAM-1 crosslinking, WT–ICAM-1–expressing cells showed ICAM-1 phosphorylation at Tyr518 as well as human Src auto-phosphorylation (pTyr419), respectively (Figure 3C). However, cells expressing the phosphorylation-defective Y518F–ICAM-1 mutant showed neither ICAM-1 nor Src Tyr419 phosphorylation after ICAM-1 crosslinking (Figure 3C). Thus, intracellular C-terminal ICAM-1 tyrosine Tyr518 phosphorylation plays an important role in Src signal amplification downstream of ICAM-1 crosslinking and activation.
SHP-2 phosphatase binds to the ICAM-1 ITAM motif7 and hence may play a role in Src activation downstream of ICAM-1. ICAM-1 crosslinking-induced Src phosphorylation was analyzed by Western blotting to determine whether SHP-2 is required for Src activation. HUVECs were cotransfected with WT mouse ICAM-1 and WT- or phosphatase-defective Cys463Ser–SHP-2 mutant (C463S–SHP-2). After ICAM-1 crosslinking in ECs expressing WT–SHP-2, we observed increased Src Tyr419 phosphorylation, whereas a much weaker response was observed in cells expressing C463S–SHP-2 (Figure 3D). Phosphorylation of human Src Tyr530, the inhibitory phospho-tyrosine in the Src C-terminal regulatory domain,27,28 decreased in cells expressing WT–SHP-2 after addition of ICAM-1 crosslinking mAb but not in cells expressing C463S–SHP-2 (Figure 3D). Cells expressing the catalytically inactive C463S SHP-2 mutant also showed less Src Tyr419 auto-phosphorylation and no change in inhibitory Src Tyr530 dephosphorylation compared with that in cells expressing WT–SHP-2 (Figure 3D). Both Tyr419 and Tyr530 are important for accurately assessing Src activity by phospho-Src immunoblot analysis27,28 ; thus, a ratio of active site and inhibitory site Src tyrosine phosphorylation (pTyr419/pTyr530) was calculated. As shown in Figure 3D, the ratio increased on ICAM-1 crosslinking in cells transfected with WT–SHP-2 but did not change significantly in cells transfected with dominant-negative SHP-2 mutant (Figure 3D). We also observed that phosphorylation of ICAM-1 Tyr518 induced by crosslinking increased in cells expressing WT–SHP-2 (Figure 3D). In contrast, there was no change of ICAM-1 Tyr518 phosphorylation induced by the crosslinking protocol in cells expressing the C463S–SHP-2 mutant (Figure 3D), indicating less Src activity in these cells. Taken together, these data indicate SHP-2 activity is required for ICAM-1 crosslinking-induced Src activation and ICAM-1 phosphorylation, most likely via SHP-2 mediated dephosphorylation of Src inhibitory Tyr530.
To determine the mechanism by which SHP-2 mediates ICAM-1 crosslinking-induced Src activation, we examined the interaction between SHP-2 and ICAM-1 by coimmunoprecipitation in HEK cells transduced with WT mouse ICAM-1. ICAM-1 association with SHP-2 was reduced after ICAM-1 crosslinking (supplemental Figure 2A). Both Y518F and Y518D (phosphor-defective and phosphor-mimicking ICAM-1 mutants) showed reduced coimmunoprecipitation (supplemental Figure 2B) with SHP-2 compared with WT–ICAM-1. Taken together, these data suggest that the hydroxyl group of ICAM-1 Y518 may be involved in coordinating SHP-2 binding within the ITAM motif, and that crosslinking-induced activation of ICAM-1 leads to displacement and activation of SHP-2 and dephosphorylation of the Src inhibitory phospho-Tyr530 residue.
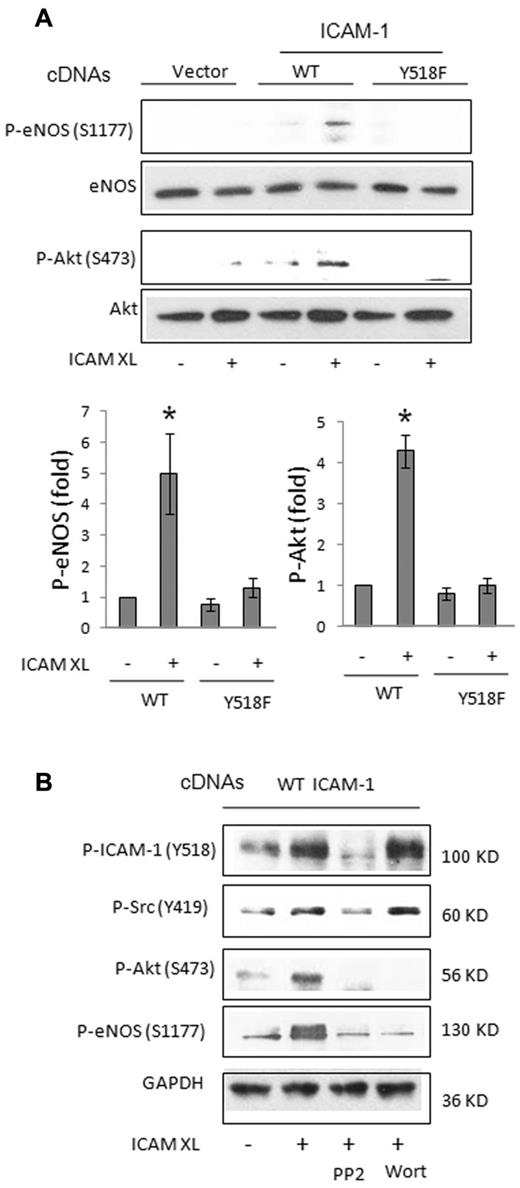
ICAM-1 activation of the Src-Akt-eNOS pathway
We next examined eNOS Ser1177 phosphorylation in ICAM-1–transfected HUVECs after ICAM-1 crosslinking to address the possible involvement of eNOS downstream of ICAM-1 activation in human ECs. ICAM-1 crosslinking induced both eNOS phosphorylation at Ser1177 and Akt phosphorylation at Ser473 in cells transduced with WT–ICAM-1, whereas no effect was observed in cells expressing the phospho-defective ICAM-1 mutant (Figure 4A). eNOS is known to be phosphorylated at Ser1177 by Akt29 downstream of PI3K and Src,21 and also by AMP kinase (AMPK).18,30 Thus, we next determined the effect of Src inhibitor PP2 (10μM), PI3K inhibitor wortmannin (100nM) on ICAM-1 induced Src, Akt, and/or eNOS phosphorylation. As shown in Figure 4B, phosphorylation of ICAM-1 and Src were blocked by Src inhibitor PP2, but not by PI3K inhibitor wortmannin. In contrast, phosphorylation of Akt Ser473 and eNOS Ser1177 was blocked by both PP2 and wortmannin (Figure 4B), indicating that Akt and eNOS activation lies downstream of ICAM-1–induced Src and PI3K activation.
Activation of eNOS and Akt induced by ICAM-1 crosslinking. (A) In transfected HUVECs, ICAM-1 crosslinking (XL) induced the phosphorylation of eNOS at S1177 and Akt at S473, which were detected using phospho-specific antibodies. (B) Effect of Src inhibitor PP2 (10μM) and PI3K inhibitor wortmannin (Wort, 100nM) on the phosphorylation of ICAM-1, Src, Akt, and eNOS. Phosphorylation of ICAM-1, Src, and Cav-1 were sensitive to PP2, whereas the phosphorylation of Akt and eNOS was sensitive to both PP2 and wortmannin. *P < .05 versus all others.
Activation of eNOS and Akt induced by ICAM-1 crosslinking. (A) In transfected HUVECs, ICAM-1 crosslinking (XL) induced the phosphorylation of eNOS at S1177 and Akt at S473, which were detected using phospho-specific antibodies. (B) Effect of Src inhibitor PP2 (10μM) and PI3K inhibitor wortmannin (Wort, 100nM) on the phosphorylation of ICAM-1, Src, Akt, and eNOS. Phosphorylation of ICAM-1, Src, and Cav-1 were sensitive to PP2, whereas the phosphorylation of Akt and eNOS was sensitive to both PP2 and wortmannin. *P < .05 versus all others.
Studies by Martinelli et al revealed that ICAM-1 monoclonal Ab alone activates eNOS via AMPK-dependent signaling in rat brain endothelial cells.18 Thus, we also examined whether primary antibody alone compared with crosslinking ICAM-1 (using both a primary Ab and secondary crosslinking Ab) induced eNOS phosphorylation and whether AMPK inhibition by 5-iodotubercidin31 blocks eNOS phosphorylation. Incubation with primary antibody alone had no effect on eNOS phosphorylation, and 5-indotubercidin reduced ICAM-1 induced eNOS phosphorylation (supplemental Figure 1B). Thus, the mechanism of mouse ICAM-1 induced eNOS activation appears to be dependent on PI3K and Akt, and to some extent by AMPK, whereas in rat brain endothelial cell eNOS activation occurs via AMPK-dependent signaling.18
ICAM-1 activation induces NO production
We next measured ICAM-1–induced eNOS-derived NO production to assess the functional significance of eNOS phosphorylation via the Src/PI3K/Akt pathway. HUVECs transfected with WT- or the Y518F–ICAM-1 mutant were subjected to ICAM-1 crosslinking and real-time NO production was measured by porphyrinic electrode as described.21 We observed NO production in WT–ICAM-1–transfected cells but not in cells transfected with the phospho-defective ICAM-1 mutant (Figure 5A). We also determined whether activation of PMNs layered on ECs (ratio of 10 PMNs/1 EC) stimulated NO production in an ICAM-1–dependent manner. Mouse PMNs activated with 10μM fMLP were added to HUVEC cultures transfected with WT mouse ICAM-1 or phospho-defective mouse ICAM-1 mutant, and NO was measured. Activated PMNs added to ECs transfected with the phospho-defective ICAM-1 mutant failed to induce NO production, whereas WT–ICAM-1 produced a 2-fold increase in NO production via eNOS (supplemental Figure 2C). To determine the role of Src and PI3K signaling in mediating ICAM-1–mediated NO production, PP2 and wortmannin were added to HUVECs and NO production was measured 30 minutes after crosslinking. We observed that ICAM-1 activation-dependent NO production required the Src-PI3K-Akt signaling pathway (Figure 5B) consistent with the eNOS Ser1177 phospho-immunoblots (Figure 4B).
ICAM-1 stimulated NO production and PMN transmigration are dependent on Src, Akt, and eNOS. (A) ICAM-1 crosslinking (XL) induced NO production in HUVECs. NO production was measured in the medium during secondary antibody incubation (30 minutes) using a porphyrinic NO electrode. (B) ICAM-1 XL-induced NO production was sensitive to both PP2 and wortmannin (Wort). Data are mean ± SD of triplicates from a representative experiment that was repeated 3 times with equivalent results. (C) ICAM-1–mediated PMN transendothelial cell migration was assessed in HUVECs expressing empty vector, WT–ICAM-1, or Y518F–ICAM-1 (top panels) or after treatment with pharmacologic inhibitors (bottom panels). Mouse PMNs labeled with fluorescent dye were added to transfected HUVEC monolayers grown to confluence in tissue culture wells for adhesion assays or Transwell filter inserts to assess transmigration. Migration was triggered by the addition of 10nM fMLP to the bottom chamber, and then the PMN fluorescence that accumulated was measured after 3 hours. (D) HUVEC monolayers were pretreated with L-NAME (1mM), PP2 (10μM), or wortmannin (100nM) for 30 minutes. Later, 10nM fMLP was added to the bottom chamber of Transwell plates to initiate migration. ICAM-1–mediated PMN adhesion was increased by L-NAME and wortmannin, whereas transmigration was blocked by PP2, wortmannin, and L-NAME. Data are the mean ± SD of 4 or 5 experiments. *P < .05 versus Ctrl (A-D); P < .05 versus WT (C-D).
ICAM-1 stimulated NO production and PMN transmigration are dependent on Src, Akt, and eNOS. (A) ICAM-1 crosslinking (XL) induced NO production in HUVECs. NO production was measured in the medium during secondary antibody incubation (30 minutes) using a porphyrinic NO electrode. (B) ICAM-1 XL-induced NO production was sensitive to both PP2 and wortmannin (Wort). Data are mean ± SD of triplicates from a representative experiment that was repeated 3 times with equivalent results. (C) ICAM-1–mediated PMN transendothelial cell migration was assessed in HUVECs expressing empty vector, WT–ICAM-1, or Y518F–ICAM-1 (top panels) or after treatment with pharmacologic inhibitors (bottom panels). Mouse PMNs labeled with fluorescent dye were added to transfected HUVEC monolayers grown to confluence in tissue culture wells for adhesion assays or Transwell filter inserts to assess transmigration. Migration was triggered by the addition of 10nM fMLP to the bottom chamber, and then the PMN fluorescence that accumulated was measured after 3 hours. (D) HUVEC monolayers were pretreated with L-NAME (1mM), PP2 (10μM), or wortmannin (100nM) for 30 minutes. Later, 10nM fMLP was added to the bottom chamber of Transwell plates to initiate migration. ICAM-1–mediated PMN adhesion was increased by L-NAME and wortmannin, whereas transmigration was blocked by PP2, wortmannin, and L-NAME. Data are the mean ± SD of 4 or 5 experiments. *P < .05 versus Ctrl (A-D); P < .05 versus WT (C-D).
ICAM-1–induced Src-Akt-eNOS signaling is required for PMN transendothelial migration
We next determined whether expression of Y518F, the phospho-defective ICAM-1 mutant, affects PMN adhesion or transmigration through transduced human EC monolayers. ICAM-1–dependent adhesion of mouse PMNs to EC monolayers expressing WT- or Y518F-mouse ICAM-1 was not different (supplemental Figure 2D). However, as shown in the transmigration assay, Y518F–ICAM-1 expression resulted in a 50% decrease in PMN migration relative to that observed in cells expressing WT–ICAM-1 (Figure 5C). WT–ICAM-1–dependent PMN transmigration was also blocked by PP2, wortmannin, and L-NAME (Figure 5D), suggesting that the Src-PI3K-Akt-eNOS pathway plays an important role in the mechanism of ICAM-1–dependent PMN transmigration.
PECAM-1 phosphorylation and binding activity downstream of ICAM-1 and eNOS
To understand how eNOS activation regulates PMN transmigration, we examined the role of the ICAM-1/Src/eNOS pathway in the regulation of cell surface expression and phosphorylation of PECAM-1 Tyr686. It was previously reported that PECAM-1, which is essential for leukocyte transmigration,6,32 can be phosphorylated on 2 tyrosine residues within the intracellular C-terminal domain.33,34 In transfected HUVECs, crosslinking of mouse WT–ICAM-1, but not that of the phospho-defective Y518F– ICAM-1 mutant, induced the phosphorylation of endogenous human PECAM-1 Tyr686 (Figure 6A-B). Furthermore, ICAM-1 crosslinking-induced PECAM-1 phosphorylation was blocked by PP2 and L-NAME, suggesting that ICAM-1 activation-dependent phosphorylation of PECAM-1 is the consequence of Src and eNOS (Figure 6B). Moreover, in eNOS−/− mouse lungs, basal and carrageenan-stimulated PECAM-1 Tyr686 phosphorylation was significantly reduced compared with that observed in WT mouse lungs (Figure 6C), suggesting that activation of PECAM-1 downstream of ICAM-1 and eNOS is an essential component of the inflammatory response in vivo.
Regulation of PECAM-1 phosphorylation and binding activity by ICAM-1 and eNOS. (A) ICAM-1 crosslinking induced phosphorylation of PECAM-1. HUVECs were transfected with empty vector, WT ICAM-1, and Y518F mutant ICAM-1 cDNAs and subjected to crosslinking assay. The phosphorylation of PECAM-1 at Y686 was examined. (B) ICAM-1 crosslinking-induced PECAM-1 phosphorylation was inhibited by PP2 (10μM) and L-NAME (1mM) in HUVECs transfected with WT ICAM-1. (C) Phosphorylation of PECAM-1 was diminished in eNOS−/− mouse lungs. (D) ICAM-1 crosslinking-induced increase in PECAM-1 binding activity. HUVECs transfected as above in 96-well plates were subjected to ICAM-1 crosslinking and PECAM-1 mAb antibody binding and cell-attached ELISA. After ICAM-1 crosslinking for 1 hour, the cells were subjected to the PECAM-1 mAb binding assay. The cells were washed and incubated with the PECAM-1 mAb diluted in medium (10 μg/mL) at 4°C for 1 hour. The cells were then fixed and incubated with HRP-labeled secondary Ab. Data are mean ± SD of triplicate samples from 1 of 3 individual experiments that yielded equivalent results. *P < .05 versus control.
Regulation of PECAM-1 phosphorylation and binding activity by ICAM-1 and eNOS. (A) ICAM-1 crosslinking induced phosphorylation of PECAM-1. HUVECs were transfected with empty vector, WT ICAM-1, and Y518F mutant ICAM-1 cDNAs and subjected to crosslinking assay. The phosphorylation of PECAM-1 at Y686 was examined. (B) ICAM-1 crosslinking-induced PECAM-1 phosphorylation was inhibited by PP2 (10μM) and L-NAME (1mM) in HUVECs transfected with WT ICAM-1. (C) Phosphorylation of PECAM-1 was diminished in eNOS−/− mouse lungs. (D) ICAM-1 crosslinking-induced increase in PECAM-1 binding activity. HUVECs transfected as above in 96-well plates were subjected to ICAM-1 crosslinking and PECAM-1 mAb antibody binding and cell-attached ELISA. After ICAM-1 crosslinking for 1 hour, the cells were subjected to the PECAM-1 mAb binding assay. The cells were washed and incubated with the PECAM-1 mAb diluted in medium (10 μg/mL) at 4°C for 1 hour. The cells were then fixed and incubated with HRP-labeled secondary Ab. Data are mean ± SD of triplicate samples from 1 of 3 individual experiments that yielded equivalent results. *P < .05 versus control.
Homophilic interaction between leukocyte PECAM-1 and endothelial cell PECAM-1 is thought to mediate leukocyte transmigration.6 Thus, we next examined the effect of ICAM-1 activation on PECAM-1 binding activity in cultured endothelial monolayers. Mouse ICAM-1 expressing HUVECs were treated with ICAM-1 crosslinking mAb and assayed for cell surface PECAM-1 binding activity by a cell-attached ELISA assay.8 Figure 6D shows that ICAM-1 activation significantly increased PECAM-1 mAb binding activity. Moreover, HUVECs expressing the phosphorylation-defective mouse ICAM-1 mutant (Tyr518Phe) showed significantly reduced PECAM-1 binding activity compared with WT–ICAM-1. Interestingly, ICAM-1 activation-dependent increase in PECAM-1 binding activity was not blocked by L-NAME (data not shown). Thus, NO appears to regulate PECAM-1 phosphorylation and PMN transmigration but does not appear to play a role in the mechanism of increased PECAM-1 mAb binding activity.
Discussion
In this report, we show an important functional relationship between ICAM-1 activation and PECAM-1 binding activity and subsequent PMN transendothelial migration during inflammation (ie, ICAM-1 activation-dependent Src and NO signaling in human ECs increases PECAM-1–dependent PMN transmigration). ICAM-1 was demonstrated to function through the phosphorylation of its Tyr518 residue that leads to activation of tyrosine phosphatase SHP-2, which, via dephosphorylation of Src inhibitory Tyr530, increased Src activity. Src activation by this mechanism induced PECAM-1 Tyr686 phosphorylation and also stimulated PI3K, Akt, and eNOS activation. The Src-Akt-eNOS signaling initiated by activation of mouse ICAM-1 expressed in human endothelial cells, which we used to assess the direct effects of ICAM-1 mediated signaling by avoiding Src activation induced by cytokines, such as TNF-α,8 was demonstrated to be essential for PECAM-1–dependent PMN transmigration. We also showed in the mouse model of carrageenan-induced lung inflammation the pathophysiologic relevance of ICAM-1–induced PECAM-1 activation in mediating inflammation. In addition to ICAM-1, ICAM-2 and VCAM-1 are also involved in leukocyte adhesion to endothelial cells.25 For example, in T-cell transmigration, ICAM-1 and VCAM-1 mediate T-cell arrest, whereas ICAM-1 and ICAM-2 mediate T-cell crawling to permissive sites for diapedesis.35 Therefore, our studies do not exclude the possibility that ICAM-2 and VCAM-1 also participate in ICAM-1 activation-dependent PMN transmigration.
Pleural space injection of carrageenan increased ICAM-1 expression and phosphorylation, as well as activation of Src and eNOS, leading to increased infiltration of PMNs in the lung. In this model, L-NAME treatment or eNOS deletion reduced lung PMN infiltration in support of cultured EC data showing that ICAM-1–activated NO production via enhanced eNOS Ser1177 phosphorylation downstream of Akt plays a key role in the mechanism of PMN transmigration in vivo. WT–ICAM-1 and phospho-defective Y518F mutant ICAM-1 expressed in ECs both supported PMN adhesion, whereas Y518F–ICAM-1 failed to induce PMN transmigration, suggesting that ICAM-1 phosphorylation-dependent signaling is required for PMN transmigration. Inhibition of the Src-Akt-eNOS pathway also blocked PMN transmigration without reducing PMN adhesion to ECs. In eNOS−/− mice in which we observed reduced PMN infiltration (total lung MPO activity) and transmigration (bronchoalveolar lavage PMN cell counts), both basal and carrageenan-induced ICAM-1 expression was greater compared with WT mice, consistent with the negative regulatory role of NO on NF-κB signaling36 and ICAM-1 gene transcription.37 We also observed reduced PMN lung infiltration in iNOS−/− mice (supplemental Figure 3A), as reported previously by Cuzzocrea et al.24 In addition, eNOS inhibitor L-NAME was able to further reduce PMN infiltration in iNOS−/− mice (supplemental Figure 3B), suggesting that both eNOS- and iNOS-derived NO production play important roles in the inflammatory response induced by carrageenan.
Antibody-induced ICAM-1 crosslinking activates Src15 ; however, the mechanism of crosslinking induced Src activation is unclear. In our cotransfection experiments using WT or phosphatase-defective SHP-2 mutant, we showed that phosphatase activity is required for ICAM-1 crosslinking-induced Src activation. Furthermore, we observed decreased Src Tyr530 phosphorylation after ICAM-1 crosslinking, which was abolished in cells expressing the phosphatase-dead SHP-2 mutant. These findings demonstrate that SHP-2 increases Src activity by de-phosphorylating the Src inhibitory Tyr530 residue and thereby dis-inhibiting tyrosine kinase activity. This function of SHP-2 probably becomes apparent after ICAM ligation (or crosslinking) by displacement from the C-terminal ICAM-1 ITAM motif.7 Displacement and activation of SHP-2 then dephosphorylates and activates Src C-terminal Tyr530.15 Coimmunoprecipitation results suggest that basal SHP-2 association with ICAM-1 is reduced after ICAM-1 crosslinking, supporting the hypothesis that SHP-2 release from ICAM-1 mediates the activation of Src. ICAM-1 was previously demonstrated to stimulate SHP-2–mediated dephosphorylation of human Src Tyr530 and induce Src activation.38 The present study identifies a novel feed-forward Src signaling mechanism leading to PMN transmigration induced by phospho–ICAM-1–dependent SHP-2–mediated dephosphorylation of Src-negative regulatory Tyr530 and subsequent Src Tyr419 auto-phosphorylation. This signaling culminates in Src-dependent PECAM-1 Tyr686 phosphorylation and enhanced PECAM-1–dependent transmigration of PMN.
PI3K is also a key downstream effector of Src.39 Here we demonstrate that activation of eNOS induced by ICAM-1 crosslinking is mediated via Src-PI3K-Akt signaling. In these studies, ICAM-1 crosslinking induced Akt phosphorylation, eNOS phosphorylation, and NO production. Both Src and PI3K inhibition prevented eNOS and Akt phosphorylation and NO production, showing that eNOS activation occurs downstream of Src and PI3K. In these studies, compared with the study by Martinelli et al,18 primary antibody alone did not induce eNOS phosphorylation or NO production. Similar to that reported previously,18 eNOS phosphorylation was blocked in part by AMPK inhibition although we also observed eNOS phosphorylation to be blocked fully by PI3K inhibition, suggesting that eNOS activation downstream of ICAM-1 occurs through both PI3K/Akt- and AMPK-dependent pathways. Thus, the mechanism of eNOS activation varies slightly between rat brain endothelial cells and HUVECs expressing mouse ICAM-1. Nevertheless, both studies suggest that ICAM-1–mediated eNOS activation may be a common mechanism regulating leukocyte transmigration in the lung and brain.
The finding that ICAM-1–activated NO signaling contributes to the mechanism of PMN transmigration and lung PMN sequestration is seemingly contrary to the reported inhibitory role of NO on PMN migration,40 which has been attributed to its ability to dampen PMN superoxide production.41 As migration of PMNs was also shown to be dependent on NO concentration,42 it is possible that the amount of NO generated on ICAM-1 activation is sufficient to induce PMN migration but not to inhibit PMN NADPH oxidase. Importantly, in our studies, ICAM-1–dependent generation of NO did not inhibit PMN adhesion to endothelial cells. Rather, NO production increased PMN transmigration, consistent with previous observations.43,44 The finding that ICAM-1 knockout mice exhibited reduced production of NO45,46 also fits with our observation that ICAM-1 signaling plays a key role in regulating NO production by stimulating the phosphorylation of eNOS.
An unanswered question in the field has been whether ICAM-1 activation regulates the function of PECAM-1 as an adhesive EC protein required for PMN transmigration. We observed that ICAM-1 activation increases the phosphorylation of PECAM-1 Tyr686 via the Src-Akt-eNOS pathway because PECAM-1 phosphorylation at this residue was blocked by L-NAME and was abolished in eNOS−/− mouse lungs. The antibody used for detecting PECAM-1 phosphorylation only recognizes phosphorylated Tyr686 (this residue is equivalent to Tyr713 in full-length signal peptide-containing PECAM-1). It is currently not known whether Src activation by the mechanism described can also regulate the phosphorylation of PECAM-1 Tyr663, which was previously demonstrated to be important for leukocyte transmigration.5,47,48 Phosphorylation of the Tyr663 residue was suggested to be essential for PMN transmigration by regulating the location and trafficking of PECAM-1 in endothelial cells.5
The mechanism by which eNOS activation and NO production increase PECAM-1 phosphorylation and homotypic PECAM-1 adhesion is not clear. Our data suggest that eNOS activity is required for PECAM-1 phosphorylation but not for increased cell surface PECAM-1 expression/binding activity. Interestingly, eNOS and PECAM-1 were previously reported to form a complex49 ; thus, it is tempting to speculate that localized activation of eNOS and resultant NO production near the lateral membrane may regulate PMN transmigration via PECAM-1–mediated binding of PMNs.
Leukocyte PECAM-1 homophilic adhesion to endothelial cell PECAM-1 is required for leukocyte transmigration.6 An increase in PECAM-1 binding activity downstream of ICAM-1 suggests that firm adhesion of PMN via ICAM-1 promotes PMN transmigration in association with PECAM-1 located in the lateral membrane. The increase of available PECAM-1 mAb binding sites may be the result of an increase in cell surface PECAM-1 expression or increased adhesivity of available PECAM-1. Phosphorylation of PECAM-1 may lead to increased trafficking of PECAM-1 to the lateral membrane from stored pools in the “lateral membrane recycling compartment”6 or perhaps to PECAM-1 clustering-induced increase in binding avidity similar to that recently described for ICAM-1.8 As the increase in PECAM-1 binding was much less in HUVECs expressing phosphorylation-defective ICAM-1 mutant, ICAM-1 phosphorylation and downstream Src and eNOS signaling appear to play an important role in the mechanism of increased PECAM-1 binding activity and transendothelial migration of PMNs. However, although L-NAME did not block the increase in PECAM-1 binding activity, it did significantly reduce PECAM-1 phosphorylation and PMN transmigration, and there was significantly less PMN infiltration in eNOS−/− mouse lungs after carrageenan-induced pleurisy. Thus, Src appears to regulate PECAM-1–mediated expression/adhesivity, whereas NO functions independent of PECAM-1–mediated adhesion to facilitate PMN transmigration. Taken together, these data indicate that ICAM-1 activation of Src induces eNOS-dependent regulation of PECAM-1 phosphorylation as well as PMN transmigration, and eNOS-independent regulation of PECAM-1 binding activity.
Interestingly, PECAM-1 was also shown to counteract ICAM-1–mediated signaling.50 Thus, signaling via ICAM-1 and PECAM-1 activation may be bidirectional and complementary, thereby dynamically regulating leukocyte transmigration via feed-forward signaling and PECAM-1 adhesivity and feedback inhibition of ICAM-1 expression and signaling. During an inflammatory response, engagement of ICAM-1 signals Src and eNOS activation, which together promote PECAM-1–dependent PMN transmigration (Figure 7). Src phosphorylation of PECAM-1 and NO production were associated with increased PECAM-1 binding activity and PMN transmigration, whereas NO also limited ICAM-1 expression and thereby PMN adhesion, which may prevent excessive neutrophilic inflammation. These results raise the prospect of manipulating inappropriate PMN trafficking by interfering with ICAM-1–induced Src and eNOS signaling, thereby mitigating tissue inflammation dependent on PECAM-1–mediated transmigration.
Schematic showing ICAM-1 activation-dependent signaling leading to increased PECAM-1 binding activity and PMN transmigration. On ligation, ICAM-1–associated SHP-2 induces Src activation, PI3K and Akt signaling, and eNOS activation. Src and NO signals mediate increased PECAM-1 binding activity and PMN transendothelial migration.
Schematic showing ICAM-1 activation-dependent signaling leading to increased PECAM-1 binding activity and PMN transmigration. On ligation, ICAM-1–associated SHP-2 induces Src activation, PI3K and Akt signaling, and eNOS activation. Src and NO signals mediate increased PECAM-1 binding activity and PMN transendothelial migration.
The online version of this article contains a data supplement.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 USC section 1734.
Acknowledgments
The authors thank Maricela Castellon and David Visintine for excellent technical assistance, mouse husbandry, and development of the carrageenan pleurisy and lung inflammation mouse model.
This work was supported by the National Institutes of Health National Heart, Lung, and Blood Institute (grant P01 HL60678, R.D.M., R.A.S., and A.B.M.; grant R01 HL71626, R.D.M.; grant R01 HL046849 and R37 HL064774, W.A.M.).
National Institutes of Health
Authorship
Contribution: G.L. designed research, performed experiments, analyzed data, made the figures, and wrote the paper; A.T.P. analyzed data, made the figures, and wrote the paper; Z.C. and V.M.B. performed experiments and analyzed data; S.M.V. and R.A.S. designed research and analyzed data; and W.A.M., A.B.M., and R.D.M. designed research, analyzed data, and wrote the paper.
Conflict-of-interest disclosure: The authors declare no competing financial interests.
Correspondence: Richard D. Minshall, Department of Pharmacology (m/c 868), University of Illinois, College of Medicine at Chicago, 835 S Wolcott Ave, Chicago, IL 60612; e-mail: rminsh@uic.edu.