Abstract
Abstract  596
596
Large population-based studies have demonstrated a significant improvement in survival (OS) for patients (pts) with multiple myeloma (MM) over time since the mid-1990s. The improvement has mostly affected younger patients suggesting a beneficial impact of AHCT. The availability of novel drugs within the last decade and their impact on the utilization and outcomes of AHCT recipients is unknown.
We retrospectively reviewed the characteristics and outcomes of 20,278 patients undergoing AHCT within 12 months of diagnosis in USA and Canada and reported to CIBMTR in the periods of 1995–1999 (n=2226), 2000–2004 (n=6408) and 2005–2010 (n=11644) including a subgroup of 4373 individuals with detailed patient, disease and treatment information. We subsequently compared survival and analyzed patient, disease and treatment characteristics across the three periods with the time period serving as a surrogate for pre- and post-transplant exposure to novel agents.
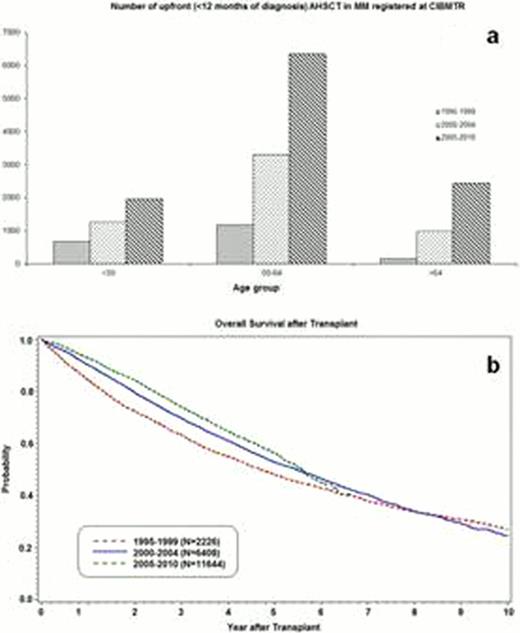
Across the 3 time periods, there was a marked increase in the number of upfront transplants across all age groups (Figure 1a). Patients receiving upfront HSCT in the more recent period were older, less likely to have stage 3 MM at diagnosis and more likely to have received thalidomide (<1 % vs. 22% vs. 52%), lenalidomide (0% vs. <1% vs. 21%) or bortezomib (0% vs. 2% vs. 35%) and have chemosensitive disease at the time of AHCT. The proportion of African-American patients remained low and stable across the three periods (14 vs. 13 vs. 15%). Over the 3 periods, there was a decrease in chemotherapy based stem cell mobilization and increase of single agent G-CSF based mobilization (24% vs. 24% vs. 41%). The use of single agent Melphalan conditioning increased from 54% in 1995–1999 to nearly 100% in the latest period concomitant with near disappearance of total body irradiation-based and multi-drug conditioning regimens. Compared with 1995–99 cohort, survival was superior in the 2000–04 and 2005–09 cohorts at 24 (72% vs. 79% vs. 84%, P<0.001), 48 (54% vs. 60% vs. 64%, P<0.001) and 60 months (47% vs. 52% vs. 55%, P<0.001) (Figure 1b). In multivariate analysis, we found that transplant in the 2000–04 period (HR=0.77, 95% C.I. 0.67–0.89) or in the 2005–10 period (HR=0.68, 95% C.I. 0.59–0.79) along with Karnofsky performance score of 80–100 (HR=0.59, 95% CI 0.51–0.70) and chemosensitivity (HR= 0.76, 95% C.I. 0.66–0.87) were associated with lower risk of death. Factors associated with higher risk of death were age 50–65 (HR=1.29 95% 1.13–1.47), age 65–80 (HR=1.45, 1.23–1.72), Durie-Salmon or ISS stage III at diagnosis (HR 1.56, 95% C.I. 1.39–1.76) and more than one prior line of therapy (HR=1.15, 95% C.I. 1.03–1.28). In comparison to patients transplanted in 1995–99, post relapse survival was superior for patients transplanted in 2000–04 and 2005–10 at 24 months (58% vs. 65% vs. 72%, P=0.005 and <0.001 respectively) and 48 months (33% vs. 39% vs. 40%, P=0.023 and 0.033 respectively). The use of maintenance therapy has changed with 27% in 1995–99 receiving planned interferon vs. 23% in 2005–09 receiving planned thalidomide, lenalidomide or bortezomib maintenance.
Utilization of upfront AHCT is increasing in the USA, particularly in older patients. Improvement in survival for MM patients seen in population studies results not only from greater utilization of AHCT but also from the improvement in outcomes after AHCT and a significant recent improvement in post-relapse survival. Pre- and post-transplant exposure to novel agents likely contributes to survival. AHCT and novel agents are complementary and should be combined for the optimal management of newly diagnosed MM.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This icon denotes a clinically relevant abstract