Abstract
Abstract  4217
4217
AHCT improves survival (OS) in newly diagnosed MM patients (pts) in large randomized trials. These trials have limited eligibility to younger, healthier pts. Selection of older pts and those with co-morbid illness for AHCT is problematic. HCT-CI, originally developed as predictor of post-allogeneic transplant outcomes, maybe valuable in stratifying risk of transplant related mortality (TRM) risk and OS in the AHCT setting. We investigated the relative impact of HCT CI along with other patient and MM related variables on outcomes after AHCT in a large cohort of transplant recipients.
Outcomes of 1156 MM pts receiving AHCT after high dose Melphalan (MEL) between 2007 and 2010 reported to the CIBMTR (Center for International Blood and Marrow Transplant Research) were analyzed. HCTCI scores and individual comorbidities were prospectively reported at time of AHCT. Median follow up of survivors was 26 month. The impact of HCTCI and other potential prognostic factors including Karnofsky performance status (KPS) on OS were studied in multivariate Cox regression models.
HCTCI score was 0, 1, 2, 3, >3 in 42%, 18%, 13%, 13% and 14% respectively. Most common co-morbidities included pulmonary, diabetes, obesity, psychiatric, cardiac, renal and prior solid tumor. Using consolidated HCTCI scores, patients were stratified initially into 3 risk groups – HCTCI 0 (42%) vs. HCTCI 1–2 (32%) vs. HCTCI >2 (26%). Males and Caucasians were more likely to have greater HCTCI score. Higher HCTCI was associated with lower KPS <90 (33% in HCTCI 0 cohort vs. 50% in HCTCI >2). HCTCI score >2 was associated with MEL dose reduction to 140 mg/m2 (22% vs. 10% in score 0 cohort). Cytogenetic risk and MM related factors were not correlated with HCTCI.
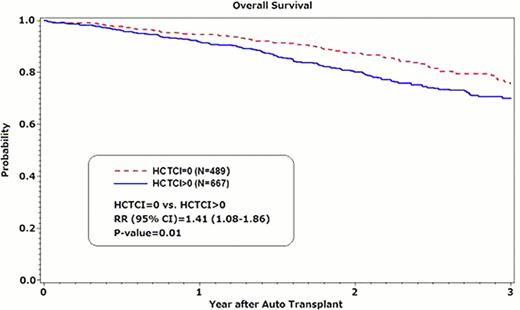
TRM at 12 month was 2%, 2%, and 3% for 3 risk groups. With extremely few TRM events, multivariate analysis did not suggest an impact of HCTCI. OS was 95%, 92%, 92% at 1 year and 87%, 81%, 80% at 2 year, respectively. OS was inferior for HCTCI >2 cohort (RR of death 1.48, p=0.02) and HCTCI cohort 1–2 (RR 1.37, p=0.04) compared with HCTCI 0 cohort. There was no significant difference in OS between HCTCI >2 vs. HCTCI 1–2 (p=0.64). Therefore the latter 2 groups were combined as the HCTCI >0 cohort [N=667] and compared with HCTCI=0 [N=489] in multivariate models. HCTCI >0 predicted inferior OS (RR of death= 1.41, p=0.01). Other significant predictors of inferior survival were KPS <90 (RR of death 1.61, p<0.01), IgA subtype (RR 1.64, p<0.01), >1 pretransplant regimen (RR 1.47, p<0.01), resistant MM at AHCT (RR 1.78, p<0.01). Major cause of death in both groups was progressive MM.
In clinical practice, higher HCTCI score was associated with MEL dose reduction. Mortality after AHCT is predominantly related to MM progression/relapse with low incidence of TRM. Higher HCTCI scores were independently associated with inferior OS. KPS remains an important tool for risk stratification.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This icon denotes a clinically relevant abstract