Abstract
Abstract 3611
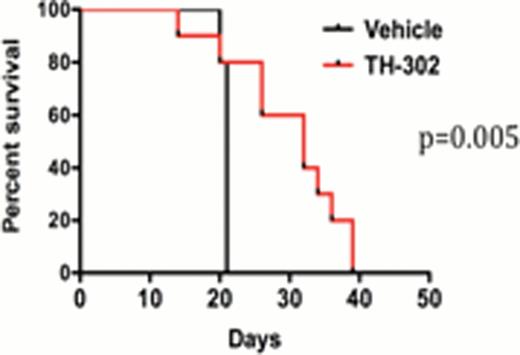
Recent evidence has demonstrated the bone marrow (BM) microenvironment, the principal site of acute myeloid leukemia (AML) initiation and expansion, is characterized by intrinsically low oxygen tension. Theoretically, such microenvironmental changes may lead to the selective outgrowth of AML clones which are “better adapted” to survive within a severely hypoxic microenvironment and/or may confer resistance to chemotherapeutic agents, similar to solid tumor cells. We report here that human AML cells (HL60, ML-2) cultured under chronic hypoxic conditions mimicking the marrow microenvironment (1% O2, 72 hours) exhibited reduced sensitivity to cytarabine-induced apoptosis as compared with normoxic cells, as determined by flow cytometric analysis, western blot analysis, and cell viability assays. Similar results were noted in primary AML samples treated with cytarabine under normoxic and hypoxic conditions in colony formation assays (n=3 samples, p=0.01). In order to improve upon chemotherapy outcomes, we investigated the effects of TH-302, a hypoxia-activated bromo-isophosphoramidate mustard prodrug, which is currently undergoing clinical trial evaluation in multiple tumor types. Treatment of AML cell lines (HL60, HEL) and primary AML samples with TH-302 (at doses ranging from 0.1– 5 mM, p values ranging from <0.05–0.0001) resulted in dose- and hypoxic-dependent inhibition of AML proliferation and apoptosis. In vivo TH-302 treatment significantly decreased disease burden, as measured by total animal bioluminescence, and prolonged overall survival in two systemic human AML xenograft models (HEL-luciferase, HL60-luciferase) (Figure 1). Immunohistochemical studies demonstrated that TH-302 treatment reduced numbers of hypoxic (pimonidazole-positive) cells within the leukemic marrow microenvironment. Because prior data in animal models has shown that AML progression within the marrow is associated with expansion of hypoxic BM areas, we examined the effects of TH-302 treatment on systemic AML growth when initiated early (prior to AML inoculation) or late (several days following AML engraftment) in the disease process. TH-302 was equally effective at both time points. Although anti-vascular therapy has been shown to enhance tumor hypoxia in other cancer types, we noted no synergistic or additive in vivo effects when TH-302 therapy was combined with sorafenib, an inhibitor of vascular endothelial growth factor receptors (VEGFR), in our models. TH-302 therapy administered for two weeks in non-leukemic and leukemia-engrafted mice was not associated with hematologic toxicities. In summary, our results demonstrate the anti-leukemic activity of TH-302 in preclinical AML models and suggest that the efficacy of this and other drugs for AML therapy may be uniquely affected by the BM microenvironment. Further clinical development of TH-302 and other hypoxia-targeted drugs for AML therapy are warranted. Based on our data, higher TH-302 doses and/or chronic drug administration may be needed for optimal in vivo anti-leukemic activity.
Effects of TH-302 treatment on systemic AML growth and overall survival in HL60-luciferase engrafted SCID mice.
Effects of TH-302 treatment on systemic AML growth and overall survival in HL60-luciferase engrafted SCID mice.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.