Abstract
Abstract 845
Waldenstrom's macroglobulinemia (WM) is a relatively uncommon plasma cell disorder and most of previous literature is limited to small patient series. We have noted ethnic disparities in multiple myeloma, another plasma cell disorder. We undertook a large Surveillance Epidemiology and End Results (SEER) based analysis to describe outcome disparities in different subgroups of WM patients, with a focus on various ethnicities, so that therapeutic resources can be targeted more effectively.
The SEER 17 Registry data (1973–2008) was utilized for patients with confirmed diagnosis of WM. To avoid bias of under representation of different ethnicities, analysis was restricted to patients with a diagnosis date of 1992 or later. Cases that received a diagnosis at death certificate or autopsy, no follow-up records, as well as lacking documentation on age at diagnosis, sex, or race/ethnicity were excluded. Cox proportional hazards models, adjusted for gender, age, race, year of diagnosis, marital status and stratified by SEER registries were used to evaluate associatio n between patient characteristics and survival. All statistical tests were two-sided and utilized the SAS software (v9.2) with a significance level of 0.05.
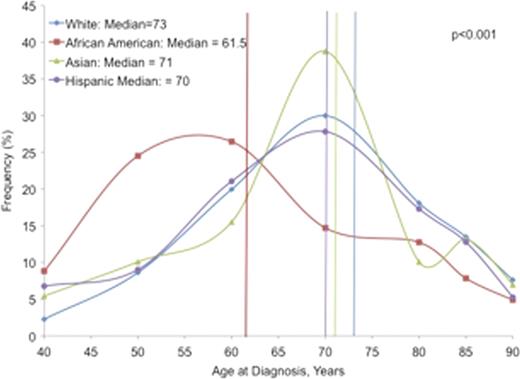
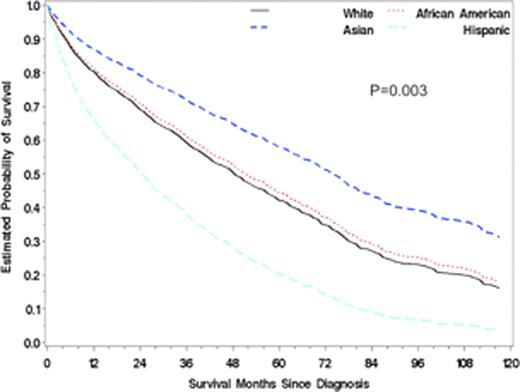
The final analysis included 2,840 WM patients (1,759 males; 62%, 1,081 females; 38%). The studied age-group cohorts included: 18–64 yrs (845; 30%), 65–74 yrs (795; 28%) and >75 yrs (1,200; 42%). Patients were stratified by race/ethnicity: White (2,471; 87%), African-American (AA) (102; 4%), Hispanic (133; 5%), Asian (129; 5%), and Native American (5; 0.1%). Patients were also stratified based on year of diagnosis (before or after 2002) to study the impact of certain novel agents (proteasome inhibitors, IMiDs) on WM treatment. There was a significant difference in the age at diagnosis of WM patients across different ethnicities, with AA the youngest (median 61.5 years) and Whites the oldest (median 73 years) subgroup (p<0.001). (Figure 1) Cause-specific mortality could not be evaluated due to variable documentation of reported causes of death for WM patients in the database. Survival analysis revealed that for all patients, females had better median overall survival (OS) than males (7.3 years vs. 6.2 years, HR 0.834; 95% CI 0.740, 0.939; p=0.003). Among the different age cohorts, patients with age ≥75 years had a significantly worse median OS (4.1 years) than those 65–74 year-old (7.3 years) or 18–64 year-old (10+ years) (p<0.001). Patients diagnosed after 2002 had a significantly better median OS (7.3 years) as compared to patients diagnosed previously (6.1 years) (p=0.002). Hispanics had the worst median OS (5 years) and Whites had the best median OS (6.8 years) across various ethnicities. In a multivariate model using gender, age, marital status, year of diagnosis and race, a significant interaction was noted between race, age and survival, with Hispanics having a significantly worse OS than Whites (HR 1.86; 95% CI 1.269, 2.726; p=0.003) (Figure 2).
Median age at the time of diagnosis in WM patients of different ethnicities.
Studies of outcome disparities are important for evaluating disease characteristics and management needs of specific patient populations as well as optimal triaging of healthcare resources. We have performed the largest population-based analysis for WM including various ethnicities in the novel therapeutic agent era. We observed that AA patients had a significantly younger age at WM diagnosis. Older patients had worse OS across all ethnic subgroups and patients diagnosed after 2002 had a better OS suggesting an impact of novel therapeutic agents (e.g., proteasome inhibitors, IMiDs). Hispanic WM patients had the worst OS among all ethnicities. This survival difference was more significant and pronounced in patients >75 years. This suggests that the impact of race on survival is influenced by patient's age. These results will help in better understanding of various influences on disease biology and clinical behavior.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.