In this issue of Blood, Chu et al report that mice with conditional inactivation of the NF-kappaB (NFkB) negative regulator A20 in B cells have an altered marginal zone B-cell development at young age that culminates in an autoimmune syndrome in older mice.1
The NFkB pathway is an important mediator of immunity and inflammation, with short-lived responses characteristic of the canonical pathway, controlled by inhibitor of nuclear factor kappa-B kinase alpha (IKKa) activation, and long-lived responses characteristic of the alternative pathway controlled by nuclear factor kappa-B inducing kinase (NIK) activation.2 Abnormal regulation of the NFkB pathway has long been implicated in cancer, but it is only recently, through a comprehensive pathway analysis in lymphoma and multiple myeloma, that the genetic basis for its constitutive activation in lymphoid malignancies has been fully unveiled.3-5
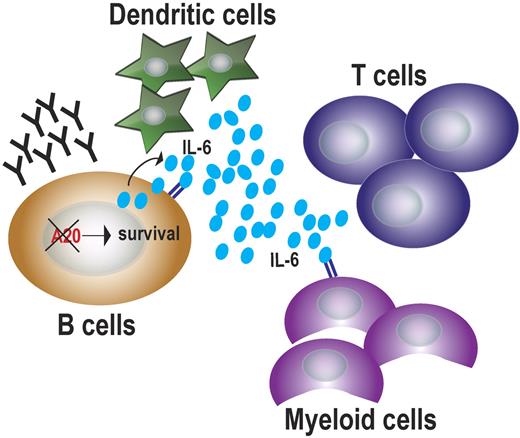
As a wide array of mutations of multiple regulators of both the canonical and noncanonical NFkB pathways have been identified, animal models become critical to elucidate the specific role of each of the identified mutations in the malignant transformation process. Specifically, loss-of-function mutations in the A20 gene have been found in diffuse large B-cell lymphoma, Hodgkin lymphoma, primary mediastinal B-cell lymphoma, and marginal zone lymphoma.6 B lymphocytes may benefit in multiple ways from the loss of A20. There is direct up-regulation of NFkB in the cell, which ultimately provides a strong prosurvival signal.7 On the other hand, the up-regulation of NFkB leads to the release of proinflammatory cytokines, mostly interleukin-6 (IL-6), that creates a supportive environment for immune cells1,8 (see figure).
A20 loss in B cells promotes cell survival and the establishment of an inflammatory microenvironment. Constitutive NFkB signaling in B cells lacking A20 induces expression of prosurvival genes, such as BclXL, and up-regulation of proinflammatory cytokines, such as IL-6, which, in turn, stimulate the growth of immune cells. In the presence of such inflammatory conditions, chronically stimulated autoreactive B cells and plasma cells produce auto-antibodies causing autoimmune disease.
A20 loss in B cells promotes cell survival and the establishment of an inflammatory microenvironment. Constitutive NFkB signaling in B cells lacking A20 induces expression of prosurvival genes, such as BclXL, and up-regulation of proinflammatory cytokines, such as IL-6, which, in turn, stimulate the growth of immune cells. In the presence of such inflammatory conditions, chronically stimulated autoreactive B cells and plasma cells produce auto-antibodies causing autoimmune disease.
Which of these events is the most important? The studies reported in this issue of Blood suggest that it is the latter, although there are some limitations extending this observation to B-cell malignancies in which A20 function is lost. In the mouse model described here, the loss of A20 early in B-cell development, mediated by CD19-CRE, leads to a skewing of normal B-cell differentiation, with abnormalities in marginal zone B cells. It is possible that loss at a later stage of B-cell development would result in a somewhat different phenotype. Interestingly, mouse models that seek to reproduce the constitutive activation of NFkB in B cells do not develop overt malignancies, but rather are characterized by a polyclonal B-cell activation, and heightened immune responses.7,9,10
Is this because the timing of sporadic cellular activation of NFkB or because activation of NFkB is insufficient to cause malignant transformation? Because in B-cell malignancies we are often able to precisely time the sequence of oncogenic events, we are fairly certain that the activation of NFkB is a secondary genetic event that provides a selective advantage, but, based on this the mouse model, it is not itself a transforming event. It would be instructive to see the result of genetic crossings of mice overexpressing oncogenes dysregulated by primary genetic events in lymphoma and multiple myeloma (eg, BCL6, MYC, or Cyclin D1) in the context of constitutive activation of NFkB to fully model the contribution of NFkB to lymphoid malignancies.
Conflict-of-interest disclosure: The author declares no competing financial interests. ■