Abstract
HIV entry into CD4+ cells requires interaction with a cellular receptor, generally either CCR5 or CXCR4. We have previously reported the case of an HIV-infected patient in whom viral replication remained absent despite discontinuation of antiretroviral therapy after transplantation with CCR5Δ32/Δ32 stem cells. However, it was expected that the long-lived viral reservoir would lead to HIV rebound and disease progression during the process of immune reconstitution. In the present study, we demonstrate successful reconstitution of CD4+ T cells at the systemic level as well as in the gut mucosal immune system after CCR5Δ32/Δ32 stem cell transplantation, while the patient remains without any sign of HIV infection. This was observed although recovered CD4+ T cells contain a high proportion of activated memory CD4+ T cells, ie, the preferential targets of HIV, and are susceptible to productive infection with CXCR4-tropic HIV. Furthermore, during the process of immune reconstitution, we found evidence for the replacement of long-lived host tissue cells with donor-derived cells, indicating that the size of the viral reservoir has been reduced over time. In conclusion, our results strongly suggest that cure of HIV has been achieved in this patient.
Introduction
Destruction of the immune system by the HIV is driven by the loss of CD4+ T cells in the peripheral blood and lymphoid tissues. Viral entry into CD4+ cells is mediated by the interaction with a cellular chemokine receptor, the most common of which are CCR5 and CXCR4.1 Because subsequent viral replication requires cellular gene expression processes, activated CD4+ cells are the primary targets of productive HIV infection. Consequently, HIV infection leads predominantly to the depletion of activated memory CD4+ T cells, most of which reside in the gastrointestinal (GI) mucosa.2-4 Although therapeutic control of HIV replication allows the immune system to partially restore and delays disease progression, the cure of HIV infection remains still unachievable with use of the currently available antiretroviral drugs. The major barrier to viral eradication in patients receiving antiretroviral therapy (ART) is the establishment of HIV reservoirs, including low-level productively and latently infected cells.5-7 Thus, maintenance of replication-competent HIV in long-lived cells and distinct anatomical sanctuaries allows the virus to reseed the body once ART is discontinued.8
Cells of persons homozygous for the CCR5 gene variant Δ32 (CCR5Δ32/Δ32) are naturally resistant to infection with CCR5-tropic HIV strains (R5 HIV) because of the lack of CCR5 cell-surface expression.9 Previously, we demonstrated the feasibility of hematopoietic stem cell transplantation (SCT) with CCR5Δ32/Δ32 donor cells (CCR5Δ32/Δ32 SCT) in an HIV-infected patient with relapsed acute myeloid leukemia (AML) and documented absent viremia during the first 20 months of remission, during which time the patient did not receive ART.10,11 This case clearly emphasizes the importance for continuing research in the field of CCR5-targeted treatment strategies, but uncertainty has remained over whether a cure for HIV infection has been achieved in this patient.
In the setting of HIV infection, the effects of pretransplantation conditioning do not allow the complete elimination of HIV, as demonstrated by previous studies in which researchers demonstrated that HIV-infected patients who undergo stem cell transplantation generally experience a viral rebound when ART is discontinued.12-17 For this reason, together with the fact that CXCR4-tropic HIV variants (X4 HIV) were present within the patient's pretransplantation HIV population, it was reasonable to hypothesize that HIV from the viral reservoir may reseed the body once the immune system has efficiently been restored with X4 HIV-susceptible target cells.18,19
Accordingly, key questions that remain to be answered are (1) whether CD4+ T cells have been efficiently restored throughout the body; (2) whether or not the patient's immune system includes HIV-susceptible target cells; and (3) how stable the size of the HIV reservoir is during the process of immune reconstitution after CCR5Δ32/Δ32 SCT.
Here, to address these questions, we extend our previous study to improve our knowledge about the curative potential of CCR5Δ32/Δ32 SCT for HIV infection. We evaluated the reconstitution of CD4+ T cells at the systemic level as well as in the mucosal immune system during the posttransplantation period of more than 3.5 years. To verify the ability of the recovered CD4+ T cells to act as HIV target cells, their activation status, CXCR4 expression profile, and susceptibility to productive HIV infection was analyzed. Moreover, because the absence of the CCR5 wild-type gene variant in donor cells provided us with the possibility to discriminate between donor- and host-derived immune cells, we were able to examine the persistence of potential viral reservoirs, in addition to the detection of viral sequences, in distinct tissue compartments.
Methods
Subjects
In February 2007, an HIV-infected patient underwent SCT because of a relapse of AML with a graft consisting of CCR5Δ32/Δ32 donor cells. The pretransplantation conditioning regimen included 100 mg/m2 amsacrine, 30 mg/m2 fludarabine, 2 g/m2 cytarabine (day −12 until −9); 60 mg/kg cyclophosphamide (days −4 and −3); 5.5 mg/kg rabbit antithymocyte globuline (in 3 doses between day −3 and −1); and a 400-cGy total body irradiation (TBI; day −5). ART was discontinued on the day of transplantation, and 13 months later the patient received a second transplantation with CCR5Δ32/Δ32 stem cells from the same donor because of a second relapse of AML. The conditioning regimen consisted of 100 mg/m2 cytarabine (day −7 until day −1), 6 mg/m2 gemtuzumab (day −7 and day −1), and a 200-cGy TBI (day −1). For clinical data and further details, see Hütter et al.10 At 5.5, 24, and 29 months after the first CCR5Δ32/Δ32 SCT, the patient underwent colonoscopy, and biopsy specimens were taken as the result of suspected intestinal graft-versus-host disease (GVHD) while tapering immunosuppressive treatment. With the patient's informed consent for this procedure, 10-13 additional colon biopsy specimens were collected at each time point for research purpose of the present study. Examination of histologic colon sections excluded the diagnosis of intestinal GVHD. Twelve months after transplantation, the patient underwent a liver biopsy, and histologic examination confirmed GVHD grade 1, which was controlled with adaption of immunosuppressive therapy (ie, cyclosporine A, methylprednisolone, mycophenolate mofetil). At 17 months after transplantation, the patient presented with neurologic disorders. Magnetic resonance imaging of the brain identified signal abnormalities compatible with leukoencephalopathy. For further evaluation, cerebrospinal fluid (CSF) samples were collected repeatedly, and, in addition, a brain biopsy was performed. Polymerase chain reaction (PCR) detection of JC virus was negative in all samples. Histologic evaluation revealed astrogliosis with microglial activation. The cumulative effect of initial AML treatment chemotherapy and salvage chemotherapy after relapse of AML, as well as pretransplantation conditioning regimen, including TBI, were assumed as the cause of leukoencephalopathy,20 which turned out to be self-limiting. Immunosuppressive treatment has been stopped 38 months after CCR5Δ32/Δ32 SCT without recurrence of GVHD.
In addition, 10 HIV-uninfected SCT patients were included into this study (SCT controls). Four of these patients underwent colonoscopy, and intestinal GVHD was histologically excluded in all cases. A total of 15 HIV-uninfected patients served as healthy controls; 5 of them underwent colonoscopy for cancer preventive examination. The study was approved by the Charité-University Medicine Berlin institutional review board, and all participants provided informed consent to study participation in accordance with the Declaration of Helsinki.
Cell preparation and activation
Peripheral blood mononuclear cells (PBMCs) were isolated from heparinized venous blood by standard Ficoll gradient centrifugation, and mucosal mononuclear cells (MMCs) were isolated from colon biopsy specimens by collagenease type II (Sigma-Aldrich) digestion.21 Cells were either immediately used for subsequent analysis or cryoconserved until HIV susceptibility assays. For some experiments, PBMCs were activated for 2 days with 3 μg/mL of phythemagglutinin (PHA; Sigma-Aldrich) and 50 U/mL of recombinant interleukin-2 (IL-2; R&D Systems) in RPMI 1640 + GlutaMAX cell culture medium (Invitrogen) containing 10% heat-inactivated fetal calf serum (Sigma-Aldrich), 100 U/mL of penicillin, and 100 μg/mL streptomycin (both from Biochrom) before flow cytometric analysis.
Flow cytometric analysis and cell sorting
Flow cytometric analysis was performed by the use of antibodies against CD3 (clone UCHT1; BD Biosciences), CD4 (SK3; BD), CD31 (WM59; BD), CD38 (HIT2; BD), CD45RO (UCHL1; BD), CD49d (9F10; BD), CD62L (Dreg-56; BD), CXCR4 (12G5; BD), HLA-DR (Immu357; Beckman Coulter), and Ki67 (Ki67; DAKO). Absolute numbers of CD4+ T cells were determined in fresh whole blood by the use of TruCount tubes and CD3/CD4/CD8 TriTest (BD) according to the manufacturer's protocol. Data were acquired on the FACSCalibur flow cytometer (BD) and analyzed with CellQuest software (BD). Lymphocytes were gated on the basis of characteristic forward and sideward scatter properties. Central memory CD4+ T cells were classified by coexpression of CD45RO and CD62L, and effector memory CD4+ T cells were classified by lack of CD62L. Recent thymic emigrants were identified by coexpression of CD31 and CD62L on CD45RO− CD4+ T cells and central naive CD4+ T cells by lack of CD31.22 CXCR4 expression density on CD4+ T cells was evaluated as the mean fluorescence intensity (MFI) of CXCR4 expression divided by the MFI value obtained with the corresponding isotype control (BD) and is expressed as the MFI ratio.
For mucosal cell sorting, the following additional antibodies were used: anti-CD33 (AC104.3E3; Miltenyi Biotec) and anti-CD68 (Kim7; BD). Cell-sorting procedures were performed by customer service of the Flow Cytometry Core Facility at the Berlin-Brandenburg Center for Regenerative Therapies, Germany, with the use of the FACSAriaII flow cytometer (BD) and FACSDiva software (BD). Mucosal CD4+ T cells were identified by their coexpression of CD3 and CD4 in the lymphocyte gate, and mucosal macrophages were selected by their coexpression of CD33 and CD68 in the CD3− macrophage gate.23 Antibodies were conjugated to fluorescin, phycoerythrin, peridinin chlorophyll protein, or allophycocyanin.
HIV-susceptibility assay
CCR5-tropic HIV-1 strain JR-CSF (obtained from the EVA Center for AIDS Reagents, National Institute for Biological Standards and Control [NIBSC]) was propagated in PBMC. A stock of CXCR4-tropic HIV-1 strain NL4-3 was generated from the HIV-1 molecular clone pNL4-3 (obtained from the EVA Center for AIDS Reagents) and then propagated in PBMC. Virus-containing cell culture supernatants were passed through a 22-μm pore-size filter (BD) to remove cell debris and then treated with Dnase (Boehringer Mannheim) in the presence of 1mM MgCl2 for 30 minutes at 37°C to remove contaminating DNA. Virus stocks were stored at −80°C. The infectious titer of thawed viral stocks was determined by tissue culture infectious dose 50% assays in PBMC. Before infection, PBMCs or MMCs were activated with PHA and IL-2 for 48 hours. Cells were washed and cultivated with virus at a multiplicity of infection of 0.001 in RPMI1640 medium supplemented with 20 U/mL of IL-2. Viral stocks diluted in cell-free medium served as background control, the patient's cells alone as a mock control, and cell-free virus suspensions as a control for background corrections. Supernatants were removed from cell cultures and cell-free controls as indicated and were replaced by fresh medium and stored at −80°C until analysis for viral replication by quantitative measurement of the HIV-1 core protein p24 production with the HIV-1 p24 ELISA assay (XpressBiotech) according to the manufacturer's protocol.
Immunohistochemistry and immunofluorescence staining
Immunostaining on paraffin sections was performed as described previously.24 Primary antibodies were mouse anti-CD4 (1F6; Novocastra), mouse anti-CD68 (PGM1; DAKO), or goat anti-CCR5 (CKR-5 [C20]; Santa Cruz Biotechnology). For detection of CD4 labeling, the Streptavidine Alkaline Phosphatase-kit (DAKO) was used. Positive cells within the mucosa of colon tissue were quantified per high-power field (hpf, 0.237 mm2), and 10 hpf were averaged in each case. Per sampling at least 3 sections were analyzed. Immunohistochemical evaluations were performed in a blinded manner, ie, the researcher was unaware of the patient's clinical characteristics. For CD4/CCR5 or CD68/CCR5 double immunofluorescence labeling, Alexa-Fluor 488–conjugated antimouse was used in combination with Alexa-Fluor 555–conjugated antigoat (Invitrogen). Images were acquired by the use of a fluorescence microscope (AxioImager Z1) equipped with a charged-coupled-device camera (AxioCam MRm) and processed with Axiovision software (Carl Zeiss MicroImaging). Negative controls were performed by omitting the primary antibodies, and unspecific staining of the antibodies was excluded by use of isotype control antibodies.
CCR5 genotyping
To study the CCR5 gene variant in HIV target cells, genomic DNA was extracted from sorted mucosal CD4+ T cells or macrophages with the use of the NucleoSpin TissueXS (Macherey & Nagel) according to the manufacturer's protocol. DNA was then subjected to PCR amplification with primers for the CCR5 gene spanning the Δ32-region from nucleotide 826 to 1138 on the chromosome 3p21.31 (accession no: NM_000579). The expected fragments were 312 bp for the CCR5 wild-type and 280 bp for the CCR5Δ32 variant.
Detection of HIV and HIV-specific antibodies
Viral RNA was isolated from plasma or CSF and the long terminal repeat and gag regions were amplified and detected with the use of the COBAS AmpliPrep/COBAS TaqMan HIV-1 Test v1.0 (Roche). Total DNA was isolated from PBMCs, tissue biopsy specimens, and sorted cells with the use of the QIAamp DNA Blood Mini Kit, the Allprep DNA/RNA Mini Kit (both from QIAGEN), and the NucleoSpin Tissue XS, respectively, following the manufacturer's directions and the long terminal repeat and env regions were detected as described previously.10 Antibodies directed against HIV antigens in serum samples were detected with immunoblot (Abbott) as described previously.10
Statistical analysis
Data are represented as medians and were analyzed with the use of 2-tailed Student t test with Prism software Version 4.0 (Graph Pad Inc). Significance is denoted with asterisks (ie, *P < .05, **P < .01, ***P < .001).
Results
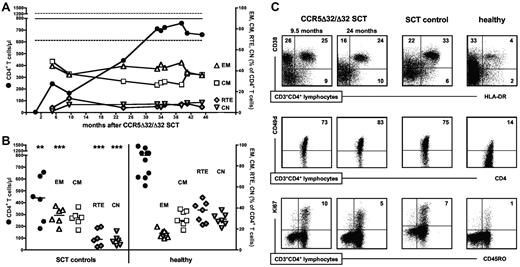
Efficient recovery of CD4+ T cells was associated with a characteristic enrichment of activated/effector memory CD4+ T cells
After CCR5Δ32/Δ32 SCT, chimerism analysis as well as genotyping of CCR5 alleles suggested that host T cells were completely eliminated from the periphery.10 Numbers of donor-derived peripheral CD4+ T cells increased continuously and, after 2 years, reached levels within the normal range of age-matched healthy patients (Figure 1A). Further phenotypic analysis revealed an increase of memory CD4+ T-cell numbers, with a parallel, but low, increase of CD4+ recent thymic emigrant as well as central naive CD4+ T-cell numbers. In both the CCR5Δ32/Δ32 SCT patient and the SCT control patients, the proportion of central memory CD4+ T cells was within the normal range, whereas effector memory CD4+ T cells remained markedly enriched within the CD4+ T-cell compartment compared with healthy control values (Figure 1A-B). This cellular composition indicates a proliferative expansion of mature CD4+ T cells. In accordance, the frequency of cells expressing the activation markers CD38, CD49d, and HLA-DR and the proliferation marker Ki67 was greater within CD4+ T cells from CCR5Δ32/Δ32 SCT and control SCT patients than from healthy control patients (Figure 1C). Thus in both cases, CD4+ T cells recovered primarily through homeostatic proliferation of memory CD4+ T cells, confirming previous reports of posttransplantation immune reconstitution.25,26 These results demonstrate that the CCR5Δ32/Δ32 SCT patient experienced a regular reconstitution of the peripheral CD4+ T-cell compartment after CCR5Δ32/Δ32 SCT, including the characteristic enrichment of activated/effector memory CD4+ T cells.
Peripheral CD4+ T cells have been efficiently restored and contain an increased proportion of activated/effector memory CD4+ T cells compared with healthy control patients. CD4+ T-cell numbers and frequencies of effector memory cells (EM), central memory cells (CM), recent thymic emigrants (RTE), and central naive cells (CN) within CD4+ T cells (A) during the course of immune reconstitution after CCR5Δ32/Δ32 SCT and (B) in SCT controls (27.5 ± 7 months after transplantation) compared with healthy patients were determined in fresh whole blood. Median CD4+ T-cell numbers of healthy patients is indicated by the thick horizontal line, and the dashed horizontal lines denote the normal 25th and 75th percentiles in panel A. The horizontal lines in panel B denote the median values of each group. Statistical significances are given for comparisons between healthy control values and SCT control values (*P < .05, **P < .01, ***P < .001). (C) CD4+ T-cell expression of the activation markers CD38, HLA-DR, and CD49d and the proliferation marker Ki67 at 9.5 and 24 months after CCR5Δ32/Δ32 SCT in comparison with SCT control and healthy control patients. Data are representative for 5 SCT control and 4 healthy control patients.
Peripheral CD4+ T cells have been efficiently restored and contain an increased proportion of activated/effector memory CD4+ T cells compared with healthy control patients. CD4+ T-cell numbers and frequencies of effector memory cells (EM), central memory cells (CM), recent thymic emigrants (RTE), and central naive cells (CN) within CD4+ T cells (A) during the course of immune reconstitution after CCR5Δ32/Δ32 SCT and (B) in SCT controls (27.5 ± 7 months after transplantation) compared with healthy patients were determined in fresh whole blood. Median CD4+ T-cell numbers of healthy patients is indicated by the thick horizontal line, and the dashed horizontal lines denote the normal 25th and 75th percentiles in panel A. The horizontal lines in panel B denote the median values of each group. Statistical significances are given for comparisons between healthy control values and SCT control values (*P < .05, **P < .01, ***P < .001). (C) CD4+ T-cell expression of the activation markers CD38, HLA-DR, and CD49d and the proliferation marker Ki67 at 9.5 and 24 months after CCR5Δ32/Δ32 SCT in comparison with SCT control and healthy control patients. Data are representative for 5 SCT control and 4 healthy control patients.
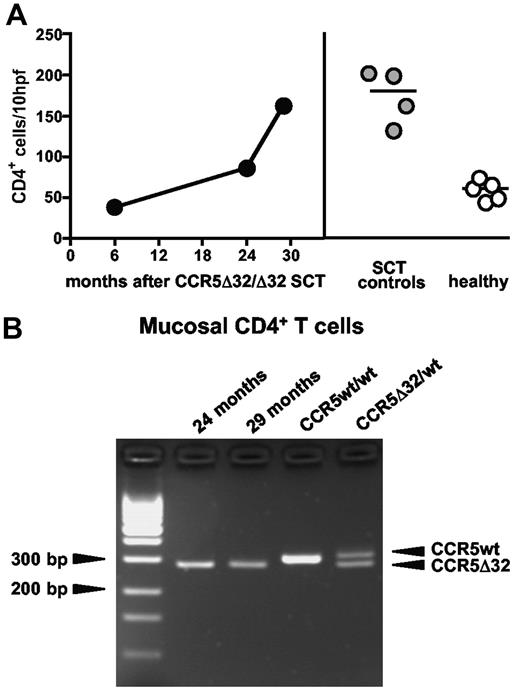
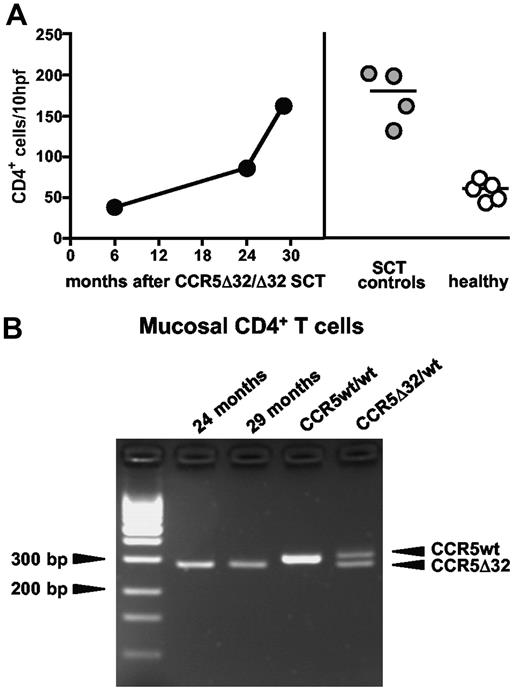
Donor-derived CD4+ T cells have efficiently repopulated the gut mucosal immune system
Most of the body's CD4+ T cells reside in the GI tract. To assess the recovery of CD4+ T cells in the gut mucosal immune system, CD4+ T cells were immunohistochemically quantified in colon tissue sections at 3 time points after CCR5Δ32/Δ32 SCT and were compared with SCT control and healthy control patients. The number of mucosal CD4+ T cells increased during the posttransplantation period, and at 29 months after CCR5Δ32/Δ32 SCT, the density of CD4+ T cells in the GI mucosa was similar to that of the SCT control patients (162 vs 180 ± 33 cells/hpf; Figure 2A). Thus, no lack of immune reconstitution could be noted in the mucosal immune system. Interestingly, compared with healthy control patients there was a more than 2-fold increased frequency of mucosal CD4+ T cells in all SCT patients (60 ± 12 vs 162 ± 29 cells/hpf), demonstrating that treatment with conditioning followed by SCT triggers the enrichment of HIV target cells in the gut mucosal immune system (Figure 2A).
The mucosal immune system has been efficiently repopulated with donor-derived CD4+ T cells. (A) Immunohistochemical quantification of CD4+ T cells in colon tissue of the CCR5Δ32/Δ32 SCT patient, SCT control patients (27 ± 9 months after transplantation), and healthy control patients. The horizontal lines denote the median values of each group. (B) Genomic DNA was extracted from mucosal CD4+ T cells and subjected to CCR5-specific PCR spanning the Δ32 region.
The mucosal immune system has been efficiently repopulated with donor-derived CD4+ T cells. (A) Immunohistochemical quantification of CD4+ T cells in colon tissue of the CCR5Δ32/Δ32 SCT patient, SCT control patients (27 ± 9 months after transplantation), and healthy control patients. The horizontal lines denote the median values of each group. (B) Genomic DNA was extracted from mucosal CD4+ T cells and subjected to CCR5-specific PCR spanning the Δ32 region.
To confirm the donor-origin of mucosal CD4+ T cells, we performed additional phenotypic and genotypic analysis. In situ detection of CCR5 by immunofluorescence staining at 5.5 and 24 months after CCR5Δ32/Δ32 SCT revealed no CCR5 expression on mucosal CD4+ T cells (not shown), which corroborates our previous finding from flow cytometric analysis.10 Moreover, CD4+ T cells sorted from MMC at 24 and 29 months after CCR5Δ32/Δ32 SCT were negative for the CCR5 wild-type gene (Figure 2B). This demonstrates that increased numbers of mucosal CD4+ T cells were exclusively derived from donor hematopoietic cells. Taken together, these results reveal that circulating donor-derived CD4+ T cells were efficiently recruited to the GI tract and have repopulated the mucosal CD4+ T-cell compartment after CCR5Δ32/Δ32 SCT.
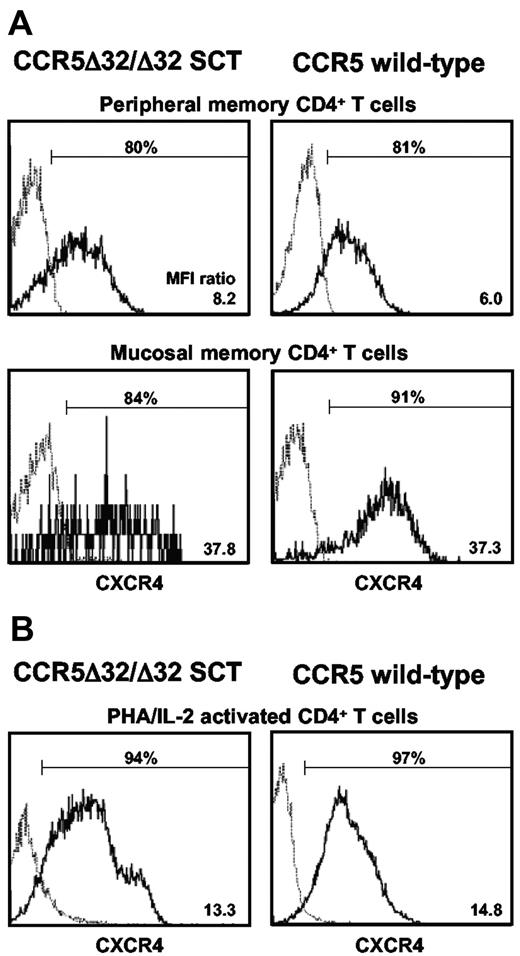
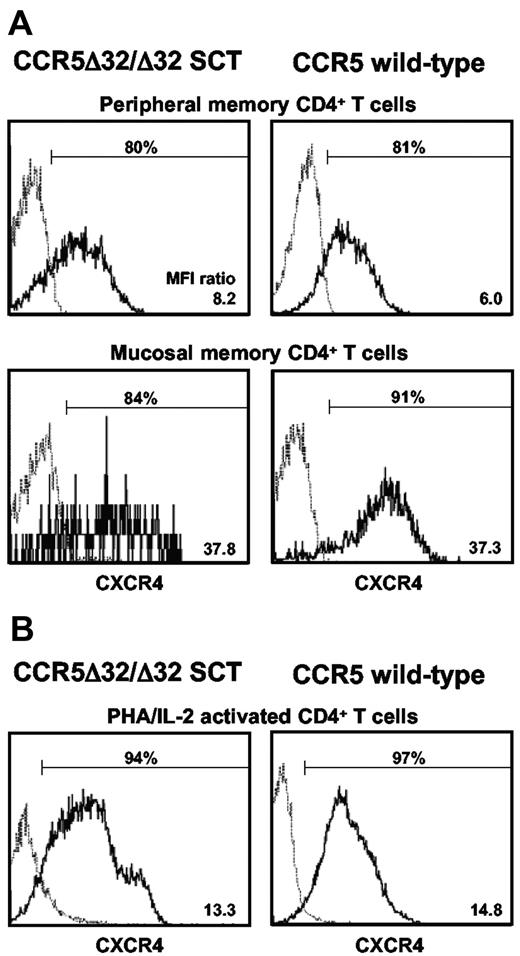
CXCR4 surface availability is not impaired on recovered CD4+ T cells
Reconstitution of the CD4+ T-cell compartment after CCR5Δ32/Δ32 SCT was associated with an expansion of activated memory cells (Figures 1 and 2), the preferential targets of productive HIV infection. Donor-derived CD4+ T cells are naturally resistant to CCR5-tropic HIV infection because of the lack of CCR5 surface expression. We were interested in whether recovered CCR5Δ32/Δ32 CD4+ T cells might also exhibit reduced CXCR4 surface availability. Therefore, we analyzed fresh whole blood cells and MMC for CXCR4 surface expression on CD4+ T cells in comparison with cells obtained from CCR5 wild-type patients. As shown in Figure 3A, both the frequency of CXCR4-expressing cells within memory CD4+ T cells as well as CXCR4 surface expression density at the single cell level (expressed as the MFI ration) were comparable with those of CCR5 wild-type control patients (80.8% ± 2.0% and 6.6% ± 1.0%, respectively). This was also observed for the peripheral naive CD4+ T-cell compartment (not shown).
CXCR4 surface expression on peripheral and mucosal CD4+ T cells is not impaired in the CCR5Δ32/Δ32 SCT patient. CD4+ T cells in (A) fresh whole blood, MMC (5.5 months after transplantation), or (B) ex vivo PHA/IL-2–activated PBMCs were analyzed for the frequency of CXCR4 surface-expressing cells and the CXCR4 expression density. CXCR4 expression density on CD4+ T cells was evaluated as the MFI of CXCR4 expression divided by the MFI value obtained with the corresponding isotype control and is expressed as the MFI ratio.
CXCR4 surface expression on peripheral and mucosal CD4+ T cells is not impaired in the CCR5Δ32/Δ32 SCT patient. CD4+ T cells in (A) fresh whole blood, MMC (5.5 months after transplantation), or (B) ex vivo PHA/IL-2–activated PBMCs were analyzed for the frequency of CXCR4 surface-expressing cells and the CXCR4 expression density. CXCR4 expression density on CD4+ T cells was evaluated as the MFI of CXCR4 expression divided by the MFI value obtained with the corresponding isotype control and is expressed as the MFI ratio.
Because the level of CXCR4 expression may vary with cell activation, we next analyzed CXCR4 expression on CD4+ T cells upon ex vivo activation and found efficient expression of CXCR4 on CCR5Δ32/Δ32 CD4+ T cells (Figure 3B). These data demonstrate that the CCR5Δ32/Δ32 SCT was not associated with an impaired CXCR4 expression on recovered CD4+ T cells. In vivo, the availability of CXCR4 may be affected by the chemokine CXCL12, the physiologic ligand of CXCR4.27 During the immune reconstitution period, CXCL12 plasma levels in the CCR5Δ32/Δ32 SCT patient remained within the normal range of healthy patients (not shown), indicating that the in vivo availability of CXCR4 was not impaired by naturally occurring receptor occupation. Altogether, these results indicate that recovered CD4+ T cells are not protected against X4 HIV entry.
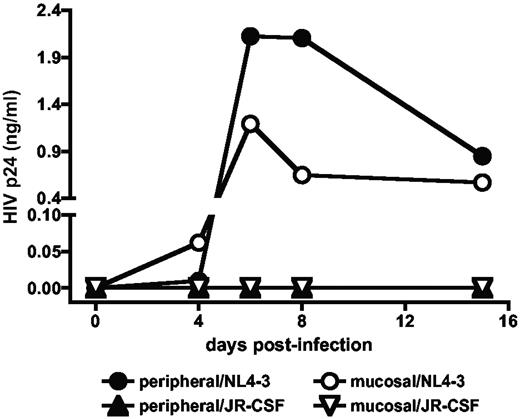
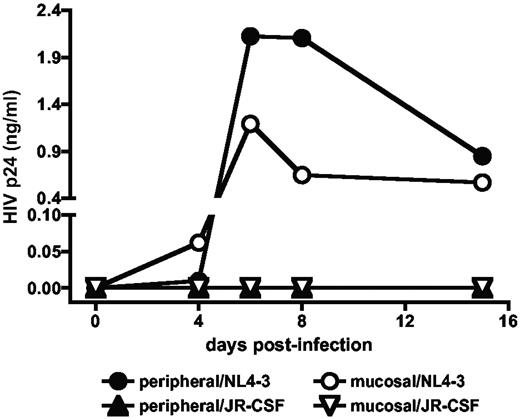
Recovered CD4+ T cells are susceptible to productive X4 HIV infection
Susceptibility of recovered CD4+ T cells in the central as well as the mucosal immune system to productive HIV infection was studied by ex vivo infections of PBMC and MMC obtained after CCR5Δ32/Δ32 SCT. As shown in Figure 4, cells from both compartments were susceptible to productive infection by X4 HIV. Consistent with our previous observation, virus production of the PBMC-propagated X4 HIV strain was greater in peripheral than in mucosal CD4+ T cells.28 As expected, because of the lack of CCR5 surface expression on donor-derived cells, both peripheral and mucosal CD4+ T cells were resistant to R5 HIV infection.
Recovered peripheral and mucosal CD4+ T cells are susceptible to productive X4 HIV infection. PBMC and MMC obtained 24 months after CCR5Δ32/Δ32 SCT were activated with PHA and IL-2 and then incubated with the CCR5-tropic HIV-1 strain JR-CSF or the CXCR4-tropic HIV-1 strain NL4-3 at a multiplicity of infection of 0.001. Viral replication was quantified by measuring the amount of HIV core protein p24 in the cell-free supernatants of cultures. No virus production was observed in the mock controls. Similar results were obtained with peripheral lymphocytes purified at 9.5 and 34.5 and months after CCR5Δ32/Δ32 SCT.
Recovered peripheral and mucosal CD4+ T cells are susceptible to productive X4 HIV infection. PBMC and MMC obtained 24 months after CCR5Δ32/Δ32 SCT were activated with PHA and IL-2 and then incubated with the CCR5-tropic HIV-1 strain JR-CSF or the CXCR4-tropic HIV-1 strain NL4-3 at a multiplicity of infection of 0.001. Viral replication was quantified by measuring the amount of HIV core protein p24 in the cell-free supernatants of cultures. No virus production was observed in the mock controls. Similar results were obtained with peripheral lymphocytes purified at 9.5 and 34.5 and months after CCR5Δ32/Δ32 SCT.
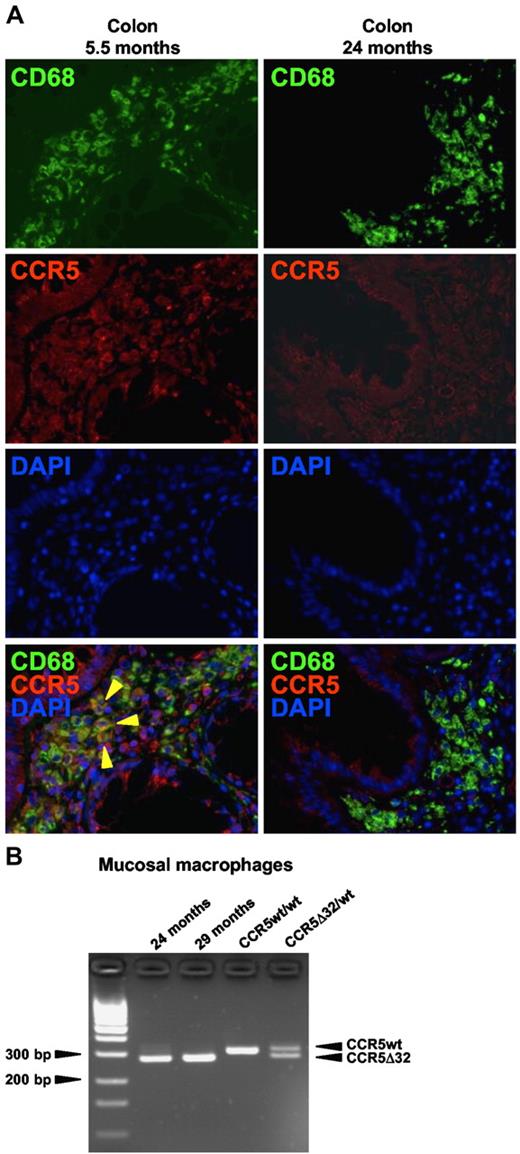
Long-lived HIV target cells of host origin were replaced with donor-derived cells during the posttransplantation period
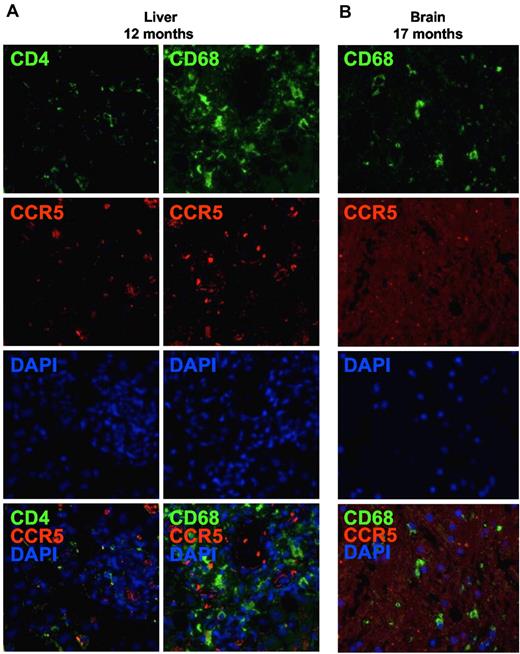
Because of the fact that recovered CD4+ T cells are susceptible to productive X4 HIV infection, long-lived HIV-infected host cells that survive chemo- and irradiation therapies represent potential sources from which HIV to emerge. Noncirculating immune cells such as tissue CD4+ T cells or macrophages are virtually chemo/radio-resistant and, therefore, represent possible viral reservoirs. We investigated the presence of residual host immune cells after CCR5Δ32/Δ32 SCT by in situ immunofluorescence detection of cellular CCR5 expression. Clinical samples from the liver, the brain, and the colon could be used for research purposes in the present study after a diagnosis was given. Brain tissue specimens were available from the white matter and the cortex. From the colon, 3 separate biopsy specimens were available from each of 3 time points during the course of immune reconstitution. In the liver, 12 months after CCR5Δ32/Δ32 SCT, CCR5-expressing CD4+ T cells or macrophages/Kupffer cells were not detectable (Figure 5A). Likewise, 17 months after CCR5Δ32/Δ32 SCT, no CCR5-expressing macrophages/microglia were found in the brain (Figure 5B).
No evidence for residual HIV target cells of host origin in the liver and the brain. CCR5-expressing CD4+ T cells or macrophages were detected (A) in liver and (B) in brain tissue sections obtained 12 and 17 months after CCR5Δ32/Δ32 SCT, respectively, by in situ immunofluorescence double staining for CD4 (green) or CD68 (green) and CCR5 (red). Original magnification ×400. Images were acquired by use of the AxioImager Z1 fluorescence microscope (Carl Zeiss MicroImaging) coupled to the AxioCam MRm digital camera (Carl Zeiss). Acquisition software: Axiovision (Carl Zeiss). Software used for image processing: Adobe Photoshop CS (Adobe Systems).
No evidence for residual HIV target cells of host origin in the liver and the brain. CCR5-expressing CD4+ T cells or macrophages were detected (A) in liver and (B) in brain tissue sections obtained 12 and 17 months after CCR5Δ32/Δ32 SCT, respectively, by in situ immunofluorescence double staining for CD4 (green) or CD68 (green) and CCR5 (red). Original magnification ×400. Images were acquired by use of the AxioImager Z1 fluorescence microscope (Carl Zeiss MicroImaging) coupled to the AxioCam MRm digital camera (Carl Zeiss). Acquisition software: Axiovision (Carl Zeiss). Software used for image processing: Adobe Photoshop CS (Adobe Systems).
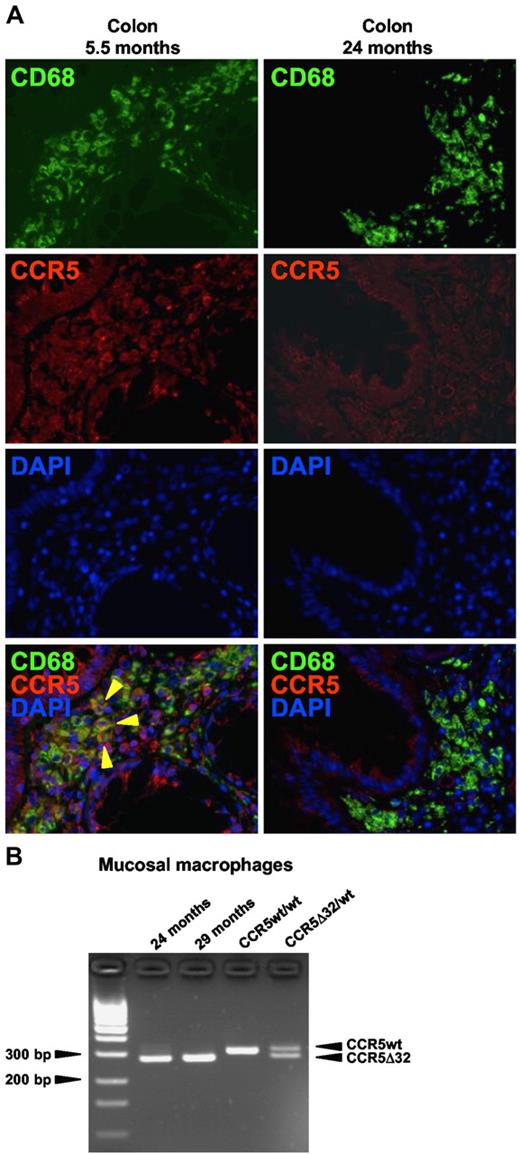
In the colon, there was no evidence of residual host CD4+ T cells after CCR5Δ32/Δ32 SCT, as already described previously (Figure 2B). However, in situ immunofluorescence staining revealed the presence of CCR5-expressing macrophages at 5.5 months after CCR5Δ32/Δ32 SCT, which is in agreement with our previous flow cytometric data10 and demonstrates the persistence of host macrophages during the first months after CCR5Δ32/Δ32 SCT (Figure 6A). Importantly, later in the course of immune reconstitution, CCR5 expression on macrophages became undetectable indicating their replacement with donor-derived cells (Figure 6A). To further prove the origin of mucosal macrophages, we performed additional genotypic analysis of sorted mucosal macrophages. As shown in Figure 6B, 24 and 29 months after CCR5Δ32/Δ32 SCT, mucosal macrophages were negative for the CCR5 wild-type gene. The absence of host's genomic DNA in mucosal macrophages at these time points confirms the phenotypic results and suggests that host macrophages have been replaced with donor-derived cells during the posttransplantation period.
Host macrophages were replaced with donor-derived cells during the course of immune reconstitution. (A) CCR5-expressing macrophages were detected by in situ immunofluorescence double staining for CD68 (green) and CCR5 (red) in colon tissue sections obtained 5.5 or 24 months after CCR5Δ32/Δ32 SCT. CCR5-expressing macrophages are indicated by yellow arrows. (B) At 24 and 29 months after CCR5Δ32/Δ32 SCT, macrophages were sorted from mucosal cells and genotyped by CCR5 variant-specific PCR.
Host macrophages were replaced with donor-derived cells during the course of immune reconstitution. (A) CCR5-expressing macrophages were detected by in situ immunofluorescence double staining for CD68 (green) and CCR5 (red) in colon tissue sections obtained 5.5 or 24 months after CCR5Δ32/Δ32 SCT. CCR5-expressing macrophages are indicated by yellow arrows. (B) At 24 and 29 months after CCR5Δ32/Δ32 SCT, macrophages were sorted from mucosal cells and genotyped by CCR5 variant-specific PCR.
HIV remains undetectable in distinct tissue compartments
The presence of HIV RNA and HIV DNA was examined in distinct tissue compartments during the course of 45 months after CCR5Δ32/Δ32 SCT. Viral sequences were not detectable in all the samples tested (Table 1).
Antibodies against HIV decrease over time
Previously, we reported the loss of antibodies directed against the HIV polymerase as well as a decrease of HIV envelope and core-specific antibodies during the first 20 months after CCR5Δ32/Δ32 SCT.10 Immunoblot analysis revealed a continuing decline of HIV specific antibodies thereafter demonstrating the process of serodeconversion: whereas HIV core-directed antibodies (p17, p24) disappeared completely, the serum level of antibodies against the HIV envelope (gp41, gp120) further decreased. Today, the patient has only HIV envelope-specific antibodies.
Discussion
Immune reconstitution is critical to the long-term success of the SCT, and, in HIV-infected patients, also provides a prerequisite for viral rebound and HIV disease progression. Progressive infection in turn impairs the reconstitution of CD4+ T cells after SCT. Our results show that systemic recovery of CD4+ T cells after CCR5Δ32/Δ32 SCT and discontinuation of ART was not impaired compared with that of SCT control patients. In accordance with previous studies,25,26 repopulation of the CD4+ T-cell compartment was associated with peripheral expansion of donor-derived memory CD4+ T cells, that probably occurs to compensate for the limited thymic capacity in adults.29-31 Generally, this homeostasis-driven expansion of activated memory CD4+ T cells leads to an enrichment of the preferential targets for productive infection with both R5 HIV and X4 HIV32 and likely contributes to the rapid dynamic of HIV rebound after conventional SCT in HIV-infected patients.12,14,15,17 Viral tropism analysis was not in the focus of previous reports of HIV-infected patients with conventional SCT and would be an interesting issue to address in future studies.
In the CCR5Δ32/Δ32 SCT patient, CD4+ T-cell numbers have even returned to the normal range of healthy patients whereas HIV RNA and HIV DNA remain continuously undetectable in plasma and PBMC, respectively. Today, by monitoring the most common prognostic markers, ie plasma viral load and CD4+ T-cell counts in the peripheral blood, HIV disease cannot be assessed in this patient.
However, observations from the central immune compartment need not be representative for distinct tissue compartments throughout the body. Only 1%-2% of the body's total CD4+ T cells reside in the peripheral blood, whereas the majority of immune cells are located in the GI tract.33 Containing most of the body's activated memory CD4+ T cells with high expression of cellular receptors, the mucosal immune system is highly prone to productive infection with both R5 HIV and X4 HIV.3,28,34-36 In fact, profound depletion of CD4+ T cells in the GI mucosa occurs earlier than that in blood or lymph nodes regardless of the infection route, and even with complete suppression of viremia for many years, residual low-level replication in the GI tract prevents full recovery of mucosal CD4+ T cells in ART-treated HIV-infected patients.2,37-39 Poor recovery of CD4+ T cells in the mucosal immune system is therefore an important risk factor for the development of HIV disease progression. After CCR5Δ32/Δ32 SCT, we found that the process of immune reconstitution included a gradual increase of donor-derived CD4+ T cells in the GI mucosa. Compared with HIV-uninfected SCT control patients, mucosal CD4+ T-cell numbers normalized whereas HIV remained undetectable in gut tissue specimens as well as in mucosal HIV target cell populations. These findings argue for the absence of HIV disease progression in the largest component of the lymphoid organ system. Surprisingly, compared with healthy control patients, mucosal CD4+ T-cell numbers in both the CCR5Δ32/Δ32 SCT patient and the SCT control patients were increased. This finding may likely be explained by the high prevalence of activated/effector memory CD4+ T cells in the circulation, for which we have previously found enhanced gut-homing capacity.40 In addition, the normalized frequency of central memory cells within circulating CD4+ T cells suggests that recovered CD4+ T cells have been efficiently directed to peripheral lymph nodes.41,42 Furthermore, the decline of HIV-specific antibodies after CCR5Δ32/Δ32 SCT indicates the continuous absence of HIV gene expression in lymphoid tissues after discontinuation of ART.
In addition to their natural protection from R5 HIV infection, CCR5Δ32/Δ32 CD4+ T cells of some persons have been suggested to be less susceptible to X4 HIV entry as a result of down-regulated CXCR4 expression.43,44 However, in the patient described here, we found no evidence for an abnormal CXCR4 expression on recovered CD4+ T cells. Moreover, the patient's peripheral and mucosal CD4+ T cells are susceptible to productive infection with X4 HIV, demonstrating that the CCR5Δ32/Δ32 SCT has not provided protection against X4 HIV infection. Consequently, the patient's risk of exogenous HIV reinfection is not completely eliminated.
Altogether, our results demonstrate that the process of immune reconstitution has successfully restored both the central and the mucosal immune system with CD4+ T cells that lack CCR5 surface expression but have susceptibility to productive X4 HIV infection. Consequently, host cells that survived the chemoirradiation therapies represent potential sources for X4 HIV rebound. Host-originating CD4+ T cells appear to be completely removed from the patient's immune system; however, in particular tissue macrophages may play a critical role as viral reservoir because they are virtually resistant to conditioning procedures and less prone to the cytopathic effects of HIV infection.45 HIV became undetectable in the brain during a neuropathologic episode, although the associated microglia activation and astrogliosis may support reactivation of viral replication from latently infected cells. This provides indirect evidence for the absence of replication-competent HIV in cells of the brain. Furthermore, in brain as well as in liver tissue sections, no CCR5 expression on macrophages was detectable, indicating the replacement of host microglial cells and Kupffer cells by donor-derived cells. Because CCR5 is not constitutively expressed on tissue macrophages,46 the limited sample availability did not allow us to extend the phenotypic results to cell-specific genomic analysis, and also, because the analyzed sections are representative only for a very limited area of the respective organ, these findings cannot definitely exclude the presence of residual, potentially infected, host cells.
However, there is convincing evidence from studies in mice to suggest that host tissue macrophages were efficiently replaced with donor-derived cells during the course of immune reconstitution. For example, although it is generally accepted that microglia under steady-state conditions are very slowly renewed by cells of hematopoietic origin, it has been demonstrated that the conditioning procedure efficiently enhances this process after stem cell transplantation.47,48 Moreover, the majority of Kupffer cells are replaced already early after SCT49 and, importantly, increasing conversion rates of tissue macrophages over time after transplantation has been demonstrated in distinct tissue compartments throughout the whole body.50,51 Evidence in support of the conclusion that conversion from host to donor tissue macrophages took place in the patient after CCR5Δ32/Δ32 SCT comes from our serial analysis in colon tissue. Here, phenotypic results revealed that residual host cells were present within the mucosal macrophage population during the first months after CCR5Δ32/Δ32 SCT. Later in the course of immune reconstitution, host-originating macrophages became undetectable in the GI mucosa by both phenotypic and genotypic analysis. These findings suggest that the replacement of host tissue cells with donor-derived cells has reduced the size of the viral reservoir during the course of immune reconstitution and, consequently, has lowered the risk of HIV rebound over time. Cell replacement in tissues under posttransplantation conditions may even allow for complete eradication of HIV; however, the unfeasibility to analyze every single cell in living humans rules out the possibility to positively prove viral eradication in this patient.
In summary, our results demonstrate successful CD4+ T-cell reconstitution at the systemic level as well as in the largest immunologic organ after CCR5Δ32/Δ32 SCT and in addition provide evidence for the reduction in the size of the potential HIV reservoir over time. Although the recovered CD4+ T cells are susceptible to infection with X4 HIV, the patient remains without any evidence of HIV infection for more than 3.5 years after discontinuation of ART. From these results, it is reasonable to conclude that cure of HIV infection has been achieved in this patient.
An Inside Blood analysis of this article appears at the front of this issue.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 USC section 1734.
Acknowledgments
We are grateful to the patients for their participation in this project. We thank Diana Bösel and Simone Spiekermann for excellent technical assistance and Désirée Kunkel from the Berlin-Brandenburg Center for Regenerative Therapies for technical support with cell sorting.
This work was supported by a research funding from the German Research Foundation (DFG KFO104) to K.A. and T.S. The HIV-1 molecular clone pNL4-3 from Dr Malcolm Martin was provided by the EU Program EVA Center for AIDS Reagents, NIBSC (AVIP Contract Number LSHP-CT-2004-503487). HIV-1 JR-CSF from Dr Isy Chen was provided from the WHO-UNAIDS Virus Network through the Center for AIDS Reagents.
Authorship
Contribution: K.A. designed experiments; K.A., J.H., and C.L. performed experiments and analyzed data; K.A. and C.L. composed the figures; K.A., G.H., J.H., and T.S. interpreted and discussed the data; G.H., K.R., and E.T. collected data; E.T. critically revised the manuscript for important intellectual content; T.S. supervised the research; K.A. wrote the manuscript; and all authors read and approved the manuscript.
The current affiliation for G.H. is the Institute of Transfusion Medicine and Immunology, University Heidelberg, Germany. The current affiliation for C.L. is the Department of Pathology, Technische Universität München, Munich, Germany.
Conflict-of-interest disclosure: The authors declare no competing financial interests.
Correspondence: Kristina Allers, Department of Gastroenterology, Infectious Diseases, and Rheumatology, Medical Clinic I, Campus Benjamin Franklin, Charité-University Medicine, Hindenburgdamm 30, 12203 Berlin, Germany; e-mail: kristina.allers@charite.de.