To the editor:
Maternal and fetal cells are in close contact during fetal development in the maternal uterine environment. Fetal cells can routinely be identified in the maternal circulation; less so maternal cells in the fetus. As such, feto-maternal and materno-fetal cell trafficking is an accepted concept today.1-4 The clinical consequences are not yet fully understood and represent a field of increasing current interest. If indeed feto-maternal and materno-fetal cell trafficking were a 2-way process, transfer of cells via maternal transit should be possible from a sibling born earlier to a sibling born later. A sibling donor born before his recipient (ie, donor older than recipient) should therefore tolerize the younger recipient, transplants from a sibling older than the recipient should less likely be rejected than transplants from a sibling younger than the recipient; a donor younger than the recipient should induce less graft-versus-host disease (GVHD) after hematopoietic stem cell transplantation (HSCT). Data from our previously reported retrospective single-center cohort study of 311 consecutive transplantations indeed showed a significantly better survival of patients who were first-born in their family and had received a HSCT from a human leukocyte antigen (HLA)–identical younger sibling.5 These data were confirmed by another small single-center study.6 Because of the fundamental implications of these findings, we attempted to solidify the results in an analysis of 2 large independent retrospective cohorts of HLA-identical sibling donor transplantations.
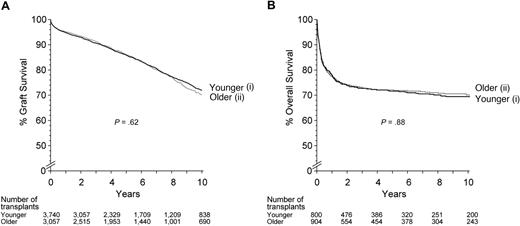
We analyzed 6062 HLA-identical living sibling donor kidney transplantations (3391 donors younger and 2671 donors older than the recipient), and 1704 HLA-identical sibling donor HSCTs for aplastic anemia (800 donors older and 904 donors younger than the recipient) performed between 1980 and 2007 for survival, graft survival, and death-censored graft survival (kidney grafts) or for incidence of graft rejection, patient survival, and probability of transplantation-related mortality (HSCT for aplastic anemia). In contrast to expectations, results were identical between the 2 donor groups. There was no difference in patient survival or death-censored graft survival for recipients of a kidney transplant from a younger compared with an older sibling (Figure 1A). There was no difference in graft rejection, transplantation-related mortality, or overall survival after HSCT for aplastic anemia (Figure 1B). This absence of a survival difference was confirmed in multivariate analyses after adjustment for known risk factors for graft outcome.
Outcome of HLA–identical sibling transplantations by birth order. (A) Graft survival of 6062 living HLA–identical sibling donor kidney allografts by birth order. (i) Donor younger than recipient. (ii) Donor older than recipient. Ten-year graft survival hazard ratio (HR) of older versus younger donor = 1.06 (95% confidence interval, 0.94-1.20; P = .37). (B) Graft survival of 1704 allogeneic HSCTs from HLA–identical sibling donors for aplastic anemia by birth order. (i) Donor younger than recipient. (ii) Donor older than recipient. Ten-year patient survival HR of older versus younger donor = 1.126 (95% confidence interval 0.914-1.388; P = .265).
Outcome of HLA–identical sibling transplantations by birth order. (A) Graft survival of 6062 living HLA–identical sibling donor kidney allografts by birth order. (i) Donor younger than recipient. (ii) Donor older than recipient. Ten-year graft survival hazard ratio (HR) of older versus younger donor = 1.06 (95% confidence interval, 0.94-1.20; P = .37). (B) Graft survival of 1704 allogeneic HSCTs from HLA–identical sibling donors for aplastic anemia by birth order. (i) Donor younger than recipient. (ii) Donor older than recipient. Ten-year patient survival HR of older versus younger donor = 1.126 (95% confidence interval 0.914-1.388; P = .265).
These data from 2 large well-defined groups of patients failed to show a significant impact of birth order in sibling donor transplantation. Probably, long-term survival of fetal cells in the circulation of the mother, a prerequisite for transfer to an afterborn sibling, is a very rare event. So far it has not been possible to identify with certainty circulating fetal cells in women long after birth. This would still be compatible with the tolerization concept in mother-to-child haploidentical HSCT.7 Alternatively, sensitization and tolerization occur with similar frequency and balance each other out in a large analysis. Both ways, the results speak against the postulated hypothesis of a clinically significant impact of feto-maternal materno-fetal cell trafficking in organ transplantation.
Authorship
Acknowledgments: This work was supported by the Collaborative Transplant Study, by the European Group for Blood and Marrow Transplantation (EBMT), its members and its corporate members, as well as in part by the European LeukemiaNet LSH-2002-22.0-3, by a grant from the Swiss National Research Foundation 3200B0-118176, and by the Swiss Cancer League.
Contribution: A.G., C.B., and G.O. designed the study concept; B.D., M.S., and J.P. performed the statistical analysis; G.O. and J.P. were responsible for the international data collection; A.G. wrote the paper; and all authors helped with the manuscript and approved the final version.
Conflict-of-interest disclosure: The authors declare no competing financial interests.
Correspondence: Prof Dr Alois Gratwohl, Hematology and Stem Cell Transplant Unit, University Hospital, Petersgraben 4, CH-4031 Basel, Switzerland; e-mail: hematology@uhbs.ch.