Abstract
Abstract 3346
Poster Board III-234
Patients who receive high-dose chemotherapy with or without radiation preparative regimens prior to allogeneic hematopoietic stem cell transplant (AHSCT) have high incidence of mucositis. The mucositis is usually seen at the nadir of neutropenia and improves with engraftment. At our center we observed late onset mucositis in patients received intravenous IV Busulfan/Fludarabine (IV-BU/FLU) preparative regimen. The onset was within 5 days of engraftment and resolved 5 days after engraftment (peri-engraftment mucositis, PEM). Upon review of literature, no reports were found that detailed this phenomenon. We attempted to determine the incidence of PEM in our patient population, as well as possible risk factors and consequences.
This retrospective chart review was designed as a cohort study. It included 382 patients who received AHSCT at Karmanos Cancer Center between 2004 and 2009; out of these were 207 patients received IV-BU/FLU; 103 patients received myeloablative dose of BU 130mg/m2 daily x 4 doses starting at day -6 and FLU 30mg/m2 daily x five doses starting at day -6. 104 patients received reduced intensity regimen of IV BU 130mg/m2 daily x 2 doses starting day -6, FLU 30mg/ m2 daily x 5 doses starting day -6, and 200 rad total body irradiation TBI (IV-BU/FLU/TBI). All patients received tacrolimus and mycophenolate for GVHD prophylaxis starting at day -3, with no methotrexate. We attempt to define this entity by examining the clinical course and correlations of diagnosis, preparative regimen, patient characteristics (age, race, weight, height, grade and duration of mucositis, opiate use, and engraftment associated acute leukocytosis) and patient outcomes (hospitalization duration, incidence of acute GvHD, survival).
A total of 207 patients received IV- BU/FLU and 175 patients received other preparative regimens. The incidence of peri-engraftment mucositis was 19% (39/207), in the group receiving IV-BU/FLU, while with other regimens it was 1 % (2/174). There was no difference in the distributions of the diagnosis, patient characteristics or patient outcomes among those who received IV-BU/FLU versus those who received other preparative regimen. Due to high incidence of this phenomenon observed in patients who received BU/FLU, this patient group was further studied. On evaluation of these patients (n=207), 9 (4%) patients were not assessable for mucositis, 62 (30%) had no mucositis and 136 (66%) developed mucositis.
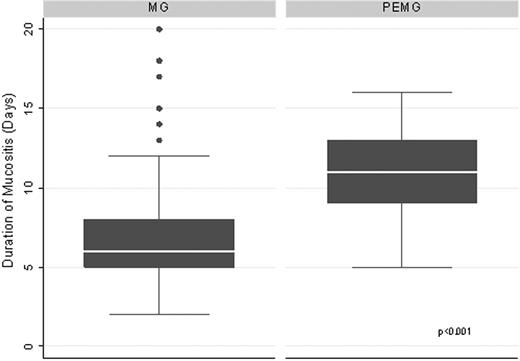
Of the 136 pts with mucositis, 39 (29%) met predefined criteria for peri-engraftment mucositis (PEM). PEM (N=39) group characteristics: Mean age is 50 (20-67). 34 patients had IV-BU/FLU and 5 IV-BU/FLU/TBI. Diagnosis: 22 AML, 6 MDS, 4 CML, 2 NHL, 2 CLL, 1each with CMML, HD, ALL. 16 patients had related AHSCT and 23 had unrelated AHSCT. All PEM patients were tested and found negative for herpes simplex virus infection at the time of PEM. The median engraftment day for both mucositis group (MG) and peri-engraftment mucositis (PEMG) group was day +11. The median duration of mucositis (6 vs. 11 days, p < 0.001), incidence of intravenous (iv) opiate usage (62% vs. 82%, p 0.023), median duration of iv opiate usage (5 vs. 7 days, p< 0.001), Mucositis grade 3 (21% vs. 43 % p < 0.001 value) and median duration of hospitalization (24 vs. 31 days, p< 0.001) were different in MG (N=97) vs. PEMG(N=39) group, respectively. The p values were calculated using wilcoxan rank sum test. No significant differences in other patient characteristics or other patient outcomes were observed in the MG vs. PEMG.
BU/FLU regimen has been in use for less than a decade. Peri-engraftment mucositis has not been described previously with this regimen. PEM is a unique phenomenon, with features including; longer duration (Fig1), more incidence of grade 3 mucositis, higher incidence and longer duration of iv opiate use and longer hospitalization. Although the pathophysiology of PEM remains unclear and no specific risk factors have been identified for it, this phenomenon increases patients' morbidity and cost of transplant.
Showing the difference in the duration of mucositis in MG vs. PEMG group
Lum:Transtarget Corporation: Founder. Abidi:Merck Pharmaceuticals: Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.