Abstract
Abstract 3201
Poster Board III-138
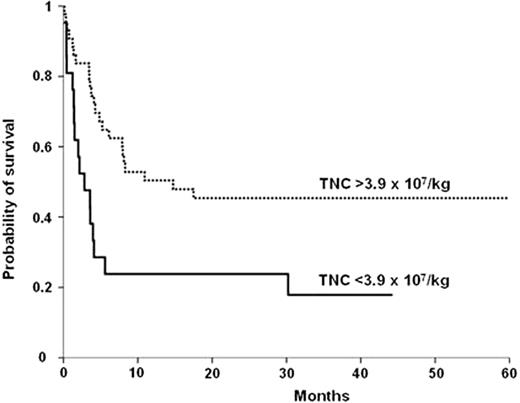
The outcome of patients with severe aplastic anemia (SAA) has greatly improved in recent years, but is still poor for patients who lack a sibling donor and who failed or relapsed after immunosuppressive therapy (IST). Recently, transplantation from unrelated donors has improved significantly. Umbilical cord blood transplantation (UCBT) has extended the availability of HSCT in the absence of a suitable donor but very little data is available in the setting of SAA. We conducted a retrospective analysis on 71 patients (33 male) diagnosed with SAA (9 with PNH) who received a single UCBT (n=57, 79%) or double UCBT (n=14, 19%) from January 1996 to January 2009 in 32 centers (23 EBMT centers). The median age was 13 years (range 2-68 years; 28 adults). Median disease duration before UCBT was 14 months (2-140). Fifty five patients (89%) received immunosuppressive therapy before transplantation and most patients were highly transfused prior to UCBT. Seven percent of cord blood units were identical to recipients (antigen level for HLA-A and B and allelic level for DRB1), 28% of units had 1 HLA mismatch and 65% had 2 or 3 HLA disparities. Median infused cell dose was 4.3 ×107 TNC/Kg (2.1-34.9) and 2.1 ×105 CD34 cells/Kg (0.4-19) for single UCBT and 7.4 ×107 TNC/Kg (5-14.7) and 3.5 ×105 CD34 cells/Kg (1-8.7) for double UCBT. Forty six patients (69%) received a reduced intensity conditioning regimen, most of which were fludarabine-based. Twenty three patients received a total body irradiation (2 Gray, n= 11) and antithymoglobulin was given to 53 patients (79%). Graft-versus host disease (GVHD) prophylaxis consisted mainly of cyclosporin+steroids (70% of patients). Cumulative incidence (CI) of neutrophil recovery (>500mm≥) at day 60 was 51±6% with a median time of 25 days (6-91). In multivariate analysis, the only factor associated with shorter time to engraftment and higher probability of engraftment was pre-freezing TNC dose (>3.9 107/Kg, HR: 1.5, 95%CI: 1-2.2, p=0.05). Chimerism analysis for patients who engrafted (n=37) showed full donor chimerism in 82%. The CI of grade II-IV acute GVHD was 20±5% (10 grade II, 5 grade III, 2 grade IV). Eleven patients of 34 at risk developed chronic GVHD leading to a CI of 18±5% at 3 years. With a median follow-up of 35 months (3 - 83), the estimated probability of 3-years overall survival (OS) was 38±6%. The main cause of death was graft failure associated with infections (n=14, 32%). In multivariate analysis, the only factor associated with survival was pre-freezing TNC dose (>3.9 107/Kg, RR: 0.4, 95%CI: 0.2-0.8, p=0.007). The estimated probability of 3-year overall survival (OS) for patients who received more than 3.9 107/Kg TNC was 45% compared to 18% for those who received less (Figure 1). Other factors such as number of HLA disparities or use of single or double CB unit were not associated with any outcome. However, the 3-year OS after single CBT was 37% and 43% after double CBT. In conclusion, this study highlights the fundamental role of the TNC dose (>3.9 × 107/kg TNC/Kg) on both engraftment and overall survival using cord blood as stem cell source in SAA. It could justify the use of double cord blood transplant if necessary for this indication. Graft failure remains a major issue in this particularly high risk population. Prospective well designed trials are necessary before the inclusion of UCBT in the treatment strategy of advanced severe aplastic anemia.
Estimate 3-year overall survival according to the TNC dose
Estimate 3-year overall survival according to the TNC dose
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.