In this issue of Blood, Verneris and colleagues report that patients receiving 2 partially HLA-matched cord blood units have significantly less leukemia relapse than patients receiving 1 partially HLA-matched cord blood unit in myeloablative transplantation.
Since the success of the first related cord blood transplantation in 1989, cord blood transplantation has developed into a viable option for patients in need of hematopoietic stem cell transplantation who do not have a matched donor.1,2 Because of the biological naivety of cord blood stem cells, there is less graft-versus-host (GVH) disease in cord blood recipients compared with bone marrow recipients.3 The widespread storage of cord units means donor units can be rapidly identified and available for patients in need.2 Cord blood also presents challenges for successful transplantation; lower available cell doses have led to delayed neutrophil and platelet engraftment in pediatric and especially in adult transplantation patients.3,4
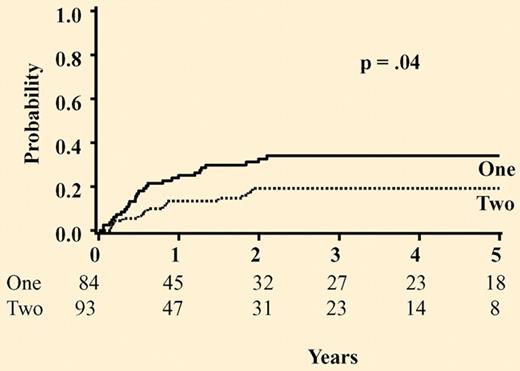
Probability of leukemia relapse for all patients based on the number of units infused. See the complete figure in the article beginning on page 4293.
Probability of leukemia relapse for all patients based on the number of units infused. See the complete figure in the article beginning on page 4293.
To overcome the significant barrier of low cell dose in adult transplantation candidates, researchers at the University of Minnesota pioneered an approach of using 2 partially HLA-matched cord blood units.5 They found improved engraftment and noted that one cord predominated donor marrow reconstitution within months of successful transplantation. Research continues to determine what factors most strongly affect outcome following double cord blood transplantation (ie, degree of human leukocyte antigen [HLA] match, GVH severity, relapse, and/or engraftment kinetics).6-8
In all transplantation settings, leukemia relapse following transplantation continues to be an impediment to long-term survival, although rates are similar among peripheral blood, bone marrow, and cord blood transplant recipients.4 Clinical GVH has been correlated with less leukemia relapse, as presumably the donor cells produce both antitumor and antihost effects during the process.9 Because cord blood transplantation is generally associated with less GVH, there has been concern over the graft-versus-leukemia effect (GVL) and prevention of disease relapse.
In this issue of Blood, Verneris et al offer a retrospective combined adult and pediatric cohort analysis for leukemia relapse following myeloablative transplantation comparing outcome in recipients of 1 or 2 partially HLA-matched cord blood units.10 They used a cell dose threshold to determine whether patients should receive one or two 4/6 HLA-matched or better cord blood units (HLA-A,B typed by intermediate resolution, HLA-DRB1 typed by allele level resolution). Recipients of 2 cord units received more CD34+ cells and T cells, and were exposed to more disparate HLA antigens. Both double- and single-cord recipients engrafted in a similar time frame; double-cord unit recipients engrafted with only 1 of the 2 units long-term, as has been previously described.5 The incidence of grade 2-4 acute graft-versus-host disease (aGVHD) was found to be significantly higher in patients who received 2 cord units and an unadjusted trend was detected for more severe (grade 3-4) aGVHD and chronic GVHD in double-cord patients over single-cord recipients. These results support recent findings that double-cord transplantation has a higher rate of GVH than single-cord blood transplant recipients, suggesting that the presence of 2 units creates an environment that facilitates host alloreactivity.8
Next, the authors attempt to link the GVH findings to relapse rate by comparing patients who received 1 or 2 cord blood units. The rate of relapse in the entire cohort was 29%, with those with advanced disease (≥ CR3 or not in remission) having a higher chance of relapse. Using unadjusted analyses, at 5 years after transplantation, those patients who received 2 cords, whether with early stage (CR1-2) or not, had less relapse than those who received only 1 cord (19% vs 34%). Moreover, those double-cord patients in early-stage remission (CR1-2) were significantly less likely to have leukemia relapse that those who received 1 cord, when controlling for other variables such as diagnosis, conditioning regimen, GVH prophylaxis, HLA match, and cell dose. These data suggest that the presence of 2 donors in the recipient creates an environment that facilitates leukemia alloreactivity or GVL effect.
The study presents intriguing data that add to the biological understanding of how the infusion of 2 cord blood donors can affect transplantation outcomes. Because the patients were acquired over 14 years, the cell dose threshold used to select 1 or 2 cord units and treatment regimens changed over time. Moreover, the rate of clinical GVH was not found to be significantly associated with leukemia relapse in the cohort. It is also important to note that overall and leukemia-free survival did not differ between the groups, suggesting that the small sample size and retrospective study design may have affected the findings. At this time, several randomized studies are comparing 1 to 2 cord blood units. These results, as well as translation research, are needed to understand the cellular interactions between cords and host in double-cord blood transplantation. The future will undoubtedly uncover scientific mechanisms that will expand our understanding of the emerging therapy of double cord blood hematopoietic stem cell transplantation.
Conflict-of-interest disclosure: The author declares no competing financial interests. ■