Abstract
CEBPA mutations have been associated with improved outcome in adult acute myeloid leukemia (AML). We evaluated the prevalence and prognostic significance of CEBPA mutations in 847 children with AML treated on 3 consecutive pediatric trials. Two types of CEBPA mutations—N-terminal truncating mutations and in-frame bZip-domain mutations—were detected in 38 (4.5%) of 847 patients tested; 31 (82%) of 38 patients with mutations harbored both mutation types. Mutation status was correlated with laboratory and clinical characteristics and clinical outcome. CEBPA mutations were significantly more common in older patients, patients with FAB M1 or M2, and patients with normal karyotype. Mutations did not occur in patients with either favorable or unfavorable cytogenetics. Actuarial event-free survival at 5 years was 70% versus 38% (P = .015) with a cumulative incidence of relapse from complete remission of 13% versus 44% (P = .007) for those with and without CEBPA mutations. The presence of CEBPA mutations was an independent prognostic factor for improved outcome (HR = 0.24, P = .047). As CEBPA mutations are associated with lower relapse rate and improved survival, CEBPA mutation analysis needs to be incorporated into initial screening for risk identification and therapy allocation at diagnosis. The clinical trials in this study are registered at http://www.clinicaltrials.gov under NCT00002798 and NCT00070174.
Introduction
CCAAT/enhancer binding protein-alpha (C/EBPα, encoded by the gene CEBPA) is a transcription factor that regulates proliferation and controls terminal granulocytic differentiation.1 Functional alterations in CEBPA have been identified in acute myeloid leukemia (AML),2,3 a heterogeneous disease that accounts for 15% to 20% of leukemia in children. At present, cytogenetic analysis at diagnosis is used to stratify patients into favorable, adverse, or intermediate risk groups,4 with implications for risk-adapted therapy. However, patients with normal cytogenetics represent more than 20% of all children with AML,5 and the intermediate risk group comprises 60% to 70%. Recent work has identified novel molecular markers, such as internal tandem duplications of the juxtamembrane domain of the FLT3 gene (FLT3/ITD)6-9 and mutations in exon 12 of nucleophosmin (NPM1),10-14 with prognostic implications that may be used to further refine risk. CEBPA mutations have been the subject of current investigations to determine their role as another potential molecular marker of prognosis in AML.
C/EBPα is the original member of the basic region leucine zipper class of transcription factors.15-17 The C/EBPα protein consists of 2 N-terminal transactivation domains, a basic DNA-binding region, and a C-terminal leucine zipper.18 Wild-type (WT) C/EBPα exists in 2 translational isoforms, p42 and p30. The shorter isoform is generated from a second internal start codon within the same open reading frame.19 C/EBPα is expressed in a variety of tissues, where it plays an important role in the differentiation of many cell types, including adipocytes,20 hepatocytes,21 and type II alveolar cells.22 In regard to hematopoiesis, C/EBPα is expressed in cells of myelomonocytic origin and regulates the expression of several granulocyte-specific genes.23 It has been shown to inhibit E2F pathways,24 down-regulating c-Myc and thus allowing myeloid precursors to enter the pathway toward granulocytic differentiation.25 C/EBPα expression is crucial to the development and terminal differentiation of granulocytes from bipotential precursors.26
Several common patterns of CEBPA mutations have been described in AML.27 In the N-terminus, small out-of-frame insertions or deletions occur resulting in a premature stop codon, which abolishes transcription of the p42 product. In this setting, p30 is solely expressed and acts in a dominant negative manner.2 In the bZip region, in-frame duplications or deletions disrupt the phasing of the leucine zipper, in turn disrupting DNA binding function as well as dimerization.3 N-terminal truncating mutations and bZip mutations often occur together.28-31 CEBPA mutations have been reported in 4% to 11% of adult AML patients2,3,28-30 and are associated with improved outcome.29-31 An initial small pediatric study reported CEBPA mutations in 7 (6%) of 117 children with AML32 but did not report outcome data. In this study we present a comprehensive, retrospective evaluation of the prevalence and prognostic significance of CEBPA mutations in a large cohort of patients with pediatric AML.
Methods
Patient samples
Newly diagnosed pediatric patients with de novo AML enrolled in 3 consecutive pediatric AML trials, CCG-2941, CCG-2961, and COG-AAML03P1, were eligible for this study. CCG-2961 and its preceding pilot, CCG-2941, enrolled a total of 988 pediatric patients with de novo AML. Details of CCG-2941 and CCG-2961 have been previously described.33 The COG-AAML03P1 study enrolled 340 pediatric patients (> 1 month to < 21 years old) with newly diagnosed de novo AML. Patients with any diagnosis of acute promyelocytic leukemia, Down syndrome, prior myelodysplastic syndrome, or inherited bone marrow failure syndromes were excluded. This pilot study evaluated the efficacy and safety of a 5-cycle modified MRC-like chemotherapy regimen that included the administration of gemtuzumab ozogamicin (GO) in selected cycles. Chemotherapy treatment included induction 1: cytarabine, daunorubicin, and etoposide (ADE) in addition to GO; induction 2: ADE; intensification 1: cytarabine and etoposide (AE); intensification 2: mitoxantrone and cytarabine (MA) in addition to GO; and intensification 3: cytarabine, asparaginase, and daunorubicin (Capizzi II). Patients with HLA-suitable sibling donors were nonrandomly assigned to bone marrow transplantation after completion of intensification 1.
Of the 1328 patients treated on the 3 consecutive studies, available diagnostic specimens from 847 patients were obtained from the COG AML Reference Laboratory for this study. Four patients with a diagnosis of granulocytic sarcoma with no morphologic evidence of bone marrow involvement were enrolled in the 3 studies. No tissue specimen was available from the chloroma in these cases. Mutation analysis was performed on the DNA extracted from the diagnostic marrow of all patients. Institutional review board approval was obtained before mutation analysis from the Fred Hutchinson Cancer Research Center, and this study was approved by the COG Myeloid Disease Biology Committee. Informed consent was obtained in accordance with the Declaration of Helsinki.
Detection of CEBPA mutations
Genomic DNA was extracted from the diagnostic marrow specimens using the Puregene protocol (Gentra Systems, Minneapolis, MN). Polymerase chain reaction (PCR) amplification of the entire coding region of CEBPA was performed using 4 overlapping primer pairs, as previously described.31 Fragment-length analysis was performed using Genescan software (Applied Biosystems, Foster City, CA). Mutations were confirmed via direct sequencing using the Thermo Sequence Dye Terminator (GE Healthcare, Piscataway, NJ) sequencing reaction.
Statistical methods
The Kaplan-Meier method was used to estimate overall survival (OS), event-free survival (EFS), and disease-free survival (DFS). OS was defined as time from study entry to death. EFS was defined as the time from study entry until death, failure to achieve complete remission (CR) by the end of 2 courses of therapy, or relapse. DFS was defined as the time from the end of course 1 for patients in CR until death, failure to achieve CR by the end of course 2 therapy, or relapse. Estimates of relapse risk (RR) were obtained using methods that account for competing events. RR was defined as the time from remission at end of course 1 to relapse where deaths from nonprogressive disease were considered competing events. The significance of predictor variables was tested with the log-rank statistic for OS, EFS, and DFS and with Gray statistic for RR. Patients who also underwent allogeneic hematopoietic stem cell transplantation (allo-HSCT) while on study were censored at the time of transplantation for all analyses. Patients lost to follow-up were censored at their date of last known contact or at a cutoff 6 months before the current date of analysis (October 14, 2004, for patients on CCG-2941; April 30, 2006, for patients on CCG-2961; and January 25, 2008, for patients on COG-AAML03P1). The significance of observed differences in proportions was tested using the χ2 test and Fisher exact test when data were sparse. The Mann-Whitney test was used to determine the significance between differences in medians. The Cox proportional hazards model was used to estimate hazard ratios (HRs) for univariate and multivariate analyses.
Results
Patient population
From September 1995 to November 2005, 1328 pediatric AML patients were treated on CCG-2941, CCG-2961, and COG-AAML03P1. Of these, 847 (64%) had diagnostic bone marrow specimens available for analysis. Demographics, laboratory and clinical characteristics, and outcome for those with and without available specimens were compared. Patients without available diagnostic specimens (n = 481) had similar clinical outcomes with 5-year OS of 52% plus or minus 6% compared with 53% plus or minus 4% for those who were analyzed (P = .736). Induction CR rates and EFS from study entry were also similar. The study population differed from those not tested mainly in regard to age and diagnostic white blood cell count (WBC), where those not tested were younger (median age: 6.6 years vs 10.2 years, P < .001) and had lower median diagnostic WBC (14.35 × 109/L vs 22.00 × 109/L, P = .001). In addition, the population that was not tested had a higher proportion of patients with megakaryocytic leukemia (10% vs 4%, P < .001).
CEBPA mutation analysis
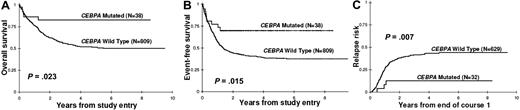
All available diagnostic specimens from patients enrolled on CCG-2941, CCG-2961, and COG-AAML03P1 were analyzed for CEBPA mutations. The entire coding region of the CEBPA gene was screened in 4 segments in CCG-2941 and CCG-2961 patients (N = 590). A total of 46 mutations were detected in 25 patients (4.2%), corresponding with the 2 patterns of functional alterations (Figure 1): N-terminal domain (NTD) mutations resulting in a premature stop codon (n = 22), or in-frame insertions or deletions in the bZip region (n = 24) disrupting the leucine zipper. Nineteen patients had out-of-frame NTD mutations, of which 7 were insertions, ranging from 1- to 7-bp long, and 13 were deletions, ranging from 1- to 17-bp long, all of which resulted in a shift in the reading frame that would lead to a truncated protein. Three patients had a 2-bp deletion/2-bp insertion mutation that produced a nonsense codon at amino acid position 87, also resulting in a truncated protein. Twenty-four patients had an in-frame C-terminal bZip domain mutation; 21 were insertions or duplications ranging from 3- to 36-bp long, and 3 were deletions ranging from 3- to 18-bp long. Of note, 21 (84%) of 25 patients with functional mutations harbored “double” mutations, pairing an NTD truncating mutation with a C-terminal in-frame bZip mutation. Of the patients with a bZip mutation, 21 (88%) of 24 carried a corresponding N-terminal mutation. Of the patients with truncating NTD mutations, 21 (95%) of 22 carried a corresponding bZip mutation.
CEBPA mutations, CCG-2941/2961 and COG-AAML03P1. (A) Fragment-length analysis, showing representative mutations. NTD: (i) wild type; (ii) 1-bp deletion; (iii) 4-bp insertion. bZip: (iv) wild type; (v) 6-bp insertion; (vi) 24-bp insertion. (B) Location of each functional mutation. Mutations that are one of a pair of CEBPA mutations within the same patient, or “double” mutations, are depicted in red. Polymorphisms are not shown. (C) Thirty-one patients (82% of those with mutations) harbored “double” mutations, pairing an N-terminal truncating mutation with an in-frame bZip mutation. Of the patients with “single” mutations, only one patient had an NTD mutation alone.
CEBPA mutations, CCG-2941/2961 and COG-AAML03P1. (A) Fragment-length analysis, showing representative mutations. NTD: (i) wild type; (ii) 1-bp deletion; (iii) 4-bp insertion. bZip: (iv) wild type; (v) 6-bp insertion; (vi) 24-bp insertion. (B) Location of each functional mutation. Mutations that are one of a pair of CEBPA mutations within the same patient, or “double” mutations, are depicted in red. Polymorphisms are not shown. (C) Thirty-one patients (82% of those with mutations) harbored “double” mutations, pairing an N-terminal truncating mutation with an in-frame bZip mutation. Of the patients with “single” mutations, only one patient had an NTD mutation alone.
CEBPA mutation analysis was then performed in the NTD and the bZip domain on all available specimens from the AAML03P1 study (N = 257). A total of 23 mutations were detected in 13 (5%) patients. Ten (4%) of 257 patients harbored N-terminal truncating mutations; in-frame bZip mutations were found in 13 (5%) patients. Of the 13 patients with mutations, 10 patients harbored double mutations. All 10 patients with NTD mutations had corresponding bZip mutations; 3 patients harbored bZip mutations alone.
Overall, we detected CEBPA mutations in 38 (4.5%) of 847 patients (Table 1). “Double” mutations were common, occurring in 31 (82%) of 38 patients with mutations (Figure 1C). In patients in whom only one CEBPA mutation was detected, this “single” mutation occurred in the bZip domain in 6 of 7 patients. In all 847 patients screened, only a single patient had a truncating NTD mutation alone.
Polymorphisms are common in the CEBPA gene
Sequence alterations in the TAD2 region were seen in 44 (7.5%) of the 590 patients screened from CCG-2941/2961, of whom 41 had a 6-bp duplication (584-589dup) and an additional 3 had a 9-bp deletion (558-566del). Forty-three of these patients had no additional mutations of the CEBPA gene; a single patient with 584-589dup also harbored both an N-terminal frameshift and an in-frame bZip mutation. Such TAD2 domain sequence alterations have been demonstrated in the healthy population and in AML patients in remission, and are considered to be non-AML–associated polymorphisms.28,34,35 Paired remission samples were available for 4 patients with the TAD2 584-589dup. Evaluation of these remission specimens detected the presence of this duplication in the TAD2 domain in all 4 cases, as would be expected in the setting of a germ-line polymorphism. As a result, those with TAD2 domain alterations without additional CEBPA mutations were analyzed as WT in outcome analysis. We also identified 2 patients with a novel in-frame 3-bp duplication (311-313dup) in the NTD domain. In contrast to other NTD mutations, this mutation would not result in an early termination codon. As a result, we questioned whether 311-313dup might be a polymorphism as well. Evaluation of remission specimens from these 2 patients also confirmed the presence of the identical alteration in the remission samples, and they were analyzed as WT for outcome analysis.
Characteristics of the study population
Demographic, laboratory, and clinical characteristics of patients with and without CEBPA mutations were compared (Table 2). Those with and without CEBPA mutations were similar in sex distribution. Patients with CEBPA mutations had a higher median age than those without mutations (13.5 years vs 10 years, P = .004) as such mutations were less common in the younger patients between the ages of 0 to 2 years (P = .075) and more common in patients older than 10 years (71% of patients with CEBPA mutations were in this age group, as opposed to 45% of patients without mutations, P = .002). Patients with CEBPA mutations had a higher diagnostic hemoglobin (P = .004) and lower diagnostic platelet count (P = .002) than patients with wild-type CEBPA.
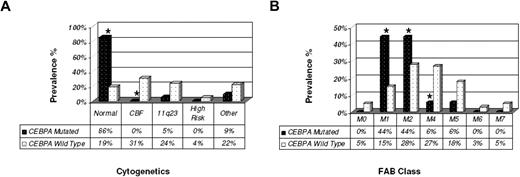
For the 489 patients with known cytogenetic data, the presence of CEBPA mutations was evaluated in the following cytogenetic subgroups: favorable risk, defined as t(8;21) or inv(16) (the core binding factor [CBF] leukemias); unfavorable risk, defined as −5/del(5q) or −7; and intermediate risk, defined as all othercytogenetic subtypes. CEBPA mutations were exclusively observed in patients with intermediate-risk cytogenetics, and predominantly observed in those with normal karyotype (Figure 2A); 86% of patients with CEBPA mutations had normal cytogenetics, as opposed to 19% of patients without CEBPA mutations (P < .001). In fact, patients with CEBPA mutations accounted for 17% of all patients with normal cytogenetics in our cohort. CEBPA mutations were not observed in patients with either CBF AML or unfavorable risk cytogenetics. Most (88%) CEBPA mutations occurred in FAB M1 and M2 (Figure 2B). CEBPA mutations were uncommon in FAB M4 and M5, and were not seen in FAB M6 and M7.
Cytogenetics and FAB class of patients with and without CEBPA mutations. (A) CEBPA mutations were found overwhelmingly in the cytogenetically normal cohort, and did not occur in either favorable (CBF AML) or unfavorable risk groups. (B) CEBPA mutations were most commonly found in FAB M1 and M2. Statistically significant differences are denoted with an asterisk.
Cytogenetics and FAB class of patients with and without CEBPA mutations. (A) CEBPA mutations were found overwhelmingly in the cytogenetically normal cohort, and did not occur in either favorable (CBF AML) or unfavorable risk groups. (B) CEBPA mutations were most commonly found in FAB M1 and M2. Statistically significant differences are denoted with an asterisk.
Other known AML-related molecular abnormalities occurred infrequently in the CEBPA-mutated cohort. FLT3/ITD occurred in 2 patients with CEBPA double mutations; WT1 mutations, in 3 patients with CEBPA double mutations; and NPM1 mutation, in 1 patient with a CEBPA double mutation (who also harbored a WT1 mutation). None of these abnormalities occurred in patients with CEBPA single mutations (Table 2).
Clinical outcome and prognostic impact of CEBPA mutations
The CR rate was determined for all patients following the first course of induction therapy. Patients with and without CEBPA mutations had a similar response to induction therapy where 32 (84%) of 38 patients with CEBPA mutations achieved CR, compared with 629 (80%) of 787 patients without CEBPA mutations (Table 2, P = .518).
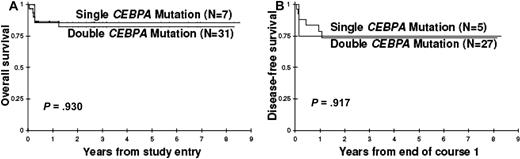
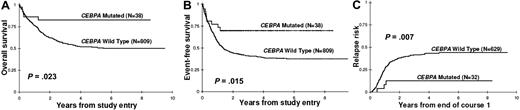
Clinical outcome was examined for the 847 patients with known CEBPA mutation status (Figure 3). Actuarial overall survival (OS) at 5 years from diagnosis was 83% plus or minus 13% for patients with CEBPA mutations, and 51% plus or minus 5% for patients without (HR = 0.40, P = .023). Patients with CEBPA mutations had an EFS at 5 years from study entry of 70% plus or minus 16%, compared with 38% plus or minus 4% for those without mutations (HR = 0.47, P = .015). Of the 661 patients who achieved an initial CR, cumulative relapse rate at 5 years from remission was 13% plus or minus 14% for those with CEBPA mutations, and 44% plus or minus 5% for those without (P = .007). Corresponding DFS from CR in patients with and without CEBPA mutations was 74% plus or minus 17% and 47% plus or minus 5%, respectively (HR = 0.50, P = .065).
Clinical significance of CEBPA mutations in pediatric AML. Kaplan-Meier estimates for (A) overall survival and (B) event-free survival from study entry for patients with and without CEBPA mutations. (C) Cumulative incidence of relapse is also presented.
Clinical significance of CEBPA mutations in pediatric AML. Kaplan-Meier estimates for (A) overall survival and (B) event-free survival from study entry for patients with and without CEBPA mutations. (C) Cumulative incidence of relapse is also presented.
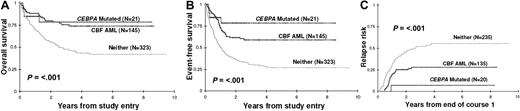
For patients with known diagnostic cytogenetic information, clinical outcome of those with CEBPA mutations was compared with that of patients with CBF AML (Figure 4). Patients with CEBPA mutations had an OS similar to those with CBF AML (78% ± 18% vs 74% ± 9%, HR = 1.00; P = .999). Cumulative incidence of relapse at 5 years from remission was 7% plus or minus 13% for patients with CEBPA mutations compared with 28% plus or minus 10% for those with CBF AML (P = .090). EFS was 78% plus or minus 19% for those with CEBPA mutation and 59% plus or minus 10% for those with CBF AML (HR = 0.56, P = .264).
Clinical outcomes for patients with CEBPA mutations versus core binding factor AML versus neither. (A) Overall survival and (B) event-free survival from study entry, as well as (C) relapse risk from first CR for patients with and without CEBPA mutations compared with those with CBF AML.
Clinical outcomes for patients with CEBPA mutations versus core binding factor AML versus neither. (A) Overall survival and (B) event-free survival from study entry, as well as (C) relapse risk from first CR for patients with and without CEBPA mutations compared with those with CBF AML.
Clinical outcome by CEBPA mutation status was also examined separately in the normal cytogenetic cohort, for those with known cytogenetics. Patients with normal cytogenetics with CEBPA mutations had superior OS compared with that of patients with WT CEBPA and normal cytogenetics (80% ± 21% vs 38% ± 13%; P = .039). EFS was similarly improved in patients with CEBPA mutations (80% ± 21%) compared with those without (30% ± 13%; P = .011). For those with normal cytogenetics, cumulative incidence of relapse at 5 years from remission was 9% plus or minus 17% in the CEBPA-mutated group versus 49% plus or minus 15% in the WT CEBPA group (P = .026). The presence of a CEBPA mutation predicted favorable prognosis even when analysis was restricted to those with normal-karyotype AML. Of note, the 2 CEBPA-mutated patients with WT1 mutations died of progressive disease during induction 2, whereas the patient with CEBPA, NPM1, and WT1 mutations was alive at last contact. One patient with FLT3/ITD experienced CNS relapse but was successfully salvaged and alive at last contact.
In the protocols presented, 168 total patients underwent a matched sibling donor (MSD) allo-HSCT following the third course of therapy. For patients in CR by the end of induction 2, we directly compared the outcome of CEBPA mutation–positive patients who underwent a MSD HSCT (n = 7) with that of those treated with chemotherapy only (n = 20). In patients with CEBPA mutations, RR (cumulative incidence) at 5 years from end of course 2 was 14% plus or minus 26% for those who underwent HSCT versus 16% plus or minus 16% for those who were treated with chemotherapy only (P = .998). Corresponding OS at 5 years from end of course 2 was 57% plus or minus 37% versus 90% plus or minus 14% (P = .054) for those who underwent HSCT and chemotherapy-only recipients, respectively. Of the 7 patients with CEBPA mutations who underwent allo-HSCT in remission, 2 patients died of treatment-related causes, and 1 patient died of relapsed disease. Of the CEBPA-mutated patients in CR by end of course 2 who received chemotherapy alone (n = 20), 1 patient died of treatment-related toxicity and 1 patient, from progressive disease. Patients with CEBPA mutations did not appear to benefit from allo-HSCT.
As COG-AAML03P1 differed substantially from the prior CCG-2941/2961 studies, we questioned whether the clinical significance of CEBPA mutations differed between the treatment protocols. The type of therapy did not appear to affect the favorable prognostic implications of CEBPA mutations. In both treatment protocols, patients with CEBPA mutations trended toward an improved outcome. In CCG-2941/2961, OS at 5 years from study entry for those with mutations was 78% plus or minus 17%, versus 50% plus or minus 5% for those without mutations (P = .078). In AAML03P1, those with CEBPA mutations had a 3-year OS from study entry of 92% plus or minus 16%, versus 60% plus or minus 9% for those without mutations (P = .154). Event-free survival at 5 years from study entry was 69% plus or minus 20% versus 37% plus or minus 5% for those with and without mutations enrolled on 2941/2961 (P = .040), whereas in AAML03P1, EFS at 3 years from study entry was 71% plus or minus 29% versus 37% plus or minus 14% (P = .215) for those with and without mutations. Relapse rate for patients with and without CEBPA mutations was 12% plus or minus 16% versus 45% plus or minus 6% for 2941/2961 (P = .019), and 15% plus or minus 28% versus 43% plus or minus 13% (P = .188) for AAML03P1. Patients with CEBPA mutations showed a trend toward improved outcome in all measures in each individual study, and combined analysis of all studies provided the power to detect statistically significant differences in outcome between patients with and without mutations.
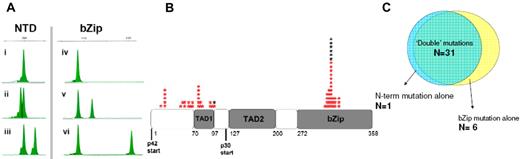
Clinical implication of single versus double mutations
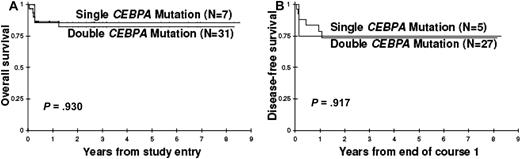
Cooperation of N-terminal truncating and bZip domain mutations is considered necessary and sufficient for the evolution of AML. Thus, patients with a single CEBPA mutation may represent a distinct biologic entity from those with double mutations. To determine whether these 2 groups of patients may have disparate outcomes, we compared the clinical outcome of patients with either single NTD or bZip domain mutations (n = 7) with those with dual NTD and bZip domain mutations (n = 31). In this analysis, those with a single mutation had nearly identical OS (P = .930) and DFS (P = .917) to those with double mutations (Figure 5). No patients with a single CEBPA mutation harbored other known molecular alterations (FLT3/ITD, NPM1 mutation, or WT1 mutation) or abnormal cytogenetics.
Comparison of clinical outcome for patients with “single” versus “double” CEBPA mutations. Patients with one CEBPA mutation had nearly identical (A) overall survival and (B) disease-free survival curves to those with 2 mutations.
Comparison of clinical outcome for patients with “single” versus “double” CEBPA mutations. Patients with one CEBPA mutation had nearly identical (A) overall survival and (B) disease-free survival curves to those with 2 mutations.
Prognostic factors
Prognostic factors were evaluated for EFS from study entry and RR from CR. We used Cox regression analysis to evaluate CEBPA mutation status, presence of high-risk FLT3/ITD (ITD with allelic ratio > 0.4),9 diagnostic WBC, and unfavorable risk (−7, −5/del5q) as well as favorable risk (CBF AML) cytogenetics, as predictors of EFS and RR in a univariate model that is stratified by the study in which each patient is enrolled (Table 3). In the univariate model, the presence of a CEBPA mutation was a significant prognostic factor for improved EFS with an HR of 0.47 (P = .015). In separate univariate models, high-risk FLT3/ITD (HR = 1.9, P < .001), diagnostic WBC more than 100 × 109/L (HR = 1.31, P = .010), and unfavorable risk cytogenetics (HR = 2.13, P < .001) were associated with worse EFS. Those with CBF AML had a favorable outcome compared with those without CBF AML (HR = 0.47, P < .001). In this univariate model, the presence of a CEBPA mutation was associated with a lower RR (HR 0.26, P = .19). In a multivariate model that included the previously mentioned prognostic factors and was stratified by study, the presence of CEBPA mutations remained an independent prognostic factor for EFS (HR = 0.36, P = .024). In this multivariate analysis, CBF AML, unfavorable risk cytogenetics, and high-risk FLT3/ITD were independent prognostic factors for EFS (Table 3). Multivariate analysis of the prognostic factors for RR demonstrated that the presence of CEBPA mutations is an independent prognostic factor for improved relapse risk (HR = 0.24, P = .047).
Discussion
This retrospective study demonstrates that pediatric AML patients with CEBPA mutations have a significantly lower risk of relapse and improved survival compared with their counterparts with wild-type CEBPA. The presence of a CEBPA mutation is shown to be an independent prognostic factor of favorable outcome. We also demonstrate that the majority of patients have mutations in both the NTD and the bZip domain, a fact that may be significant in the stepwise evolution of AML.
Pediatric AML patients with CEBPA mutations show a striking absence of other cytogenetic or known molecular abnormalities. This may suggest that AML arising in the setting of CEBPA mutations follows a relatively simple pathway to leukemogenesis. In fact, we found that the most common second molecular event in a patient with one CEBPA mutation is a second CEBPA mutation. There are data to suggest that these mutations are biallelic.28 An NTD mutation resulting in an early termination codon truncates the p42 protein, allowing intact translation of only the p30 protein. In a biallelic model, the bZip mutation in the opposite allele disrupts the bZip domains of its protein products, resulting in loss of function. Such a biallelic mutation would result in the expression of p30 as the only functional protein. Kirstetter et al36 recently found that sole expression of p30 may be sufficient for the development of AML. In their mouse model, expression of the p30 isoform in the absence of p42 resulted in a fully penetrant AML phenotype. This model would argue that both mutations are required for AML pathogenesis. Constitutional N-terminal CEBPA mutations have been described in several kindred of familial AML,37,38 possibly suggesting that a truncating mutation of the NTD may be the initial “hit” that requires the evolution of the second event for development of the AML phenotype. Patients with single CEBPA mutations may acquire the second event in a manner other than primary mutation of the CEBPA gene.
Functional CEBPA mutations are undetectable in complete remission, yet mutations identical to those at diagnosis almost always occur at relapse.39,40 However, novel CEBPA mutations have not been described to occur in relapse. Taken together, these data suggest that loss of function of CEBPA is important for leukemogenesis in both the de novo and relapsed setting, but is not related to the progression of disease.
The fact that patients with CEBPA mutations have such a favorable outcome may suggest that these mutations evolve in a more differentiated cell population. We have previously reported a close link between the lineage involvement of the AML-related mutation and response to therapy, where patients whose FLT3/ITD involved the CD34+/CD33− early progenitors had more resistant disease, whereas those with the mutation limited to the more differentiated CD34+/CD33+ population had a more favorable outcome.41 Demonstration of restricted involvement of the CEBPA mutation may justify efforts toward therapies directed at this more differentiated population. Restoring or enhancing CEBPA expression may have therapeutic ramifications for these patients as well. In fact, the triterpenoid CDDO has been shown to induce differentiation and apoptosis of AML cells via CEBPA translational up-regulation.42
The high frequency of double mutations, and the fact that single NTD mutations are rare events, will help streamline molecular screening for CEBPA mutations in clinical trials. Fragment-length analysis of the bZip region would allow identification of the overwhelming majority of CEBPA mutations and provide a rapid screening tool for identification of those with favorable prognosis. This approach would entail a shorter turnaround time, obviate the need for sequencing, and avoid detection of nonpathogenic polymorphisms, which are not found in the bZip region. We recommend bZip fragment-length analysis as a rapid and specific clinical test for detecting CEBPA mutations.
Patients with CEBPA mutations represent 4.5% of our study population, but account for 17% of the cohort with normal cytogenetics, comparable with what has been reported in adult studies of AML patients with normal karyotype.31 Further, of the 38 patients with CEBPA mutations in our study, all except 1 patient with FLT3/ITD with high allelic ratio would have been classified as intermediate risk using current risk-stratification schemes. Since approximately 60% of pediatric AML patients lack either favorable or unfavorable markers, biomarkers for risk identification in these intermediate risk patients are needed for more appropriate therapy allocation. We propose that CEBPA mutation screening should be included in the molecular characterization of pediatric AML at diagnosis, and that patients with CEBPA mutations should be prospectively stratified into the favorable risk treatment group. These patients, like those with CBF AML, have favorable survival rates and low relapse risk. Thus, patients with CEBPA mutations may not benefit from HSCT in first remission. In our retrospective analysis, only 7 patients with CEBPA mutations underwent allo-HSCT. However, the difference in OS between CEBPA-mutated patients who underwent HSCT (57% ± 37%) compared with those who received chemotherapy alone (90% ± 14%, P = .054) is striking, as 2 of the 7 CEBPA-mutated patients who underwent HSCT suffered toxicity-related deaths, and 1 patient died of relapse following transplantation. Given that patients with CEBPA mutations have a favorable outcome with chemotherapy and there are no data to suggest any benefit from HSCT, we conclude that patients with CEBPA mutations should be prospectively stratified into chemotherapy-only treatment. As CEBPA mutations lead to myeloid maturation arrest, novel differentiating agents may provide future therapeutic options for managing these favorable risk patients while minimizing treatment-related toxicity.
An Inside Blood analysis of this article appears at the front of this issue.
The online version of this article contains a data supplement.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 USC section 1734.
Acknowledgments
We thank Ms Cristina Galer for excellent technical contribution to this work, and the Children's Oncology Group Acute Myeloid Leukemia Reference Laboratory for providing diagnostic specimens. We are grateful to the patients and families who consented to the use of biologic specimens in these trials.
This work was supported by the National Institutes of Health (Bethesda, MD; grants R21 CA10262-01 and R01 CA114563-01, and Children's Oncology Group Chair's grant NIH U10 CA98543) and the National Cancer Institute (Bethesda, MD; grant T32 CA009351).
National Institutes of Health
Authorship
Contribution: P.A.H. designed research, performed research, analyzed data, and wrote the paper; T.A.A. served as senior statistician, performed statistical analyses, and edited the paper; R.B.G. performed statistical analyses and edited the paper; J.P., D.L.S., C.H., N.A.H., B.H., S.C.R., and J.P.R. analyzed data and edited the paper; B.L. and J.L.F. served as clinical study PIs and edited the paper; and S.M. designed research, analyzed data, and wrote the paper.
A complete list of Children's Oncology Group participants can be found in the Supplemental Appendix (available on the Blood website; see the Supplemental Materials link at the top of the online article).
Conflict-of-interest disclosure: The authors declare no competing financial interests.
Correspondence: Phoenix Ho, Fred Hutchinson Cancer Research Center, D2-373, 1100 Fairview Ave N, Seattle, WA 98109; e-mail: pho@fhcrc.org.