Abstract
We report the use of NT-ProBNP (N-terminal fragment of brain natriuretic peptide) as an independent marker to identify patients with AL amyloidosis whose clonal response to chemotherapy is inadequate. The aim of chemotherapy is to allow improvement in amyloidotic organ function but the significant time lag often means that patients are either over or under treated. Use of biomarkers (such as BNP and NT-ProBNP) for risk stratification is an area of increasing interest.
200 patients with AL amyloidosis diagnosed between 2004–2007, who had completed one line of treatment and had a complete results available prior to and six month from the start of treatment, were identified from the databases of the Amyloidosis centres in Pavia, Italy and London, UK. Organ involvement and response was assessed according to the international consensus criteria (Gertz et al 2005). NT-ProBNP change was deemed significant if there was a rise or fall of both 30% and >300 ng/L over the starting value. Kaplan-Meier and Cox regression were used for survival analysis as appropriate. The median age was 63 yrs (range 38–83) and the median number of organs involved was 2. 132 (66%) had cardiac involvement, 150 (75%) had renal and 42 (21%) had liver involvement at presentation. 115 (56%) responded to chemotherapy with a complete response (CR) in 34 (17%) and a partial response in 81 (40%).
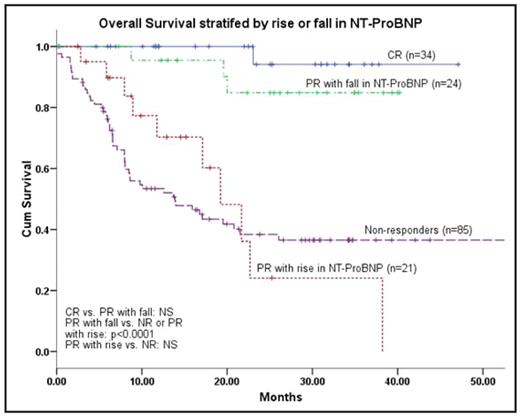
At baseline, median NT-ProBNP was 1865 ng/L (range 50–70144) and was >332 ng/L (the cut-off reported as significant by Dispenzieri et al, J Clin Oncol 2004) in 159 patients (80%). The median follow-up was 23 months. The median overall survival (OS) has not been reached with an estimated 2 yr survival of 71%. Patients with cardiac involvement had worse outcomes (OS 29 mo vs. not reached; p =0.001) whereas renal, liver, neuropathy, soft tissue involvement, the light chain type or presence of a measurable M protein did not significantly impact survival. Haematologic responders had a significantly better overall survival (median not reached) than non-responders (median 22 months; p<0.0001) with those achieving CR having significantly better survival than PR (estimated 4 year survival of 94% and 65% respectively; p=0.005).
The NT-proBNP increased and decreased significantly in 45 (22%) and 92 (46%) respectively - with the latter group achieving lower FLC concentration after treatment (27.6 vs. 96.4 mg/L, p<0.0001).16 of the 22 (73%) patients with heart involvement who obtained CR also has decreases in NT-ProBNP. Patients without significant NT-ProBNP decrease (median OS 29 months vs. not reached) or with significant increase (median OS 20 months vs. not reached) had significantly poorer outcome (p<0.0001). The impact of this was most marked in patients achieving a PR – in this group, the estimated 3 year survival was 48% for patients in whom there was an increase in NT-ProBNP (not significantly different from the non-responders) vs. 86% for patient in whom there was a decrease (not significantly different from those who achieved CR) (log rank p<0.0001, see figure). On multivariate analysis, cardiac involvement and change NT-ProBNP were highly significant independent prognostic factors.
In summary, patients who have a fall in NT-ProBNP have excellent outcomes irrespective of the degree of haematological response. Conversely, the failure to see a fall or to see an increase in NT-ProBNP clearly identifies a group of patients with AL amyloidosis, who despite a haematologic response to treatment, have significantly poorer outcomes. A prospective randomised study to see the effects of rapidly changing to alternative treatment in the latter groups is being planned.
Disclosures: No relevant conflicts of interest to declare.
Author notes
Corresponding author