Abstract
Patients with acute lymphoblastic leukemia (ALL) and an intrachromosomal amplification of chromosome 21 (iAMP21) comprise a novel and distinct biological subgroup. We prospectively screened 1630 (84%) patients treated on the UK MRC ALL97 protocol for iAMP21 and herein present demographic, clinical, and survival data on the 28 (2%) children found to harbor this abnormality. They had a common or pre-B ALL immunophenotype, were significantly older (median 9 years vs 5 years), and had a lower white cell count (median 3.9 vs 12.4) compared with children without this abnormality. Notably, patients with iAMP21 had a significantly inferior event-free and overall survival at 5 years compared with other patients: 29% (95% confidence interval [CI], 13%-48%) versus 78% (95% CI, 76%-80%) and 71% (95% CI, 51%-84%) versus 87% (95% CI, 85%-88%), respectively. As a result of this 3-fold increase in relapse risk, newly diagnosed patients with iAMP21 recruited to the current UK MRC ALL2003 trial are being treated on the high-risk arm and are considered for bone marrow transplantation in first remission.
Introduction
We have recently defined a novel, recurrent chromosomal abnormality in a distinct subgroup of childhood acute lymphoblastic leukemia (ALL), which is characterized by the presence of an intrachromosomal amplification of chromosome 21 (iAMP21).1–3 Despite variability between patients in the morphology of the abnormal chromosome 21, they consistently show multiple, extra copies of the RUNX1 (AML1) gene, tandemly repeated along the length of the abnormal chromosome.1 Genomic and expression analysis has further characterized this abnormality, demonstrating a common region of amplification (CRA) between 33.192 and 39.796 Mb on chromosome 21 (which includes RUNX1).3 In addition, gene expression profiling comparing patients with iAMP21 with other children with ALL found that 10% of the genes overexpressed among patients with iAMP21 were located within the CRA.3 Preliminary survival analysis of these patients suggested that they had a increased risk of relapse.2 Here, we present a detailed survival analysis of 28 children with ALL and iAMP21 treated on the UK MRC ALL97 trial.
Patients and methods
All patients had a confirmed diagnosis of ALL and were recruited to the UK Medical Research Council (MRC) ALL97 treatment trial.4 Local Ethical Committee approval was obtained by treating centers, and informed consent was given by parents and/or patients. The basic treatment template was an initial 3-drug induction phase followed by 2 intensification modules, maintenance, 2 short delayed intensification phases, and continuing therapy for a total of 2 years.4 The trial contained both a steroid and purine randomisation. In 1999, BFM-type intensification modules5 replaced the previous UK versions, and age and presenting white cell count (WCC) were used to risk stratify patients into regimens A (standard risk) or B (high risk). This phase of the trial was designated ALL97/99. The speed of response was assessed at day 8 for regimen B (4-drug induction and BFM consolidation) or day 15 for regimen A (3-drug induction and standard consolidation). Patients with more than 25% blasts in their bone marrow (BM) at the relevant time point were transferred to regimen C (very high risk). In addition, patients with high-risk cytogenetics and those who failed to remit by day 29 were transferred to regimen C.
Pretreatment BM or peripheral blood samples were sent for cytogenetic analysis at the time of diagnosis to regional centers and were subsequently reviewed and collated centrally by the Leukaemia Research Cytogenetics Group (LRCG).6 Fixed-cell suspensions from the same diagnostic sample were screened prospectively, either locally or centrally, using the LSI TEL-AML1 ES Dual Colour Translocation probe (Abbott Diagnostics, Maidenhead, United Kingdom) regardless of the patients' presentation features or the presence of other cytogenetic abnormalities.7 Patients with 5 or more signals from the AML1 probe corresponding to 3 or more extra copies of the RUNX1 gene on a single abnormal chromosome 21 were classified as having an iAMP21.1,2 Patients were also classified according to the presence of t(12;21)(p13;q22)/ETV6-RUNX1, high hyperdiploidy (51-65 chromosomes; HeH), t(9;22)(q34;q11)/BCR-ABL, 11q23/MLL translocation, near haploidy (23-29 chromosomes), or low hypodiploidy (30-39 chromosomes) on the basis of conventional cytogenetic analysis or fluorescence in situ hybridization (FISH) using commercially available probes for BCR-ABL and MLL, as previously described.7
The main survival analyses are of event-free survival (EFS) and overall survival (OS), defined as time to the first adverse event, whether relapse or death (including nonremitters and those who died in remission), or death, respectively. Patients who did not suffer an event or die within the follow-up period were censored on October 31, 2005. Kaplan-Meier life tables and curves were constructed by means of the log-rank method. The observed-expected ratios were generated from unadjusted log-rank tests comparing 2 groups. Multivariate analysis was performed using the Cox proportional hazards model. The chi-squared test was used to examine the distribution of categorical variables.
Results and discussion
A total of 1935 patients were treated on ALL97 and 1630 (84%) were prospectively screened for iAMP21. This abnormality was detected in 28 (2%) patients. All patients with iAMP21 had common/pre-B ALL and an L1 French-American-British (FAB) morphology. They were significantly older, had a lower WCC, and a lower platelet count compared with the rest of the cohort (Table 1). However, they showed no sex bias. There was no difference between patients with iAMP21 and other patients with respect to the following diagnostic variables: central nervous system (CNS) disease, percentage of BM blasts, splenomegaly, hepatomegaly, anterior mediastinal mass, or hemoglobin count (Table 1). None of the patients with iAMP21 had Down syndrome, and their ethnicity was consistent with the cohort as a whole (Table 1). No other significant recurrent chromosomal abnormality was observed in any of the patients. Soulier et al8 reported 16 patients with iAMP21 and reviewed clinical data from 14 further patients from the literature. The sex (17 boys to 13 girls), age (median, 11.5 years; range, 3-19 years), WCC (median, 4.9 × 109/L; range, 1-26 × 109/L), and immunophenotypic (all common/pre-B ALL) profiles of these 30 patients were consistent with those of our patients (Table 1).
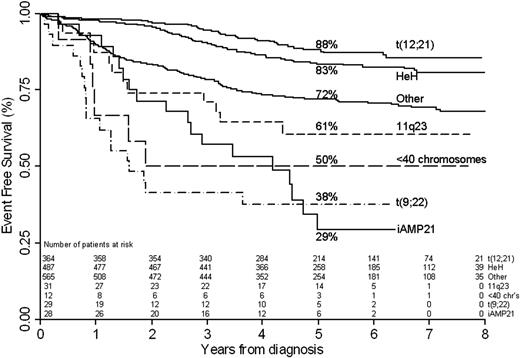
All (96%) but 1 of the patients with iAMP21 achieved a complete remission (CR), albeit with 3 patients requiring in excess of 35 days of treatment (47, 49, and 55 days, respectively). The 1 remaining patient achieved a good partial remission (6% residual blasts) after consolidation but died 8 months after diagnosis from pneumonia. To date, a total of 17 (61%) patients with iAMP21 have relapsed, which is significantly more than expected. The 5-year EFS was 29% (95% confidence interval [CI], 13%-48%), which is significantly worse than expected (Table 1) and comparable with other poor-risk cytogenetic subgroups (Figure 1). Patients with iAMP21 suffered either isolated BM relapses (n = 11), isolated CNS relapses (n = 5), or a combined BM and CNS relapse (n = 1) (Table 1). Eight (47%) of the relapses occurred while the patients were still on treatment, which included 4 of the isolated CNS relapses. The remaining 9 (53%) relapses occurred between 8 months and 3 years off therapy. The 10 patients in continuing CR have been off treatment for between 4 months and 4.6 years. The OS at 5 years was 71% (95% CI, 51%-84%), which is significantly lower than expected, although not as low as the EFS might suggest. Among the 17 relapsed patients with iAMP21, 8 (47%) have died, 2 following a second relapse. The median time to death after relapse was 4 months. The median follow-up time for the iAMP21 cohort was 4 years and 10 months, and 5 years and 3 months for the other patients. Multivariate analysis confirmed that the presence of the iAMP21 chromosomal abnormality was an independent indicator of poor EFS and OS (Tables 2-3). When the effects of sex, age, and WCC within the iAMP21 cohort were assessed by Cox regression analysis, none were found to be statistically significant. In view of the fact that none of the patients with iAMP21 had T-cell ALL (T-ALL), we repeated the analyses restricting the cohort to those with B-cell precursor (BCP) disease. The exclusion of patients with T-ALL made no difference to the results, and patients with iAMP21 were older, had a lower WCC and platelet count, and had a poorer outcome compared with other patients with BCP-ALL (data not shown).
EFS of patients treated on UK MRC ALL97 by cytogenetic subgroup. iAMP21 indicates intrachromosomal amplification of chromosome 21q; t(12;21), t(12;21)(p13;q22)/ETV6-RUNX1; HeH, high hyperdiploidy (51-65 chromosomes); t(9;22), t(9;22)(q34;q11)/BCR-ABL; 11q23, 11q23/MLL translocation; less than 40 chromosomes (chrs), near-haploidy (23-29 chromosomes), or low hypodiploidy (30-39 chromosomes); and other, all other patients.
EFS of patients treated on UK MRC ALL97 by cytogenetic subgroup. iAMP21 indicates intrachromosomal amplification of chromosome 21q; t(12;21), t(12;21)(p13;q22)/ETV6-RUNX1; HeH, high hyperdiploidy (51-65 chromosomes); t(9;22), t(9;22)(q34;q11)/BCR-ABL; 11q23, 11q23/MLL translocation; less than 40 chromosomes (chrs), near-haploidy (23-29 chromosomes), or low hypodiploidy (30-39 chromosomes); and other, all other patients.
The iAMP21 subgroup was not defined or linked to a poor outcome until 2003; hence, the front-line therapy of these children would not have been altered as a result of its presence. Only 6 of these patients were treated as high-risk on the basis of other factors. Among the 10 patients treated on ALL97, only one was independently classified as high risk by the Oxford Hazard Score,4 and the patient was treated on the high-risk arm and received a transplant in first remission. The remaining 18 patients were treated on ALL97/99 and assigned to regimens A (n = 10) or B (n = 8) according to age and WCC. Five of these patients were subsequently transferred to regimen C because they failed to remit (n = 1) or were classified as a slow early responder (n = 4). The difference between the EFS and OS suggests that relapsed patients might be salvageable. However, the follow-up of the 9 relapsed patients with iAMP21 that remained alive was highly variable, with 4 patients having less than 1 year post-relapse follow-up. There was no standard treatment after relapse, and all were treated off protocol. However, 8 patients with iAMP21 have received a bone marrow transplant in second remission. Four of these patients subsequently died (one after a second relapse), and the remaining 4 are surviving between 4 and 44 months after transplantation. It is intended to further monitor all surviving patients with iAMP21 over an extended period.
In conclusion, we have demonstrated that patients with ALL and iAMP21 have a 3-fold increased risk of relapse and are twice as likely to die compared with their counterparts without this abnormality. This is the first report to accurately assess the prognosis of patients harboring this abnormality, and we eagerly await results from other cooperative study groups. In light of these findings, the UK MRC/NCRI Childhood Leukaemia Working Party have recommended that patients with iAMP21 treated on the current trial, ALL2003,9 be transferred to the high-risk arm and, in association with a slow early response, be considered for transplantation in first remission.
Authorship
Author contribution: A.V.M. designed and performed the study, analyzed the data, and wrote the manuscript; C.J.H., J.C.S., and H.M.R. analyzed cytogenetic and FISH data and helped design the study; S.M.R. collected trial data and was the trial statistician; and B.E.S.G., S.E.K., T.O.B.E., A.J.V., and C.D.M. coordinated the trial on which the patients were treated. All authors critically reviewed the manuscript.
A complete list of the members of the UK MRC/NCRI CLWP appears as a data supplement to the online version of this article.
Conflict-of-interest statement: The authors declare no competing financial interests.
Correspondence: Anthony V. Moorman, Leukaemia Research Cytogenetics Group, Cancer Sciences Division, University of Southampton, MP 822, Duthie Building, Southampton General Hospital, Southampton, SO16 6YD, United Kingdom; e-mail: avm@soton.ac.uk.
The online version of this article contains a data supplement.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 USC section 1734.
Acknowledgments
Supported by Leukaemia Research, London, United Kingdom.