Abstract
The Children's Cancer Group (CCG) 1952 clinical trial for children with standard-risk acute lymphoblastic leukemia (SR-ALL) compared intrathecal (IT) methotrexate (MTX) with IT triples (ITT) (MTX, cytarabine, and hydrocortisone sodium succinate [HSS]) as presymptomatic central nervous system (CNS) treatment. Following remission induction, 1018 patients were randomized to receive IT MTX and 1009 ITT. Multivariate analysis identified male sex, hepatomegaly, CNS-2 status, and age younger than 2 or older than 6 years as significant predictors of isolated CNS (iCNS) relapse. The 6-year cumulative incidence estimates of iCNS relapse are 3.4% ± 1.0% for ITT and 5.9% ± 1.2% for IT MTX; P = .004. Significantly more relapses occurred in bone marrow (BM) and testicles with ITT than IT MTX, particularly among patients with T-cell phenotype or day 14 BM aspirate containing 5% to 25% blasts. Thus, the estimated 6-year event-free survivals (EFS) with ITT or IT MTX are equivalent at 80.7% ± 1.9% and 82.5% ± 1.8%, respectively (P = .3). Because the salvage rate after BM relapse is inferior to that after CNS relapse, the 6-year overall survival (OS) for ITT is 90.3% ± 1.5% versus 94.4% ± 1.1% for IT MTX (P = .01). It appears that ITT improves presymptomatic CNS treatment but does not improve overall outcome.
Introduction
Presymptomatic central nervous system (CNS) therapy changed the prognosis of acute lymphoblastic leukemia (ALL) in the early 1970s. Before then, more than half of the complete remissions induced by combination chemotherapy ended in CNS relapse. With the combination of 2400 cGy cranial irradiation (cXRT) and intrathecal (IT) therapy, fewer than 10% of cases recurred in the CNS and almost 50% of patients achieved long-term survival.1 Since that time, progressively more intensive systemic and IT regimens have largely replaced cXRT in the treatment of childhood ALL.2-6 IT methotrexate (MTX), dosed by age rather than body surface area, has been the standard IT therapy used in Children's Cancer Group (CCG) protocols for treatment of de novo ALL.3,7 Seeking greater efficacy of CNS-directed therapy, some investigators and cooperative groups have added IT cytarabine and/or corticosteroids to MTX in pursuit of additive benefit or synergy.6,8-13 However, investigations assessing the benefit of these drug combinations in vitro or in animal models in vivo are inconclusive, as results show both antagonism and synergy.14-18
At the time the CCG 1952 phase 3 study was designed, the isolated CNS (iCNS) relapse rate among children with standard-risk (SR) and low-risk ALL treated with IT MTX on CCG protocols was 6% to 8%, representing one third of all relapses.19,20 In contrast, the iCNS relapse rate among relatively similar patients treated with IT triples (ITT) (MTX, cytarabine, and hydrocortisone sodium succinate [HSS]) on the Pediatric Oncology Group (POG) AlinC13 study was 3%.21 The disparity in study cohorts and differences in systemic therapy, timing, and frequency of IT administration have prevented meaningful comparisons of the 2 IT regimens across protocols. Consequently, the CCG 1952 trial was conceived as a direct comparison of IT MTX and ITT. Using a 2 × 2 factorial design, CCG 1952 compared outcome among patients treated with (1) either postinduction IT MTX or ITT as CNS-directed therapy and with (2) either mercaptopurine (MP) or thioguanine (TG) as the maintenance thiopurine. This report concerns the IT comparison; the thiopurine question is the topic of a separate report.
Patients, materials, and methods
Patients
CCG 1952 opened in May 1996 and completed accrual in February 2000. Eligible patients were 1 to less than 10 years of age with presenting white blood cell (WBC) count below 50 × 109/L (National Cancer Institute, SR-ALL criteria).22 Diagnosis of ALL required a bone marrow (BM) aspirate with more than 25% L1 or L2 lymphoblasts by French-American-British (FAB) morphology, negative histochemical staining for myeloperoxidase, and reactivity with monoclonal antibodies to B-lineage– or T-lineage–associated differentiation antigens, as previously described.23,24 Patients with L3 morphology or with t(8;14), t(8;22), or t(2;8) were excluded. Patients with corticosteroid exposure for more than 48 hours during the preceding month were ineligible.
Treatment protocol
The National Cancer Institute and institutional review boards of all participating CCG institutions approved the study. Written informed consent was obtained from guardians or parents according to the guidelines of the National Institutes of Health. Patients received 3-drug induction therapy with 1 dose of IT cytarabine, intravenous vincristine, oral prednisone, intramuscular native Escherichia coli asparaginase, and 2 doses of IT MTX as detailed in Table 1. Patients with CNS-1 (CSF WBC count below 5/μL without blasts) and CNS-2 status (CSF WBC count below 5/μL with blasts present on cytocentrifuge preparation) or traumatic taps received identical IT and systemic therapy. CNS leukemia, or CNS-3, was defined as CSF WBC count at least 5/μL and a cytocentrifuge preparation demonstrating leukemic blasts, or clinical signs such as facial nerve palsy or hypothalamic syndrome even when CSF WBC count was normal. If the patient had leukemic cells in the peripheral blood and the lumbar puncture was traumatic and contained at least 5/μL WBCs with blasts, the following algorithm was used to define CNS disease: If the CSF WBC/RBC ratio was greater than the WBC/RBC ratio of the peripheral blood, the patient was considered as having CNS-3 status. Patients were said to have had a traumatic tap with blasts (TLP+) when their CSF had a red blood cell (RBC) count of at least 10/μL and blasts without meeting the algorithm criteria for CNS-3.
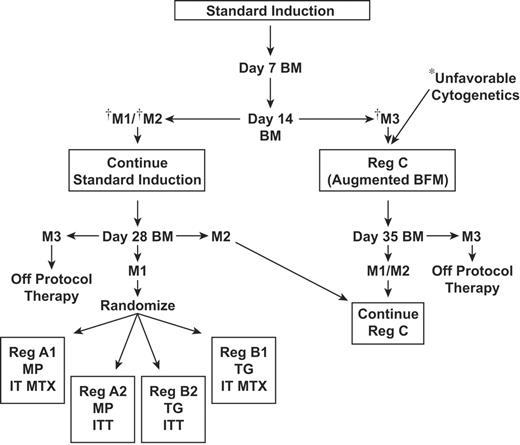
BM status was determined by local institutions: fewer than 5% blasts (M1), 5% to 25% blasts (M2), and more than 25% blasts (M3). Patients who were M2 or M3 on day 7 were reassessed with aspirates on day 14. Randomization required M1 or M2 status by day 14, remission status (M1) at day 28 of induction, and no unfavorable leukemia cytogenetics (t(4;11), t(9;22), or hypodiploidy with fewer than 45 chromosomes). Patients who did not meet randomization criteria were assigned to more intensive therapy (Figure 1).
At the end of induction, eligible patients were assigned randomly by the CCG central statistical office in Arcadia, CA, in a 2 × 2 factorial design to 1 of 4 treatment regimens, as shown in Figure 1: regimen A1: oral MP and IT MTX; regimen A2: oral MP and ITT; regimen B1: oral TG and IT MTX; regimen B2: oral TG and ITT. IT MTX and ITT doses were age adjusted using standard mg per age range, as shown in Table 2.
Details of therapy within each phase appear in Table 1. Girls were treated for 2 years and boys for 3 years from the start of interim maintenance (IM). Girls were to receive 19 IT injections and boys 23 throughout their entire course of treatment, including induction. Children with overt CNS disease received 2400 cGy cranial and 600 cGy spinal irradiation during consolidation; patients with testicular involvement received 2400 cGy testicular irradiation. The backbone therapy of CCG 1952 was based on the results of CCG-1891, which suggested that double delayed intensification (DI) improved the outcome of children with SR-ALL.19 Prednisone was given in induction and maintenance; dexamethasone was given in the DI phases.
Genetic and BM evaluations
Cytogenetics were performed on diagnostic BM samples at local institutions using standard techniques and nomenclature.25,26 The CCG Cytogenetics Committee centrally reviewed each karyotype. TEL/AML1 expression was analyzed by reverse transcriptase–polymerase chain reaction (RT-PCR) in the CCG ALL Reference Laboratory on blasts from the first 1000 subjects. RT-PCR was performed using the conditions and primers reported by Shurtleff et al.27 Local institutions determined BM blast percentage on day 7 and day 14 aspirates, as has been standard on Children's Oncology Group (COG) protocols.28,29
CCG 1952 treatment schema. *t(9;22)(q34;q11), t(4;11)(q21;q23), or hypodiploidy with fewer than 45 chromosomes. †See “Treatment protocol” for definitions.
CCG 1952 treatment schema. *t(9;22)(q34;q11), t(4;11)(q21;q23), or hypodiploidy with fewer than 45 chromosomes. †See “Treatment protocol” for definitions.
Statistical methods
Sample size and power calculations for the CCG 1952 study were initially based on an expected long-term event-free survival (EFS) plateau of 80% and a freedom from CNS relapse of 94% in the control regimens of the 2 × 2 factorial design. Initial accrual was planned for 3 years, with approximately 564 patients randomized each year. An accrual of 1692 patients was intended to have in excess of 80% power (2-sided log-rank test) to detect an improvement to 87.5% EFS (relative hazard rate [RHR] = 0.5984) in half the subjects and an 86% power to detect improvement to 97% freedom from CNS relapse (RHR = 0.4923) in half the subjects. The analysis of treatment effects of either of the main factors (MP versus TG, IT MTX versus ITT) employed a stratified life table analysis (stratified for the remaining factor), giving a type of pooled results across the strata. There was no apparent biologic or other reason to anticipate interaction effect on outcome. In the actual study analysis, tests for statistical interaction of the IT regimens with the systemic chemotherapy regimens were performed using a Cox regression test.30,31 Once open to accrual, the study was monitored with interim analyses by the independent CCG Data Monitoring Committee (DMC) using a Lan-DeMets spending function approach.32,33 Because fewer events had occurred than expected on the control regimens by the middle of 1999, the DMC approved extending accrual for 6 additional months and 300 more patients to ensure at least 80% power for the EFS comparisons.
Randomization to 1 of 4 treatment regimens occurred at the end of induction. Outcome comparisons used an intent-to-treat approach. Analysis of iCNS relapse rate was performed using a cumulative incidence function.34 EFS and OS life table estimates were performed with the Kaplan-Meier (KM) method with 6 years of follow-up.35 EFS and OS comparisons began at the time of randomization when subjects achieved their first complete remission (CR1). Events include first relapse at any site(s), death in first remission, and second malignant neoplasm (SMN). Patients lost to follow-up were censored at the date of final contact. The standard deviation of the KM estimates was calculated using the Peto variance formula.36 RHRs were estimated by the log-rank method of observed divided by expected (O/E) events. χ2 tests for homogeneity of distributions were used in some comparisons, and multivariate analysis of prognostic factors was performed with the Cox proportional hazards model.37 In the present report, iCNS relapse, EFS, and OS are presented as percent ± standard error (SE).
Relapse definitions
Isolated CNS relapse occurred when CSF contained at least 5 WBCs per microliter with morphologically identifiable blasts on cytospin, BM aspirations showed normal trilineage hematopoeisis with fewer than 5% blasts, testes were normal to palpation, and no other extramedullary (EM) sites of disease were identified. BM relapse was defined as an M3 status after CR1 and, occasionally with approval of the study chair, as an M2 status with the diagnostic cytogenetic clone. Combined relapses included those with simultaneous recurrence in BM and an EM site.
Results
Patient and leukemia characteristics
A total of 2185 patients were entered onto study. Ten were found to be ineligible prior to randomization (5 due to misdiagnosis; 3 inadequate institutional review board approval or improper consent; 1 prolonged prednisone exposure; and 1 who was registered more than 72 hours after initiating treatment). A total of 113 patients were excluded from randomization because of induction death, M3 day 14 marrows, or unfavorable cytogenetics; 32 subjects refused further study participation. Among the 2030 randomized patients, 3 were deemed ineligible following randomization (1 improper consent; 1 day-14 marrow inappropriately omitted; 1 M3 day-14 marrow). Thus, 2027 eligible and randomized patients are included in the statistical comparisons of the randomized treatment regimens. A total of 1018 patients were randomized to receive IT MTX; 1009 were randomized to receive ITT.
The CCG Cytogenetics Committee reviewed 1857 institutional karyotypes and accepted 881 (43%) from the entire randomized study population. EFS and OS were equivalent for the subgroups with accepted and rejected karyotypes. A total of 121 cases (14%) were identified with trisomies of chromosomes 4, 10, and 17 (“triple trisomies” [TTs]). TEL/AML1 expression was successfully analyzed by the CCG ALL Reference Laboratory in 940 randomized patients; 189 (20%) cases expressed the TEL/AML1 fusion transcript. Among the 416 randomized patients with both accepted cytogenetics and TEL/AML1 analysis, 134 (32%) were identified with either TT or TEL/AML1 expression.
Among 1973 randomized subjects with complete data, the day 7/day 14 marrow results were as follows: 970 cases were M1/not evaluated, 478 were M2/M1, 346 were M3/M1, 47 were M2/M2, and 132 were M3/M2. A total of 91% of the randomized patients were M1 by day 14, and the rest were M2.
Presenting characteristics of patients and blast cytogenetics/molecular genetics were not significantly different between the 2 IT cohorts or among the 4 randomized regimens (P = .13 to .9; Table 3). However, a disparity occurred in the randomization of subjects with M3 day 7 BM status and M2 day 14 BM status. More patients received ITT than IT MTX in both of these slow response subgroups, as shown in Table 3.
Median follow-up from randomization is 6 years for patients alive in continuous remission. Eighty-two randomized patients are currently lost to follow-up, 40 on IT MTX and 42 on ITT.
Treatment outcome
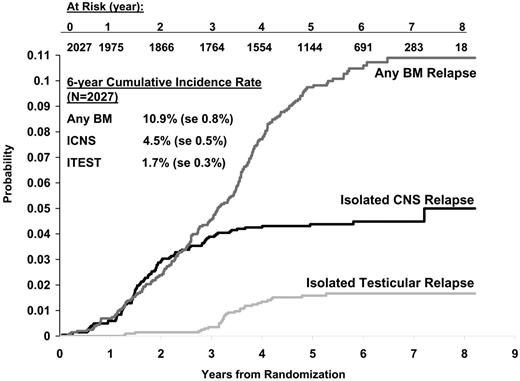
Overall outcome. For the 2027 eligible randomized patients, the 6-year estimated EFS is 81.6% ± 1.3% and OS is 92.3% ± 0.9%. The overall rate of iCNS relapse ± SE at 6 years is 4.9% ± 0. 8%, and the BM (includes BM and EM) relapse rate ± SE at 6 years is 7.7% ± 1.1%. Most iCNS relapses occurred within the first 3 years of diagnosis, as shown in Figure 2. In contrast, more than half of the BM relapses were diagnosed after that time period. Isolated testicular relapses typically presented following completion of therapy, and the 6-year life table estimate of isolated testicular relapse is 3.4% of the male cohort.
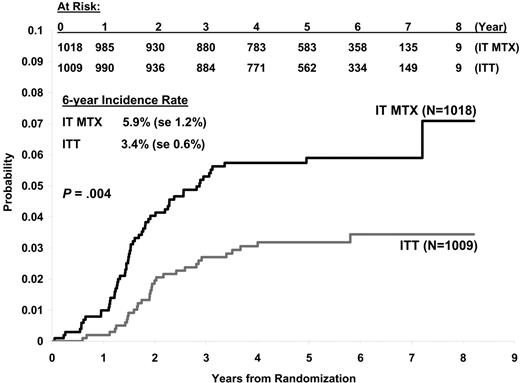
Comparison between IT regimens. The incidence of iCNS relapse is significantly lower among patients treated with ITT than with IT MTX (P = .004, RHR = 0.53), with 31 iCNS relapses on the former regimen and 58 on the latter. Cumulative incidence estimates of iCNS relapse at 6 years are 3.4% ± 1.0% for ITT and 5.9% ± 1.2% for IT MTX (Figure 3). Among the iCNS relapses, 40.4% developed “early” (within 18 months of CR1); 59.6% occurred “late.” Most of these relapses were identified in asymptomatic patients by CSF results obtained at the time of IT administration. More cases of iCNS relapse occurred “early” with IT MTX than ITT regimens: 46.6% versus 29%, respectively (P = .083, χ2).
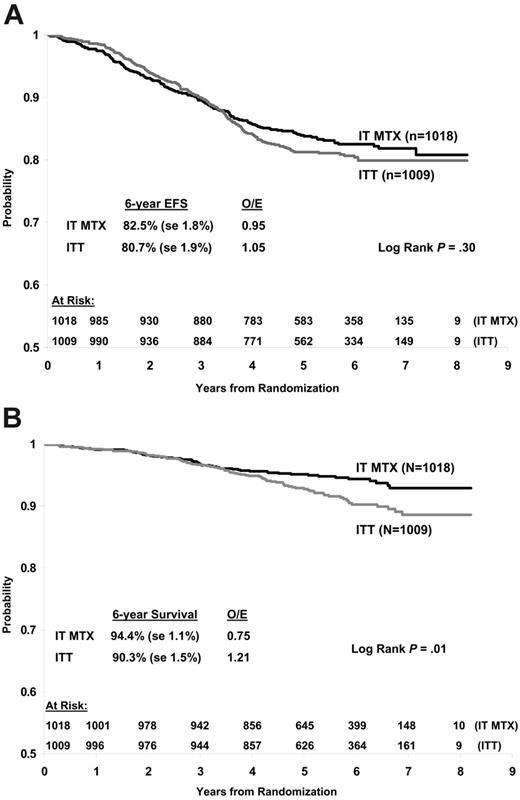
More BM relapses developed on the ITT than the IT MTX regimens: 117 (22 BM and CNS; 7 BM and other EM; 88 BM only) versus 79 (21 BM and CNS; 4 BM and other EM; 54 BM only). Moreover, almost twice as many non-CNS EM relapses (primarily testicular) occurred with ITT than with IT MTX (20 versus 11). Thus, more events have occurred among the 1009 patients randomized to ITT than in the 1018 randomized to IT MTX: 174 relapses and 186 total events (7 remission deaths and 5 SMNs) on ITT; 151 relapses and 168 total events (12 remission deaths and 4 SMNs) on IT MTX. The estimated 6-year EFSs of ITT and IT MTX are statistically equivalent at 80.7% ± 1.9% and 82.5% ± 1.8%, respectively (P = .3, log-rank; Figure 4A). Because more patients have died after BM than iCNS relapse, there is currently a 6-year overall survival (OS) advantage for patients on IT MTX compared with ITT: 94.4% ± 1.1% versus 90.3% ± 1.5% (P = .01, log-rank), with a relative death rate 1.5 times higher for ITT than IT MTX (Figure 4B).
Because the randomization resulted in a slight disparity in the percentages of patients on the ITT and IT MTX regimens with regard to marrow involvement status at day 7 and day 14 of induction, stratified log-rank tests were performed to adjust for the imbalance and compare those results with the general findings for the unadjusted comparison of ITT and IT MTX. Comparing OS for ITT versus IT MTX with adjustment for the day 7 and day 14 marrow ratings resulted in only slightly modified results from the unadjusted comparisons (day 7 marrow: adjusted P = .03, RHR = 0.68; day 14 marrow: adjusted P = .02, RHR = 0.67). Similarly, adjusted analyses for marrow relapse outcome still support a significant excess of marrow relapse occurring on the ITT regimen.
More marrow relapses occurred with ITT and more iCNS with IT MTX in each of the thiopurine strata. No evidence for statistical interactions between the IT and thiopurine regimens was found for EFS or OS by Cox regression; P = .54 and .25, respectively.
Outcome analyses among subsets. While variation in outcome for patient subsets could be due to simple statistical random variation, some of the results are worth noting. The incidence of iCNS relapse is not statistically different between patients with day 14 M2 BM on IT MTX or ITT; P = .12, log-rank. However, the 6-year estimated EFS is worse with ITT than IT MTX (58.9% ± 8.4% versus 75.4% ± 8.6%; P = .05, log-rank; RHR = 1.7) because of an excess in BM relapses on the former regimen (28 versus 8). Estimated 6-year OS is markedly worse with ITT than IT MTX in the M2 cohort: 76.7% ± 7.6% versus 97.4% ± 3.0%; P = .002; RHR = 5.3.
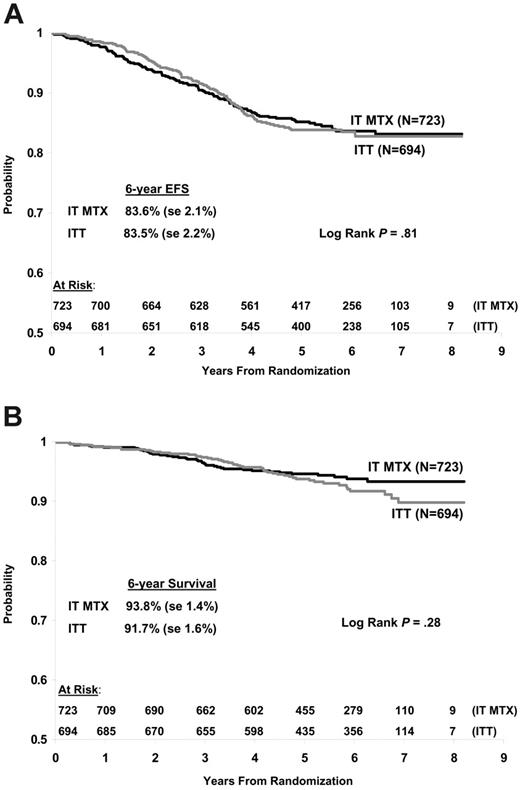
Figure 5 compares the EFS and OS between IT regimens for the currently defined COG SR-ALL precursor-B rapid early response (RER) subset (n = 1417), excluding higher-risk patients (T lineage, day 14 M2, CNS-3, or testicular disease). The iCNS relapse rate is 4.8% ± 1.3% among the 723 subjects on IT MTX and 3.3% ± 1.1% among 694 on ITT; RHR = 1.6; P = .09, log-rank. The estimated 6-year EFS is equivalent on both regimens, with 109 events and EFS of 83.6% ± 2.1% on IT MTX and 110 events and EFS of 83.5% ± 2.2% on ITT; P = .81, log-rank; RHR = 0.96. Moreover, the 6-year OS among the redefined SR-ALL subset is equivalent with IT MTX and ITT: 93.8% ± 1.4% and 91.7% ± 1.6%, respectively; RHR = 0.8; P = .28, log-rank.
Factors predictive of iCNS relapse
Among randomized patients, univariate analysis of presenting features found age (1 versus 2 to 5 or 6 to 9 years), sex, CNS status (CNS-1 versus CNS-2), immunophenotype (pre-B versus T), hepatomegaly, mediastinal enlargement, nodal enlargement, splenomegaly, and WBCs (less than 20 000 × 109/L versus 20 000 × 109/L or more) to have prognostic significance for iCNS relapse. In multivariate analysis, 4 variables retained statistical significance: sex, hepatomegaly, CNS status, and age at diagnosis (Table 4). Mediastinal mass had borderline significance; P = .08.
Survival of redefined SR-ALL subset. (A) EFS. (B) OS. See “Outcome analyses among subsets” for definitions.
Survival of redefined SR-ALL subset. (A) EFS. (B) OS. See “Outcome analyses among subsets” for definitions.
For cases with centrally approved cytogenetics, the presence of TTs had no impact on the incidence of iCNS relapse: 5.1% ± 3.7% versus 5.0% ± 1.4% for TT-positive and TT-negative patients, respectively; P = .97. Among those tested for TEL/AML1 expression, iCNS relapse rates at 6 years are lower within the TEL-positive than TEL-negative cohort: 2.8% ± 2.0% versus 6.7% ± 1.5%, respectively (RHR = 0.42; P = 06, log-rank).
The impact of the IT regimens on outcome within the CNS-2 cohort deserves mention. ITT reduces the 6-year cumulative incidence estimate of iCNS relapse to a significantly greater degree in the CNS-2 cohort (n = 113) than the CNS-1 cohort (n = 1827) when compared with IT MTX: The CNS-2 iCNS relapse rate was 7.7% ± 5.3% versus 23.0% ± 9.5%, respectively (RHR = 0.20; P = .004, log-rank), and the CNS-1 iCNS relapse rate was 3.1% ± 1.0% versus 5.1% ± 1.2%, respectively (RHR = 0.59; P = .03, log-rank). However, this reduction in iCNS relapse rate with ITT did not translate into a statistically significant EFS or OS advantage for the CNS-2 cohort. The 6-year EFS was 76% versus 66% and OS was 89% versus 92% for the ITT and IT MTX arms, respectively; P = .12 and .3.
Toxicity
CNS toxicity. According to toxicity coding on end-of-phase forms, grade 3-4 CNS toxicity occurred in 6.3% of randomized patients: 5.8% on IT MTX and 6.7% of those on ITT. The number of adverse events that occurred within each phase and IT regimen is shown in Table 5. Three patients experienced 2 episodes each.
The study chair was directly informed about 64 CNS toxicity events. These episodes included 23 seizures; 19 hemiplegias (with or without aphasia, dysarthria, ataxia, seizures); 9 severe ataxias (with or without slurred speech); 4 facial nerve palsies (with or without slurred speech); 3 Guillain-Barré–like weaknesses, and 6 “other” neurotoxicities. Forty-eight episodes occurred in DI no. 1 or no. 2 within 10 days after day 35 IT treatment or during weekly IT doses in consolidation. Most of these episodes resolved rapidly without residual deficits or recurrent seizures and without anticonvulsant therapy. Some patients had subsequent magnetic resonance imaging (MRI) that documented leukoencephalopathy. All patients survived the toxic event, although a few have residual impairments.
Among patients who experienced acute CNS toxicity, the subsequent dose of ITT or IT MTX was generally followed by oral leucovorin 10 mg 36 to 48 hours later. Thereafter, IT doses were given without leucovorin. IT cytarabine (with or without HSS) was rarely substituted for IT MTX or ITT during the remaining treatment. Ten patients received no further IT therapy after the adverse event.
Other toxicity. Aside from reversible venoocclusive disease (VOD) induced by TG,38 no unexpected toxicities occurred on this study. The frequencies of non-CNS grade 3-4 toxicities, including VOD, were equivalent on the 2 IT regimens. The mean number of inpatient days per patient were also similar with IT MTX and ITT: consolidation/IM no. 1: 3.2 versus 2.9; DI no. 1: 5.0 versus 5.2; IM no. 2: 1.1 versus 1.1; DI no. 2: 5.0 versus 5.6; and maintenance (each 84-day course): 0.99 versus 1.04, respectively.
Discussion
Isolated CNS relapse remains a major obstacle in the cure of childhood ALL and accounts for 30% to 40% of the initial relapses on recent CCG low-, standard-, and average-risk ALL trials.19,20,39 In the early 1970s, cXRT with limited IT MTX provided excellent protection against CNS relapse.2-4 However, surviving patients suffered considerable neurocognitive and endocrine impairments, and some developed brain tumors.40-44 Since that time, treatment approaches for ALL have attempted to prevent CNS disease by substituting extended IT regimens for cXRT. The Southwest Oncology Group first studied ITT in a randomized comparison with IT MTX and HSS for children with recurrent CNS disease; they found comparable efficacy.45 Of note, HSS was included in both regimens in an attempt to decrease arachnoiditis rather than to enhance disease control.2 Sullivan et al6 then demonstrated equivalent outcome with extended ITT compared with cXRT and limited IT MTX in patients with de novo ALL. Subsequently, some institutions and cooperative groups adopted ITT as “presymptomatic” IT,11,13 while others continued to give MTX alone.46,47
In this large multiinstitutional study, cumulative iCNS relapse is considerably less with ITT than IT MTX. However, this iCNS relapse advantage of ITT over IT MTX is offset by a significantly greater number of BM and testicular relapses on the ITT regimen. Although the 6-year EFS of the 2 regimens is statistically equivalent, the 6-year OS is significantly worse with ITT than IT MTX, because fewer patients are salvaged following a BM than an iCNS relapse. This paradoxic effect of ITT is different from that seen within the CCG-1922 SR-ALL experimental cohort, where dexamethasone was given throughout treatment and significantly reduced the incidence of both iCNS and BM relapse and improved long-term EFS.20 The addition of cytarabine and HSS to IT MTX is purely a CNS-directed intervention, because the former 2 drugs do not achieve appreciable plasma levels to exert a systemic effect.48-50 In contrast, dexamethasone reaches leukemic cells within the CNS, BM, and other EM sites.51 The 40 mg/m2 dose of prednisone used in the present study is the same as that used in CCG predecessor Berlin-Frankfurt-Muenster (BFM)–modified protocols for standard/low-risk ALL, most of which had very favorable results as compared with contemporary studies. It is not known whether the higher induction dose of 60 mg/m2 given to higher-risk CCG patients would have impacted iCNS relapse rate or outcome.19,20
The exchange of iCNS relapse for later BM or testicular relapse supports the concept that a CNS relapse does not, in fact, occur in “isolation.” Certain patients in CR1 are poised to relapse. This relapse may initially manifest in an EM site, in the BM, or both. CSF cytospins may be more sensitive indicators of relapse than BM aspirates, because blasts are morphologically detectable in CSF after more than 105 lymphoblasts fill the CSF compartment but not until more than 109 fill the marrow space.52 A purely CNS-directed intervention, like IT cytarabine added to IT MTX, appears to shift the site of relapse from CNS to BM or testes but does not ultimately prevent relapse. In the 1970s and 1980s, investigators debated whether BM recurrence following iCNS relapse reflects reseeding of BM from CSF or subclinical disease already present in BM at the time of iCNS relapse.53-55 Data from the present clinical trial support the latter concept. Studies identifying minimal residual disease (MRD) in BM concurrent with an iCNS relapse also support this model.56-58 Therefore, one possible detrimental effect of ITT could be a delay in detection of disease recurrence.
The currently defined COG SR-ALL precursor-B RER subset excludes patients with T lineage, day 14 M2, CNS-3, or testicular disease. Consequently, we compared outcome between IT MTX and ITT among subjects on CCG 1952 in this redefined cohort and found equivalent estimated 6-year EFS and OS. In contrast, a marked excess of BM relapses developed among the day 14 M2 cohort treated with ITT compared with IT MTX. Thus, ITT may have had an unfavorable effect on patients with M2 day 14 BM.59 Interestingly, an inferior EFS was also observed on POG 9005 for lower-risk B-lineage ALL when ITT was substituted for IT MTX part way through that study.60
The lower EFS with ITT in the day 14 M2 subgroup raises the possibility that ITT interferes with systemic chemotherapy. Systemic MTX exposure may, in fact, be greater after IT than oral administration.61 If either IT cytarabine or HSS interferes with egress of MTX from CSF into blood, the BM of patients on ITT may have been exposed to less systemic MTX than those on IT MTX. This theoretical effect of ITT could have been particularly harmful during 3 weekly IT treatments in the month of consolidation, when no weekly oral MTX is given. Arguing against this hypothesis, however, is the POG 9005 study, because systemic MTX was given with each ITT.60,62 Furthermore, patients treated by Sullivan et al with 5 weekly injections of ITT in induction developed significantly more myelosuppression than those who received no IT, suggesting that at least some MTX reached the BM after ITT administration.6 IT cytarabine is rapidly deaminated as it enters the systemic circulation and achieves no measurable plasma level.49 Therefore, it is unlikely that antagonism between cytarabine and MTX within the BM compartment contributes to the inferior EFS. 18,63 It remains unclear why EFS is worse in the M2 day 14 cohort given ITT on CCG 1952.
Potential factors predictive of iCNS relapse were analyzed on this study. Multivariate analysis found sex, hepatomegaly, CNS status, and age to have strong prognostic significance. Boys are 2.7 times more likely than girls to experience an iCNS relapse on this study despite an additional year of maintenance and 4 more IT injections. Previous studies also identified male sex as a risk factor for iCNS relapse.8,20,64,65 Interestingly, outcome was worse for boys than girls on St Jude's Total XIII and ALL-BFM 90 protocols, despite a very low iCNS relapse rate for both sexes.66-68 Splenomegaly, nodal enlargement, and hepatomegaly were each significant predictors of iCNS relapse in univariate analysis. Hepatomegaly retained marked prognostic significance in multivariate analysis. Thus, EM spread of ALL at diagnosis, even outside the CNS, correlates with future iCNS relapse.
Patients with CNS-2 status at diagnosis were 4 times more likely to relapse in CNS than their CNS-1 counterparts. Contrary to the recent practice of some cooperative groups, the CNS-2 cohort did not receive additional doses of IT chemotherapy during induction on this study.67,69,70 Interestingly, ITT reduced the iCNS relapse rate 5-fold compared with IT MTX in the CNS-2 subset. Excess BM relapses and poorer EFS did not occur in the CNS-2 cohort treated with ITT compared with IT MTX. For these patients and for those with traumatic spinal taps at diagnosis, intensifying CNS-directed therapy may minimize the risk of seeding marrow from the CNS.66
Some studies have found that patients whose initial spinal tap is traumatic with blasts (TLP+) have an increased risk of CNS relapse and adverse outcome, particularly among high-risk cohorts.71-73 In our study, the incidence of TLP+ was too low to analyze its effect on outcome. Similarly, the impact of either IT regimen on the outcome of patients with TLP+ could not be evaluated.
ITT prevented iCNS relapse but failed to improved EFS and worsened OS in this large SR-ALL cohort. ITT may improve outcome compared with IT MTX when combined with more intensive systemic treatment, like treatments designed for Burkitt lymphoma or T-cell ALL.74,75 ITT may offer an advantage to relapsed patients somewhat resistant to MTX.76 It may also benefit select SR-ALL subsets, like those with CNS-2 status at diagnosis.
Our data suggest that if IT MTX is used for IT presymptomatic CNS therapy, it should be combined with systemic therapy that would provide better CNS protection, such as higher doses of MTX, higher doses of prednisone, or dexamethasone as the sole corticosteroid therapy. If ITT is to be used for IT presymptomatic CNS therapy, it should be combined with more intensive systemic therapy than given in this study. Because iCNS relapse is largely a local manifestation of systemic failure, efforts to improve outcome in all risk categories of ALL require interventions directed simultaneously at marrow and EM sites. Successor COG studies for children with SR-ALL administer MTX alone for presymptomatic CNS therapy. Dexamethasone is used as the sole corticosteroid with the intention of providing superior systemic and CNS-directed therapy.
Appendix
Participants in the Children's Oncology Group Study 1952 are included as follows (wherever applicable, principal investigators are listed in parentheses): A. B. Chandler Medical Center–University of Kentucky, Lexington (Martha Greenwood); Albany Medical Center, NY (Jennifer Pearce); Allan Blair Cancer Centre, Regina, SK, Canada (Mansoor Haq); Atlantic Health System, Morristown, NJ (Hazem Mahmoud); Backus Children's Hospital at MHUMC, Savannah, GA (Tribhawan Vats); Baystate Medical Center, Springfield, MA (Philippa Sprinz); Bellin Memorial Hospital, Green Bay, WI; British Columbia's Children's Hospital, Vancouver, BC, Canada (Mason Bond); Brookdale Hospital Medical Center, Brooklyn, NY (Kusum Viswanathan); Brooklyn Hospital Center, NY (Swayamprabha Sadanandan); C. S. Mott Children's Hospital, Ann Arbor, MI (Raymond Hutchinson); CancerCare Manitoba, Winnipeg, MB, Canada (Rochelle Yanofsky); Cedars-Sinai Medical Center, Los Angeles, CA (Carole Hurvitz); Children's Healthcare of Atlanta at Scottish Rite, GA; Children's Healthcare of Atlanta, Emory University, GA (Howard Katzenstein); Children's Hem/Onc Team at Covenant Children's Hospital, Lubbock, TX (Melanie Oblender); Children's Hospital and Regional Medical Center, Seattle, WA (Douglas Hawkins); The Children's Hospital at The Cleveland Clinic, OH (Joanne Hilden); Children's Hospital Central California, Madera (Vonda Crouse); The Children's Hospital–Denver, CO (Kelly Maloney); Children's Hospital of Austin, TX (Sharon Lockhart); Children's Hospital of Pittsburgh, PA (A. Ritchey); Children's Hospitals and Clinics–St Paul, MN; Children's Medical Center Dayton, OH (Emmett Broxson); The Childrens Mercy Hospital, Kansas City, MO (Maxine Hetherington); Children's National Medical Center–DC, Washington (Max Coppes); Children's Hospital LosAngeles, CA(Paul Gaynon); Children's Hospital Medical Center–Akron, OH (Steven Kuerbitz); Children's Hospital Oakland, CA (James Feusner); Children's Hospital of Orange County, Orange, CA (Violet Shen); Children's Hospital of Philadelphia, PA (Richard Womer); Children's Hospital of Western Ontario, London, ON, Canada (A. Cairney); Children's Hospital–King's Daughters, Norfolk, VA (Rebecca Byrd); Children's Hospitals and Clinics of Minnesota, MN (Bruce Bostrom); Children's Memorial Hospital of Omaha, NE (Minnie Abromowitch); Christiana Care Health Services/A. I. duPont Institute, Wilmington, DE (Gregory Griffin); Cincinnati Children's Hospital Medical Center, OH (John Perentesis); City of Hope National Medical Center, Duarte, CA (Judith Sato); Clarian Health, Indianapolis, IN; Columbia Medical Center–West, El Paso, TX; Columbia Presbyterian College of Physicians and Surgeons, New York, NY (Linda Granowetter); Columbus Children's Hospital, OH (Amanda Termuhlen); Connecticut Children's Medical Center, Hartford (Arnold Altman); Cooper Hospital/University Medical Center Camden, NJ; Dakota Clinic, Fargo, ND; Dakota Midwest Cancer Institute, Sioux Falls, SD; Deaconess Medical Center, Spokane, WA; DeVos Children's Hospital, Grand Rapids, MI (David Freyer); Doernbecher Childrens Hospital–Oregon Health and Science University, Portland (Linda Stork); Duluth Clinic, MN; East Tennessee Childrens Hospital, Knoxville (Ray Pais); Geisinger Medical Center, Danville, PA (Jeffrey Taylor); Georgetown University Medical Center, Washington, DC (Aziza Shad); Group Health Cooperative, Seattle, WA; Gundersen Lutheran, La Crosse, WI; Henry Ford Hospital, Detroit, MI; Indiana University–Riley Childrens Hospital, Indianapolis (Robert Fallon); Izaak Walton Killam (IWK) Health Centre, Halifax, NS, Canada (Margaret Yhap); Janeway Child Health Center, St John's, NF, Canada (John [Jack] Hand); Kaiser Permanente Medical Group, Northern CA, Sacramento (Vincent Kiley); Kalamazoo Center for Medical Studies, MI (Leonard Mattano, Jr); Kosair Childrens Hospital, Louisville, KY (Salvatore Bertolone); Loma Linda University Medical Center, CA (Antranik Bedros); Loyola University Medical Center, Maywood, IL (Ricarchito Manera); Lutheran General Children's Medical Center, Park Ridge, IL (Jong-Hyo Kwon); M. D. Anderson Cancer Center, Houston, TX (Joann Ater); Maimonides Medical Center, Brooklyn, NY (Ludovico Guarini); Marshfield Clinic, WI (Michael McManus); Mary Bridge Hospital, Tacoma, WA (Ronald Louie); Mayo Clinic and Foundation, Rochester, MN (Carola Arndt); Medical College of Georgia Children's Medical Center, Augusta (Roger Vega); Mercy Children's Hospital, Toledo, OH (Rama Jasty); MeritCare Medical Group doing business as Roger Maris Cancer Center, Fargo, ND (Nathan Kobrinsky); Methodist Children's Hospital of South Texas, San Antonio (Donna Wall); MetroHealth Medical Center, Cleveland, OH; Michigan State University, East Lansing (Renuka Gera); Miller Children's Hospital/Harbor–University of California at Los Angeles (UCLA), Long Beach, (W. Roberts); Montefiore Medical Center, Bronx, NY (Adam Levy); Mountain States Tumor Institute, Boise, ID (J. Johnston); Nevada Cancer Research Foundation–CCOP, Las Vegas, NV (Jonathan Bernstein); New York Hospital–Cornell University Medical Center, New York, NY (Patricia Giardina); New York Medical College, Valhalla (Fevzi Ozkaynak); New York University Medical Center, NY (Elizabeth Raetz); Newark Beth Israel Medical Center, NJ (Peri Kamalakar); Penn State Children's Hospital, Hershey Medical Center (John Neely); Phoenix Children's Hospital, AZ (Jessica Boklan); Presbyterian/St Luke's Medical Center and CHOA, Denver, CO (Stephen Palmer); Primary Children's Medical Center, Salt Lake City, UT (Phillip Barnette); Princess Margaret Hospital for Children, Perth, WA,Australia (David Baker); Quain & Ramstad Clinic, Bismarck, ND; Rainbow Babies' and Children's Hospital, Cleveland, OH (Susan Wiersma); Raymond Blank Children's Hospital, Des Moines, IA (Torrey Mitchell); Saint Barnabas Medical Center, Livingston, NJ (Brenda Sison); Santa Barbara Cottage Children's Hospital, CA (Daniel Greenfield); Saskatoon Cancer Center, SK, Canada (Kaiser Ali); Schneider Children's Hospital, New Hyde Park, NY (Arlene Redner); Schneider Children's Hospital at North Shore, Manhasset, NY; Sinai Hospital of Baltimore, MD (Joseph Wiley); Sioux Valley Children's Specialty Clinics, Sioux Falls, SD (Linda Stout); South Carolina Cancer Center, Columbia (Ronnie Neuberg); Southern California Permanente Medical Group, Downey (Robert Cooper); Southern Illinois University School of Medicine, Springfield (Gregory Brandt); St Joseph's Hospital and Medical Center, Paterson, NJ (Mary Ann Bonilla); State University of New York Health Science Center at Brooklyn (Sreedhar Rao); Texas Tech UHSC–Amarillo (Curtis Turner); Tod Childrens Hospital–Forum Health, Youngstown, OH (Ayman Saleh); Toledo Children's Hospital, OH (Dagmar Stein); UCLA School of Medicine (Theodore Moore) University of California at San Francisco School of Medicine (Katherine Matthay); University of California, Irvine, Orange (Stanley Calderwood); The University of Chicago Comer Children's Hospital, IL (James Nachman); University of Illinois–Chicago (Mary Schmidt); University of Illinois–Rockford; University of Iowa Hospitals and Clinics, Iowa City (Raymond Tannous); University of Medicine and Dentistry of New Jersey, New Brunswick (Richard Drachtman); University of Minnesota Cancer Center, Minneapolis (Joseph Neglia); University of Nebraska Medical Center, Omaha (Peter Coccia); University of North Carolina at Chapel Hill (Stuart Gold); University of Wisconsin–Children's Hospital Madison (Yousif [Joe] Matloub); Vanderbilt Children's Hospital, Nashville, TN (James Whitlock); William Beaumont Hospital, Royal Oak, MI (Charles Main); Winthrop University Hospital, Mineola, NY (Mark Weinblatt).
Prepublished online as Blood First Edition Paper, April 11, 2006; DOI 10.1182/blood-2005-12-011809.
A complete list of the members of the Children's Oncology Group appears in “Appendix.”
Supported in part by the Children's Oncology Group Chairman's grants CA 98543 and CA 98413 from the National Cancer Institute, National Institutes of Health.
Y.M. participated in the running of the study and wrote the manuscript; S.L. analyzed data and presented an abstract at the 44th annual meeting of the American Society of Hematology; P.S.G. designed the study and headed the CCG ALL Committee; H.S. designed study statistics and analyzed data; M.L. and N.A.H. analyzed data; E.B. participated in the running of the study and edited the manuscript; R.Y. participated in the running of the study; R.H. participated in the study as vice chair; J.N. edited the manuscript; M.B., L.M.W., A.D.S., M.M., and J.F.K. participated in the running of the study; and L.C.S. designed the study as study chair and participated in the writing of the manuscript.
Presented in abstract form at the 44th annual meeting of the American Society of Hematology, December 9, 2002.77
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 U.S.C. section 1734.
We thank Dr Archie Bleyer as CCG chair, Dr Gregory Reaman as COG chair, Dr William Carroll as chair of the COG ALL Committee, CCG/COG staff and investigators, institutional clinical research associates, and all the patients and families who participated in the study.