Meningeal involvement in patients with AIDS-related non-Hodgkin lymphoma (ARL) is common; it confers a dismal prognosis, and therapy usually involves frequent lumbar punctures. In 137 individuals with ARL in the era of highly active antiretroviral therapy (HAART), 22 had meningeal involvement at presentation. We compared the use of standard alternating intrathecal methotrexate and cytarabine with a sustained-release formulation of intrathecal cytarabine (DepoCyt) that maintains concentrations in the cerebrospinal fluid (CSF). There were no significant changes in overall survival, the rate of fall of CSF protein, and remission rates defined as absence of lymphomatous cells in the CSF and a CSF protein level less than 0.4 mg/L. DepoCyt appears safe and effective in patients with ARL and meningeal disease and reduces the number of intrathecal administrations required.
Despite the progress that has been made in controlling cancer at most sites in the body, the outcome of individuals affected by meningeal infiltration by cancer remains poor. As few patients with this condition survive for more than several months, the management of individuals with meningeal disease remains a great challenge.1-3 The direct intrathecal instillation of anticancer drugs is one approach that has successfully been used by oncologists, particularly in the treatment and prevention of leptomeningeal leukemias and lymphomas, to circumvent the pharmacologic sanctuary resulting from the blood-brain barrier. Only methotrexate and cytarabine (cytosine arabinoside [Ara-C]) are routinely administered intrathecally, and both are specific to the cell cycle's S phase. Therefore, both agents would appear most effective when cytotoxic concentrations are maintained. Achieving this has necessitated prolonged and frequent course of lumbar punctures, which are both painful and labor intensive.
An encapsulated microvesicular liposome preparation named DepoCyt (Sykepharma, London, United Kingdom) drastically changes the pharmacokinetics of the free cytarabine released4,5 such that the mean elimination t1/2 of the depot formulation of free cytarabine is 130 to 277 hours, versus 3.4 hours for native cytarabine.6-8 In 2 randomized clinical trials by Glantz et al that have recruited a total of 89 patients,9,10 DepoCyt produced a high response rate, comparable with either methotrexate or free cytarabine, and delayed neurologic progression. The DepoCyt regimen also produced a higher clearance rate of lymphoma from the CSF and prolonged time to neurologic progression compared with conventional intrathecal chemotherapy in a randomized controlled trial.11
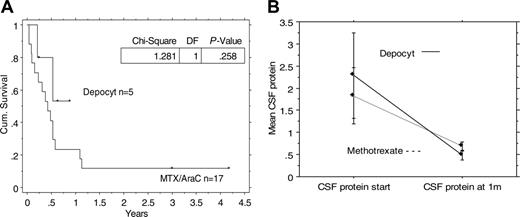
Survival and change in CSF protein with DepoCyt versus standard alternating methotrexate and cytarabine. (A) A Kaplan-Meier curve demonstrating the overall survival of individuals with ARL and meningeal disease, treated with either DepoCyt or alternating intrathecal installations of methotrexate and cytarabine. (B) A comparison of the rate of fall of CSF protein from the first intrathecal installation to 1 month. The median with the standard error of the mean is shown.
Survival and change in CSF protein with DepoCyt versus standard alternating methotrexate and cytarabine. (A) A Kaplan-Meier curve demonstrating the overall survival of individuals with ARL and meningeal disease, treated with either DepoCyt or alternating intrathecal installations of methotrexate and cytarabine. (B) A comparison of the rate of fall of CSF protein from the first intrathecal installation to 1 month. The median with the standard error of the mean is shown.
DepoCyt has not been evaluated in HIV-1-seropositive individuals. Because patients with ARL have frequent meningeal involvement (a situation complicated by frequent poor compliance in this vulnerable patient group12,13 ), we compared the efficacy of DepoCyt with that of alternating intrathecal methotrexate and cytarabine.
Since 1996, the start of the HAART era, 137 individuals at The Chelsea and Westminster Hospital have been diagnosed with biopsy-confirmed ARL, including 22 (16%) with meningeal involvement at presentation; these comprised 0.4% of all HIV-1-seropositive individuals with whom follow up was conducted during this time. Meningeal involvement was defined as abnormal enhancement on a brain computerized tomography or magnetic resonance scan and/or the presence of lymphoma cells in the CSF.
In addition to their systemic chemotherapy, they received intrathecal chemotherapy. Up until 2004, this comprised alternating intrathecal methotrexate (12.5 mg) and intrathecal cytarabine (50 mg), given twice a week for 4 weeks, then once a week for 4 weeks, then once a fortnight for 8 weeks, and then monthly until systemic chemotherapy was completed, approximately 18 intrathecal procedures in total.14 Since that time, DepoCyt, a slow-release formulation of cytarabine, has been used alone, comprising a 50-mg intrathecal injection alone every 2 weeks for 2 months followed by monthly injections for 6 months, for a total of 10 intrathecal installations. Each DepoCyt injection was accompanied by 4 mg dexamethasone given orally or intravenously twice a day for 5 days.
There were no significant differences in overall survival between individuals who received either intrathecal alternating methotrexate and cytarabine, or intrathecal DepoCyt (Figure 1A; log-rank, P = .26). Table 1 demonstrates the characteristics of 17 HIV-1-infected individuals with meningeal involvement at ARL presentation who received alternating intrathecal methotrexate and cytarabine compared with 5 patients who received DepoCyt since 2004. There were no differences that approached significance at baseline between the 2 groups, including no difference in the initial CSF protein (Mann-Whitney U test, P = .42) or in the rate of fall in CSF protein during the first month of therapy (Mann-Whitney U test, P = .55), or thereafter (Figure 1B). Ten (45%) individuals of the 22 achieved a CSF remission, as defined by the absence of lymphomatous cells in the CSF and CSF protein levels of less than 0.4 mg/L. These comprised seven (41%) of 17 on intrathecal methotrexate and cytarabine and 3 (60%) of 5 on DepoCyt (Mann-Whitney U test, P = .46). Out of these 10 individuals who achieved a CSF remission, 6 relapsed with CSF disease; all these patients died. CSF relapse occurred a median of 4 months after diagnosis (range, 0.7 to 5.8 months), and no late relapses have been observed. Thus, the 2-year survival for patients who achieved a CSF remission is 34% (95% confidence interval, 2%-66%).
Overall, DepoCyt is safe and effective in HIV-1-positive individuals with lymphomatous meningeal infiltration and has significant obvious advantages in its frequency of administration (18 vs 10 installations). It offers a significant alternative to the limited armamentarium of intrathecal agents in a group of individuals with well-documented issues with compliance18 and adherence.13,19
The leptomeninges and CSF pose a specific cytokinetic problem for oncologists because CSF concentrations of drugs need to be higher than any plasma-based administration can achieve (in either the plasma or CSF), and malignant cells within the CSF tend to proliferate slowly.2,20,21 The repeated intra-CSF administrations necessary to accomplish this obviously pose difficulties and Ommaya reservoirs have been implanted to permit repeated intra-CSF installations.22 This in turn requires anesthesia and surgery, though their use has not been reported in the setting of ARL.
Standard treatment for meningeal disease is time consuming, painful, labor intensive, and the subject of much adverse media and journal coverage when errors occur.23,24 As the prognosis of patients with meningeal disease has not changed for 3 decades,2 any therapy that reduces pain, time, and labor for both patients and treating physicians without a deleterious effect on outcome should be considered as standard therapy. As improved systemic therapy has ironically resulted in greater numbers of patients with leptomeningeal disease, DepoCyt should also be considered in a trial of CNS prophylaxis in patients with ARL and others at high risk of meningeal relapse.
J.S. and D.M. contributed equally to this letter.
All authors contributed substantially to manuscript writing, data collection and interpretation, and study design and methodology, and approved the final manuscript.