Abstract
This open-label, dose-escalation study evaluated the safety and efficacy of single-agent gemtuzumab ozogamicin, a humanized anti-CD33 antibody–targeted chemotherapeutic agent, for pediatric patients with multiple relapsed or primary refractory acute myeloid leukemia (AML). Twenty-nine children 1 to 16 years of age (relapsed disease, 19; refractory disease, 10) received gemtuzumab ozogamicin ranging from 6 to 9 mg/m2 per dose for 2 doses (separated by 2 weeks) infused over 2 hours. All patients had anticipated myelosuppression. Other toxicities included grade 3/4 hyperbilirubinemia (7%) and elevated hepatic transaminase levels (21%); the incidence of grade 3/4 mucositis (3%) or sepsis (24%) was relatively low. One patient treated at 9 mg/m2 developed veno-occlusive disease (VOD) of the liver and defined the dose-limiting toxicity. Thirteen patients underwent hematopoietic stem-cell transplantation less than 3.5 months after the last dose of gemtuzumab ozogamicin; 6 (40%) developed VOD. Eight of 29 (28%) patients achieved overall remission. Remissions were comparable in patients with refractory (30%) and relapsed (26%) disease. Mean multidrug resistance-protein–mediated drug efflux was significantly lower in the leukemic blasts of patients achieving remission (P < .005). Gemtuzumab ozogamicin was relatively well tolerated at 6 mg/m2 for 2 doses and was equally effective in patients with refractory and relapsed disease. Further studies in combination with standard induction therapy for childhood AML are warranted.
Introduction
Acute myeloid leukemia (AML) is generally considered to be a disease of older adults. The annual incidence of AML in people older than 65 years of age exceeds 10 per 100 000, making it the second most common form of leukemia in this population. However, AML is also diagnosed in a substantial number of children and adolescents. The estimated incidence of AML in children up to 4 years of age is 0.9 per 100 000, and for persons 15 to 19 years of age, it is 0.8 per 100 000.1,2
With currently used induction regimens, more than 80% of children with AML achieve remission.3-6 Dose intensification by time compression or increased exposure during induction chemotherapy has improved survival.3,4 However, only approximately 50% of all children with newly diagnosed AML will be cured with currently available treatment.7 Although several randomized studies have demonstrated that allogeneic hematopoietic stem-cell transplantation (HSCT) from a human leukocyte-antigen–matched family donor can improve survival in children with AML in first remission compared with chemotherapy alone or autologous HSCT, some centers prefer to perform allogeneic HSCT in second remission for some favorable subgroups.8 Thus, the goal of chemotherapy for patients with relapsed AML is to achieve remission for patients to undergo subsequent HSCT.
Gemtuzumab ozogamicin (Mylotarg CMA-676; Wyeth Pharmaceuticals, Philadelphia, PA) is a humanized monoclonal antibody directed against the CD33 surface antigen that is conjugated to a derivative of the cytotoxic antibiotic calicheamicin.9 Approximately 90% of patients with AML have myeloid blast cells that express significant levels of CD33.10 On binding, the antibody-antigen complex is internalized into target cells, and the calicheamicin molecule is released through hydrolysis. Calicheamicin binds to the minor groove of cellular DNA and causes double-strand breaks that lead to apoptosis.11
Gemtuzumab ozogamicin is approved by the US Food and Drug Administration (FDA) for the treatment of patients 60 years of age or older with CD33+ AML in first relapse who are ineligible for other cytotoxic chemotherapy.12,13 Response rates of approximately 25% have been observed in adult patients with refractory AML treated with gemtuzumab ozogamicin.14-16 The most clinically important toxicities associated with this drug have been abnormalities in hepatic function.15,16 Only limited data exist regarding the use of gemtuzumab ozogamicin for the treatment of refractory or relapsed AML in children.17-20 This phase-1 clinical trial was undertaken to evaluate the efficacy and tolerability of gemtuzumab ozogamicin as monotherapy in children younger than 18 years of age with relapsed or refractory CD33+ AML.
Patients, materials, and methods
Patients
Twenty-nine children with CD33+ AML who did not respond to primary induction therapy (n = 10) or who experienced relapse (n = 19) participated in this prospective, open-label, dose-escalation study conducted at 7 clinical research centers in the United States from 1999 to 2002 to evaluate the efficacy and safety of gemtuzumab ozogamicin as monotherapy. Children were considered to have CD33+ AML if they had more than 80% of leukemic blast cells with CD33+ immunofluorescence staining 4 times above background staining. Other enrollment criteria included a Lansky play index or a Karnofsky performance status of 60% or greater, normal renal and liver function, and a peripheral white blood cell (WBC) count of less than 30 000/μL. Patients who acquired AML secondary to chemotherapy or exposure to toxins were ineligible for enrollment. Patients with known central nervous system leukemia or testicular involvement with leukemia or patients who had undergone previous HSCT were also ineligible. Concomitant chemotherapy was prohibited.
The legal guardians of all patients provided signed informed consent, which was often also obtained from the patient. The study was approved and monitored by the institutional review board at each center and was performed in a manner consistent with the tenets of the Declaration of Helsinki and with Good Clinical Practice guidelines.
Gemtuzumab ozogamicin dosage
Determining the maximum tolerated dose (MTD) of gemtuzumab ozogamicin in pediatric patients was a primary objective of the study. Based on results obtained in the phase-2 trials using 9 mg/m2 as a 2-hour intravenous infusion conducted in 142 adults with AML in first untreated relapse,15 the first pediatric patient cohort received gemtuzumab ozogamicin monotherapy starting with a dose of 6 mg/m2 (0.2 mg/kg for patients younger than 3 years of age) for 2 doses with a 14-day interval between doses. Dose-limiting toxicity (DLT) was defined as National Cancer Institute (NCI) grade 3 gemtuzumab ozogamicin–related nonhematologic toxicity. Exceptions were grade 3 infections, bleeding, nausea, vomiting, febrile neutropenia, or infusion-related adverse events that resolved within 24 hours or elevations in hepatic enzyme and bilirubin levels that were transient and reversible within 28 days of last dose. If DLT did not develop in 3 patients, the next 3-patient cohort was escalated to 9 mg/m2 (0.3 mg/kg for children younger than 3) for 2 doses, 14 days apart. The final escalation planned was 12 mg/m2 (0.4 mg/kg for children younger than 3). Toxicity was assessed after each infusion at all dose levels. In the event that 3 or more patients experienced a grade 3 or 1 patient experienced a grade 4 nonhematologic event or that any patient experienced veno-occlusive disease (VOD), de-escalation to the MTD was allowed. The goal was to have 10 to 15 patients treated at the MTD, defined as the dose level just below the level at which DLT occurs.
Before receiving gemtuzumab ozogamicin, patients were required to have peripheral WBC counts of less than 30 000/μL; hydroxyurea treatment was allowed to reduce peripheral WBC counts to that level. Patients were routinely premedicated with acetaminophen (15 mg/kg intravenously or orally) and diphenhydramine (1 mg/kg) approximately 1 hour before gemtuzumab ozogamicin infusion. Two additional doses of acetaminophen were permitted, one at approximately 4 hours and the other at approximately 8 hours after the initial pretreatment dose. Steroids were not used as prophylactic medication before gemtuzumab ozogamicin administration. Patients were eligible to receive the second dose of gemtuzumab ozogamicin if they had recovered from reversible nonhematologic toxicities resulting from the previous dose and had no evidence of uncontrolled infection, disease progression, or detectable formation of antibodies reactive with the drug.
The outcome of gemtuzumab ozogamicin therapy was evaluated for the treatment period, defined as the time from administration of the drug until 28 days after the completion of therapy. After recovery from treatment with gemtuzumab ozogamicin, patients received additional therapy thought most appropriate by their treating physician.
Safety assessments
Adverse events. The primary safety assessment was monitoring of adverse events, defined as treatment-emergent or infusion-related adverse events or any clinically significant abnormal laboratory finding. All patients who received at least one dose of study drug were included in the safety analysis. Safety was monitored continually during study drug administration and immediate follow-up and then monthly for approximately 6 months. Treatment-emergent adverse events were events not present at baseline or events present at baseline that worsened during treatment. The severity of adverse events was evaluated using the NCI Common Toxicity Criteria version 1. Events with a severity of grade 1 or 2 were considered mild or moderate and manageable. Grade 3 or 4 events were considered severe or life threatening. The presence and severity of VOD was determined according to the criteria established by McDonald et al.21
Analysis for antibodies directed against components of gemtuzumab ozogamicin. Gemtuzumab ozogamicin contains 3 components: humanized monoclonal antibody hP67.6 against the CD33 antigen, a derivative of calicheamicin, and a linker connecting the antibody and the calicheamicin derivative. Patients were screened for the production of antibodies directed against any of these components. Details regarding the methodology of enzyme-linked immunosorbent assays in gemtuzumab ozogamicin antibody analyses have been described elsewhere.15
Efficacy assessments
The primary efficacy end point in this study was the rate of complete remission (CR). Patients were assessed monthly for remission status. A patient had to meet the following criteria to be classified as having achieved CR: leukemic blasts absent from peripheral blood; percentage of blasts in the bone marrow 5% or less, as measured by morphologic studies, either bone marrow aspirate or biopsy; peripheral blood counts with hemoglobin level 9 g/dL or greater, absolute neutrophil count 1500/μL or greater, and platelet count 100 000/μL or greater; and red blood cell transfusion independence for 2 weeks and platelet transfusion independence for at least 1 week.
In adult phase-2 trials with gemtuzumab ozogamicin, a portion of patients met all the criteria for CR with the exception of full recovery of platelet counts (CRp) before additional therapy was received. CRp is defined in the same way as CR except that the platelet count is not specified, though platelet transfusion independence for at least 1 week is required. The rate of CRp was included as a secondary efficacy end point. The overall remission rate was the sum of the CR and the CRp rates.
Patients were considered to have achieved no remission (NR) if they did not meet all the criteria for CR or CRp. The NR category included patients who had leukemic blasts in the peripheral blood or whose percentage of blasts in the bone marrow was more than 5%. Patients with NR also included those who met the bone marrow criteria for remission but did not meet the criteria for peripheral count recovery or were not transfusion independent.
Drug efflux studies
Analysis of drug efflux based on adenosine triphosphate (ATP)–dependent multidrug resistance (MDR) transport proteins was determined using the fluorescent dye DiOC2 as a surrogate substrate, as previously described.22 Multiparameter flow cytometry was used to assess the residual DiOC2 in cells treated with or without cyclosporin A (CSA; Novartis Pharmaceuticals, East Hanover, NJ). CSA was used at concentrations that inhibit MDR protein–mediated dye efflux. Efflux ratios in the presence or absence of CSA were then calculated as the ratio of loading fluorescence intensity and fluorescence intensity after incubation. Statistical significance was calculated using the Wilcoxon rank sum test for the difference between the mean efflux ratios of responders and nonresponders. Previous analysis of MDR and response to gemtuzumab ozogamicin therapy in adult patients indicated that the median dye-efflux ratio in patients failing to achieve CR or CRp was significantly greater than the median value (of 1.2) observed in patients achieving CR or CRp.22 In the present study, the significance of a 1.2 cutoff value for efflux ratio was assessed with the Fisher exact test.
Results
Patient characteristics
Twenty-nine children who had AML refractory to initial induction therapy or who were in untreated first relapse were enrolled in this phase-1 study. The median age of the patients was 12 years (range, 1-16 years). Fifteen (52%) patients were boys, and 23 (79%) patients were white. Of the patients who were entered in the protocol and treated, 10 (35%) had been refractory to previous therapy, and 19 (66%) experienced relapse after a previous remission. Median first remission before relapse was 144 days (4.7 months; range, 1.1-27.8 months). At study entry, most (26 of 29) patients had 20% blasts, as determined by histopathology or flow cytometry. Three patients with blasts between 13% and 19% were also enrolled.
Dosing
All 29 patients received a first dose of gemtuzumab ozogamicin (14 at 6 mg/m2, 2 at 7.5 mg/m2, 13 at 9 mg/m2), and 23 patients were administered a second dose (12 at 6 mg/m2, 1 at 7.5 mg/m2, and 10 at 9 mg/m2). Six patients did not receive a second dose of gemtuzumab ozogamicin because of refractory leukemia (n = 2), adverse event (n = 1), death from disease progression 7 days after first gemtuzumab ozogamicin dose (n = 1), fever, neutropenia, and disease progression (n = 1), or infusion-related nausea and vomiting (n = 1). The second dose was administered a median of 14 days after the first dose (range, 14-26 days; mean, 16 days).
Initially, a single patient received 1 dose and 6 patients received 2 doses of drug at 6 mg/m2 each. Because no DLT was observed, the dose was escalated to 9 mg/m2 for 2 doses (n = 13). Three patients had grade 3/4 elevations of aspartate aminotransferase/alanine aminotransferase (AST/ALT). One patient was treated at this dose and developed VOD; therefore, the dose in the next 7 patients was de-escalated to 6 mg/m2, again without DLT. Subsequently, the dose in 2 patients was escalated to 7.5 mg/m2, without DLT, before the study closed.
Safety results
Infusions were associated with low-grade chills (55%), vomiting (41%), fever (35%), nausea (28%), tachycardia (14%), headache (10%), body pain (10%), sweating (7%), hypotension (7%), neck pain (7%), and hypertension (7%). Eight patients developed 12 episodes of infusion-related grade 3 or 4 adverse events (Table 1). These were generally of short duration and tolerable. There were no instances of anaphylaxis, anaphylactoid reactions, or delayed hypotension.
Almost all patients had transient and reversible elevations in liver function test results (AST, ALT, and total bilirubin). Grade 3 or 4 elevations were observed in 8 (28%) patients (Table 1). The most common grade 3 or 4 treatment-emergent adverse events were leukopenia (48%), thrombocytopenia (35%), sepsis (24%), fever (24%), hypokalemia (21%), hypochromic anemia (17%), pleural effusion (17%), and pneumonia (17%).
Veno-occlusive disease was assessed separately according to the criteria of McDonald et al21 and occurred in 7 patients. One patient received the first dose of gemtuzumab ozogamicin and 3 days later developed signs and symptoms of VOD that resolved in 13 days. This patient subsequently underwent allogeneic HSCT without VOD. Fifteen patients underwent HSCT after gemtuzumab ozogamicin, with 6 patients developing moderate to severe VOD (Tables 2, 3). Mean time from the first dose was 102 days, and 12 of the 15 patients had a second dose a mean of 98 days (range, 35-410 days) before HSCT. Median time between the first and second doses was 14 days (range, 14-32 days). Patients who developed VOD after HSCT underwent transplantation fewer than 107 days (3.5 months) from the last dose of gemtuzumab ozogamicin (Tables 2, 3). Only 1 (3%) of 29 patients developed VOD without having undergone HSCT. VOD occurred 3 days after the first dose of gemtuzumab ozogamicin. The patient did not receive a second dose of gemtuzumab ozogamicin and died approximately 9 months later of refractory leukemia.
Deaths after gemtuzumab ozogamicin treatment. Causes of death in this study are listed in Table 4. Most patients died of progressive disease. Three patients died within 28 days of the last dose of gemtuzumab ozogamicin. All were reported to have disease refractory to gemtuzumab ozogamicin and died of progressive disease. All other patients died more than 28 days after the last dose of gemtuzumab ozogamicin (n = 24) or are still living (n = 2; one patient with CR and one with CRp are alive and in remission at 645+ and 112+ days, respectively).
Survival characteristics of patients treated with gemtuzumab ozogamicin. Survival of patients with initially refractory and relapsed AML was typically short. Those patients who underwent HSCT had the longest survival. However, HSCT was also associated with toxicity and early death in some patients (Table 4).
Immunogenicity of gemtuzumab ozogamicin in treated patients. None of the patients developed detectable antibody responses against the hP67.6 monoclonal antibody, calicheamicin, or the linker on day 8 or day 22 after each dose.
Efficacy results
Four patients experienced CR, and 4 experienced CRp, for 8 (28%) overall remissions after gemtuzumab ozogamicin therapy (Table 4). Of the 8 remissions, 5 (26%) were from the initial relapse group, and 3 (30%) were from the initial refractory group.
Drug efflux results
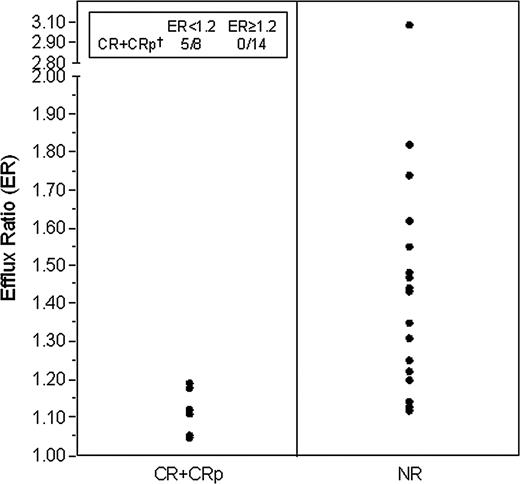
Previous studies have demonstrated that the MDR phenotype, defined as the ability of leukemic cells to show increased efflux of multiple drug types in association with elevated expression of ATP-dependent drug transporters (such as P-glycoprotein and MDR-related proteins), correlates with resistance to gemtuzumab ozogamicin.22 In these studies, a median dye-efflux ratio of more than 1.2 was observed in patients who did not achieve CR or CRp. To assess the applicability of this observation from patient samples in our phase-1 trial, we determined the relative level of drug efflux with and without the inhibitor of MDR-mediated efflux, CSA. Data available from the samples of 22 patients indicated a significant difference in the mean efflux ratio of responders compared with nonresponders (P = .005; Wilcoxon rank sum test). The groups also appeared to be separable by using an efflux ratio cutoff value of 1.2. Five of 8 patients with an efflux ratio less than 1.2 achieved CR or CRp, whereas none of the 14 patients with a ratio of 1.2 or greater achieved remission (P = .002, Fisher exact test) (Figure 1).
Discussion
Limited data have been published on the use of gemtuzumab ozogamicin for the treatment of AML in younger patients. Because children were not enrolled in the pivotal phase-2 clinical trials of gemtuzumab ozogamicin that led to its marketing approval in the United States,14 this dose-escalating study was conducted to evaluate the efficacy and safety of gemtuzumab ozogamicin in patients younger than 18 years of age with refractory and relapsed AML.17
Dose-limiting toxicity was not seen at a dose of 6 mg/m2. Although some reversible hepatic transaminase and bilirubin elevations occurred, these were not dose limiting. At the 9-mg/m2 dose, one patient developed VOD considered related to gemtuzumab ozogamicin and, thus, a DLT. The MTD was determined to be 6 mg/m2; however, 2 patients tolerated the 7.5-mg/m2 dose, and one achieved CRp. Before more patients could be escalated to this dose, the FDA approved gemtuzumab ozogamicin, additional enrollment was halted, and the study was closed. Of interest, responses were observed in all dose categories. The MTD of gemtuzumab ozogamicin for adults is 9 mg/m2. Given that the pharmacokinetic data for adults are comparable to those for children for this drug,20 it is possible that the MTD could be higher than 6 mg/m2 for children.
Level of drug efflux and response to single-agent gemtuzumab ozogamicin in pediatric patients with AML. This figure demonstrates the response (defined as CR or CRp) for patients whose leukemic blasts showed an efflux ratio less than 1.2 compared with a ratio of 1.2 or greater (P = .005). The ratio of drug efflux is defined in “Patients, materials, and methods.”
Level of drug efflux and response to single-agent gemtuzumab ozogamicin in pediatric patients with AML. This figure demonstrates the response (defined as CR or CRp) for patients whose leukemic blasts showed an efflux ratio less than 1.2 compared with a ratio of 1.2 or greater (P = .005). The ratio of drug efflux is defined in “Patients, materials, and methods.”
The safety and tolerability profile of gemtuzumab ozogamicin presented here appears to be similar to that described for adults.15,16 Most of the deaths that occurred during this pediatric study were attributable to disease progression or to complications associated with HSCT. Gemtuzumab ozogamicin was generally well tolerated by younger patients. Grade 3 or 4 infusion-related adverse events and grade 3 or 4 elevations in liver function tests were each reported in 8 patients. In previous studies of gemtuzumab ozogamicin, hyperbilirubinemia and elevated hepatic transaminase levels also were common nonhematologic adverse events.15,16
The overall incidence of VOD in the current study was 24% (n = 7). In the analysis of 277 adult patients with AML in first relapse from 3 pivotal phase-2 trials of gemtuzumab ozogamicin,23 the rate of VOD when the drug was administered without previous or subsequent HSCT was less than 1%. The incidence of VOD increased to 17% when gemtuzumab ozogamicin was given before or after HSCT.24 It is important to note that VOD developed in 6 of 7 patients in the study after they underwent HSCT.
Depending on previous therapy and on the conditioning regimen received, VOD develops in approximately 15% of patients after transplantation. Two studies have suggested an elevated risk for VOD among patients undergoing transplantation within a short time interval after gemtuzumab ozogamicin exposure.24,25 In the present study, all 6 children in whom VOD developed after transplantation had been exposed to gemtuzumab ozogamicin within 3.5 to 4 months of transplantation. Neither of the 2 patients who underwent transplantation more than 4 months from gemtuzumab ozogamicin exposure developed VOD. These findings are consistent with those of Erba et al24 and Wadleigh et al.25 When taken together with the data from the present trial, these studies suggest that the time from treatment with gemtuzumab ozogamicin to transplantation for relapsed or refractory AML appears to be important with respect to the development of posttransplantation VOD, regardless of patient age. Although the current study was not designed to assess the relationship between gemtuzumab ozogamicin administration, time to HSCT, and VOD, these results suggest such a relationship. At the doses used in this phase-1 trial, gemtuzumab ozogamicin as a single agent may increase the risk for VOD when bone marrow transplantation occurs less than 3.5 months from the time of the last dose of the antibody conjugate. However, the data presented in this report are not necessarily relevant to patients with relapsed or newly diagnosed AML who receive gemtuzumab ozogamicin at lower doses in combination with chemotherapy, such as is being tested in several ongoing studies.
More than one third (35%) of the patients in this study entered the trial with AML that was refractory to primary therapy, and the median duration of first CR for the remaining patients was only 4.7 months. Yet, the response of these patients was 28% overall. Importantly, patients with refractory disease responded as well as patients in first relapse (30% and 26%, respectively), suggesting that gemtuzumab ozogamicin has comparable efficacy in these 2 high-risk but distinct patient populations.
The analysis of drug efflux phenotype and the response to gemtuzumab ozogamicin is a possible surrogate marker of response, with no remissions observed in patients whose leukemic blasts showed relatively elevated levels of drug efflux. These data are consistent with those of a previous report correlating clinical response to gemtuzumab ozogamicin with low drug efflux blast phenotype.22 The data we present in our study extend these observations to pediatric patients within this clinical trial. Additional studies are warranted to determine whether the phenotype of low compared with high levels of drug efflux helps to define a priori which patients are more or less likely to respond to gemtuzumab ozogamicin. Similar studies with combinations of chemotherapy plus gemtuzumab ozogamicin should be particularly interesting to examine using drug efflux as a predictive surrogate of response. It will also be important to assess whether gemtuzumab ozogamicin is particularly useful in pediatric patients with newly diagnosed AML, given the low level of MDR1 expression in this patient population.26,27
The remission rate observed in our study compares favorably with rates observed in adult patients with relapsed AML treated with gemtuzumab ozogamicin reported by Sievers et al15 (30%) and Larson et al16 (28%). Additionally, these results are similar to those of 2 published reports in which gemtuzumab ozogamicin was used to treat children with refractory/relapsed AML on a compassionate-use basis.18,19 As reported by Zwaan et al,18 15 children (4 with de novo disease, 11 with relapsed/refractory disease) were administered gemtuzumab ozogamicin in the dose range of 4 to 9 mg/m2 per course. Clinical response included 3 patients achieving CR, 5 patients achieving CRp, and 3 patients with no change in bone marrow blast count. Although survival rates were low, many of these patients had relapses at least once, if not multiple times, and were resistant to multiple chemotherapeutic agents and combinations. Results reported by Reinhardt et al19 in 12 patients with relapsed/refractory disease who were receiving gemtuzumab ozogamicin doses of 1.8 to 9.0 mg/m2 per course did not reveal any CRs. In both compassionate-use reports, one patient in each report experienced VOD. The results cannot be used to predict efficacy or survival in other patients, such as those with nonrelapsed disease or those treated with combination therapy.
The targeting of myeloid cells by gemtuzumab ozogamicin and our demonstration of comparable remission rates in patients with refractory and relapsed disease suggests that this agent should be further tested in combination with standard chemotherapy to increase the initial remission rate of pediatric patients with de novo AML and potentially to increase relapse-free survival. The MTD outlined in this trial may not be the appropriate dose in combination therapy. In adults with AML, De Angelo et al28 reduced the dose of gemtuzumab ozogamicin by 30% when the drug was used with combination chemotherapy. Thus, a dose-escalation combination chemotherapy clinical trial would be suggested as a next step.
This clinical dose-escalation trial demonstrated that single-agent gemtuzumab ozogamicin can be used with acceptable safety and comparable efficacy at 6 mg/m2 in pediatric patients with relapsed and refractory AML. Once these patients enter remission, subsequent therapy is the next issue for physicians to determine. If an appropriate donor has been identified, HSCT is an important consideration in this pediatric population, and our data demonstrate that gemtuzumab ozogamicin can allow patients to achieve sufficient disease control to undergo HSCT. Safely balancing an increased risk for VOD, associated with swift application of transplantation against the risk for recurrent leukemia that often occurs during the interval between remission induction and transplantation, remains a complex challenge for future studies. Recent data suggest that the occurrence of VOD may be reduced if the experimental medication defibrotide is used prophylactically.29 The timing of transplantation after exposure to gemtuzumab ozogamicin and the potential role of prophylaxis for VOD must be studied further, especially when gemtuzumab ozogamicin is used at reduced doses in combination with chemotherapy.
Prepublished online as Blood First Edition Paper, May 10, 2005; DOI 10.1182/blood-2004-10-3821.
Supported by a research grant from Wyeth Research, a division of Wyeth Pharmaceuticals, Philadelphia, PA.
M.S.B. and M.L.S. were employed by the study sponsor, Wyeth Pharmaceuticals, at the time of the study. Both worked directly on the Wyeth product, gemtuzumab ozogamicin, which is discussed in this article. Both authors are now employed by Glaxo SmithKline Pharmaceuticals, Philadelphia, PA, and no longer have a financial interest in gemtuzumab ozogamicin.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 U.S.C. section 1734.