Abstract
Chronic infection with the hepatitis C virus (HCV) is associated with failures of T-cell–mediated immune clearance and with abnormal B-cell growth and activation. We examined the levels of chemokines that bind to CXC chemokine receptor 3 (CXCR3) to determine whether such chemokines might play a role in the failure of the immune system to clear HCV infection. Elevations in CXC ligand 9 (CXCL9), CXCL10, and CXCL11 were observed in all patients with HCV. CXCR3 expression was increased significantly on peripheral blood B lymphocytes, but not T lymphocytes, from individuals with HCV infection. Chemokine levels were measured in samples collected before, during, and after antiviral therapy from a group of 29 patients infected with HCV genotypes 1a (24 patients) and 1b (5 patients). Levels of CXCL10 and CXCL9 decreased following successful antiviral therapy; CXCL11 did not decline significantly during or in the first 6 months after therapy. The baseline level of CXCL10 (measured before the start of antiviral treatment) was greatest in patients with HCV who subsequently became nonresponders to therapy. These results suggest that plasma concentrations of immunoreactive CXCL10 may be a predictor of responsiveness or nonresponsiveness to antiviral therapy with pegylated interferon (IFN) with or without ribavirin. This observation has implications for understanding the pathogenesis of HCV infection.
Introduction
At least 170 million people worldwide are chronically infected with the hepatitis C virus (HCV) (reviewed in Lauer and Walker1 and Poynard et al2 ). Infection is spread primarily through the parenteral route, and the epidemic continues among those who share needles and drugs. Chronic infection can progress to cirrhosis, hepatocellular carcinoma, and liver failure. HCV infection is now the leading indication for liver transplantation in the United States and Europe.2 Antiviral therapy for HCV infection has improved significantly in recent years and typically includes 24 to 48 weeks of therapy with pegylated interferon α (IFNα) and ribavirin. This regimen is successful in approximately 50% to 60% of those treated, meaning that HCV RNA remains undetectable 6 months after completion of therapy (sustained virologic response, SVR). However, there are still those in whom treatment has little to no effect on levels of circulating viral RNA (nonresponders). In addition, the virus burden rebounds during therapy in some patients who had initially responded (breakthrough); in others who responded during treatment, HCV RNA reemerges after completion of therapy (relapse). The factors that determine the outcome of therapy are poorly understood. It is clear that viral sequences play a role in determining the outcome of therapy, since the response rates differ among individuals infected with different HCV genotypes.3 HCV genotype 1, which infects approximately 77% of US patients with HCV,4 is difficult to treat. In contrast, HCV genotypes 2 and 3, together accounting for approximately 22% of US patients, respond to therapy with pegylated IFNα and ribavirin in a majority of cases. HCV genotypes 1a and 1b are typically treated for 48 weeks, while HCV genotypes 2 and 3 can often be successfully treated in only 24 weeks. Host differences also contribute to different therapy outcomes; thus, response rates differ among different racial groups.5,6
The actions of pegylated IFNs and ribavirin may be mediated by a combination of direct antiviral effects and stimulation of immune function. Type I IFNs are produced in the infected liver,7 but they may not be sufficient to eliminate viral infection.7 Some reports suggest that HCV proteins can directly block IFN signal transduction and downstream effects.8 Studies of viral kinetics show that HCV viremia declines rapidly in the early hours and days of IFN therapy, presumably because of reduced HCV replication within infected hepatocytes.9,10 However, the second phase of HCV decline—and sustained control of HCV replication—may be mediated by immunologic mechanisms, including IFNγ secretion and cytolytic elimination of infected cells.11,12 Direct cytolytic mechanisms of viral control require that effector cells home to the liver, the primary site of HCV replication. Ethical concerns have limited the study of intrahepatic immune responses during antiviral therapy, because such studies would entail repeated biopsies. Studies of peripheral blood T-cell responses to HCV antigens during antiviral therapy have yielded conflicting results13,14 ; thus, the role of acquired immunity in clearance of HCV during IFN-ribavirin therapy is not firmly established.
Control of HCV infection may depend in part on chemokine-mediated recruitment of specific T cells to the liver. The chemokines comprise a set of 43 small proteins that influence cell localization, function, and growth by binding to G protein–coupled receptors on target cells (reviewed in von Andrian and Mackay15 and Rot and Von Andrian16 ). Chemokines associate with endothelial cells and the extracellular matrix near the site of their production, but elevated levels of specific chemokines have been reported in serum from patients infected with HCV.17-20 CXC ligand 9 (CXCL9) (monokine induced by IFNγ, MIG) was associated with hepatic sinusoidal endothelium in normal liver and was increased in liver tissue from patients with end-stage HCV infection.21 CXCL10 (IFNγ-inducible protein 10, IP-10) may be produced by hepatocytes, sinusoidal endothelial cells, lymphoid cells, and monocytoid cells in the infected liver.19,21 CXCL11 (IFN-inducible T-cell α chemoattractant, I-TAC) protein and mRNA were associated with hepatic sinusoidal endothelial cells and hepatocytes in areas of inflammation.22 Intrahepatic T and B cells in end-stage hepatitis C express the CXC chemokine receptor 3 (CXCR3) receptor for CXCL9, CXCL10, and CXCL11.21,23 CXCR3 is prominent on effector T cells and is associated with a T-helper cell type 1 (TH1)–type response.15 These observations suggest that chemokines that bind to CXCR3 are important regulators of T- and/or B-cell localization in the liver during HCV infection.
We have previously observed that some patients with HCV had an increased frequency of circulating B lymphocytes.24 Because the increased B cells did not express activation markers, we hypothesized that they were increased in the circulation as a result of changes in the cytokine or chemokine environment in patients with HCV. We set out to test this hypothesis by measuring the levels of cytokines and chemokines that could affect lymphocyte localization and mobilization. Significant changes were noted in the levels of some chemokines.
Patients, materials, and methods
Patients
The details of these studies were approved by institutional review boards at Saint Louis University School of Medicine, Weill Cornell Medical College, and Rockefeller University. All subjects gave written informed consent before donating blood. Patients with HCV not currently on antiviral therapy were studied for Figures 1 and 2. Control subjects included 58 self-reported healthy volunteers and 42 sustained responders who remained free of detectable HCV RNA more than 6 months after completion of therapy. In addition, 9 patients who achieved SVR during the course of this study (see Table 2) were also included in the SVR analysis in Figure 1, bringing the total number of SVR samples analyzed to 51. Sustained responder samples were collected an average of 12.2 months after completion of therapy (SD, 11.5). Demographic information about these patients and control subjects is summarized in Table 1.
Response data for patients who donated serial samples
Patient no. . | Treatment group . | Day-29 response* . | EVR at wk 12† . | ETR at wk 48‡ . | SVR at wk 72 or beyond§ . | Summary . |
|---|---|---|---|---|---|---|
| 1 | B | + | + | + | + | SVR |
| 2 | A | + | + | - | - | Breakthrough |
| 3∥ | A | + | + | + | + | SVR |
| 4 | A | - | + | + | - | Relapse |
| 5∥ | A | + | + | + | + | SVR |
| 6¶ | A | - | - | - | - | Nonresponder |
| 7 | A | + | + | + | + | SVR |
| 8 | A | - | - | - | - | Nonresponder |
| 9 | A | - | - | - | - | Nonresponder |
| 10 | C | - | + | + | - | Relapse |
| 11 | C | + | + | + | + | SVR |
| 12 | C | - | - | - | - | Nonresponder |
| 13 | C | - | + | + | + | SVR |
| 14 | C | - | + | + | - | Relapse |
| 15 | C | - | - | - | - | Nonresponder |
| 16 | B | + | + | + | + | SVR |
| 17 | B | - | - | - | - | Nonresponder |
| 18 | B | + | + | + | - | Relapse |
| 19 | B | + | + | - | - | Breakthrough |
| 20 | B | - | - | - | - | Nonresponder |
| 21 | B | - | + | - | - | Breakthrough |
| 22 | B | + | + | + | + | SVR |
| 23 | B | - | - | - | - | Nonresponder |
| 24 | B | - | - | - | - | Nonresponder |
| 25 | B | - | - | + | - | Relapse |
| 26 | B | + | + | + | + | SVR |
| 27 | B | - | - | - | - | Nonresponder |
| 28 | B | + | + | + | + | SVR |
| 29 | B | + | + | + | + | SVR |
Patient no. . | Treatment group . | Day-29 response* . | EVR at wk 12† . | ETR at wk 48‡ . | SVR at wk 72 or beyond§ . | Summary . |
|---|---|---|---|---|---|---|
| 1 | B | + | + | + | + | SVR |
| 2 | A | + | + | - | - | Breakthrough |
| 3∥ | A | + | + | + | + | SVR |
| 4 | A | - | + | + | - | Relapse |
| 5∥ | A | + | + | + | + | SVR |
| 6¶ | A | - | - | - | - | Nonresponder |
| 7 | A | + | + | + | + | SVR |
| 8 | A | - | - | - | - | Nonresponder |
| 9 | A | - | - | - | - | Nonresponder |
| 10 | C | - | + | + | - | Relapse |
| 11 | C | + | + | + | + | SVR |
| 12 | C | - | - | - | - | Nonresponder |
| 13 | C | - | + | + | + | SVR |
| 14 | C | - | + | + | - | Relapse |
| 15 | C | - | - | - | - | Nonresponder |
| 16 | B | + | + | + | + | SVR |
| 17 | B | - | - | - | - | Nonresponder |
| 18 | B | + | + | + | - | Relapse |
| 19 | B | + | + | - | - | Breakthrough |
| 20 | B | - | - | - | - | Nonresponder |
| 21 | B | - | + | - | - | Breakthrough |
| 22 | B | + | + | + | + | SVR |
| 23 | B | - | - | - | - | Nonresponder |
| 24 | B | - | - | - | - | Nonresponder |
| 25 | B | - | - | + | - | Relapse |
| 26 | B | + | + | + | + | SVR |
| 27 | B | - | - | - | - | Nonresponder |
| 28 | B | + | + | + | + | SVR |
| 29 | B | + | + | + | + | SVR |
Patients 1 to 29 from our previous study,24 all infected with HCV genotype 1, were enrolled in a study of viral kinetics and evolution during therapy with pegylated IFNα and ribavirin. Treatment groups A, B, and C are described in “Patients, materials, and methods.” HCV viral load was recorded at frequent intervals during therapy. + and - refer to positive and negative responses, respectively.
A positive day 29 response was defined as a > 2 log10 drop in viral load; a negative day 29 response was defined as a drop of < 1 log10 in viral load.
Early virologic response, EVR, was defined as a > 2 log10 drop in viral load following 12 weeks of therapy.
A positive end-of-treatment response, ETR, was achieved if HCV RNA was undetectable in patient serum at the end of treatment.
An SVR was achieved if HCV RNA remained undetectable in patient serum 6 months after completion of therapy.
These patients, who both achieved SVRs, declined to donate follow-up blood samples at the 72-week time point.
This patient, who was a nonresponder, discontinued therapy before the 48-week point but remained in the study.
Summary of subject demographic data
. | Control . | SVR* . | HCV-infected† . |
|---|---|---|---|
| Total no. | 58 | 51 | 82 |
| Sex, no. | |||
| Male | 30 | 27 | 40 |
| Female | 28 | 22 | 31 |
| Not reported | 0 | 2 | 11 |
| Race/ethnicity, no. | |||
| White | 41 | 44 | 58 |
| African American | 13 | 1 | 8 |
| Asian | 3 | 1 | 2 |
| Other or not reported | 3 | 5 | 13 |
| Hispanic ethnicity | 6 | 0 | 1 |
| HCV genotype, no. | |||
| Genotype 1a | NA | 8 | 37 |
| Genotype 1b | NA | 5 | 21 |
| Genotype 2 | NA | 7 | 7 |
| Genotype 3 | NA | 0 | 1 |
| Mixed genotypes | NA | 1 | 2 |
| Not available | NA | 30 | 14 |
| Mean age, y (SD) | 35.7 (9.6) | 49.8 (9.5) | 50 (10.4) |
| Duration of SVR, mo (range) | NA | 12.2 (1-72) | NA |
. | Control . | SVR* . | HCV-infected† . |
|---|---|---|---|
| Total no. | 58 | 51 | 82 |
| Sex, no. | |||
| Male | 30 | 27 | 40 |
| Female | 28 | 22 | 31 |
| Not reported | 0 | 2 | 11 |
| Race/ethnicity, no. | |||
| White | 41 | 44 | 58 |
| African American | 13 | 1 | 8 |
| Asian | 3 | 1 | 2 |
| Other or not reported | 3 | 5 | 13 |
| Hispanic ethnicity | 6 | 0 | 1 |
| HCV genotype, no. | |||
| Genotype 1a | NA | 8 | 37 |
| Genotype 1b | NA | 5 | 21 |
| Genotype 2 | NA | 7 | 7 |
| Genotype 3 | NA | 0 | 1 |
| Mixed genotypes | NA | 1 | 2 |
| Not available | NA | 30 | 14 |
| Mean age, y (SD) | 35.7 (9.6) | 49.8 (9.5) | 50 (10.4) |
| Duration of SVR, mo (range) | NA | 12.2 (1-72) | NA |
Patients and control subjects are characterized according to sex, race, and ethnicity (self-reported), HCV genotype if applicable, age, and duration of SVR (time between completion of therapy and collection of sample tested in this report).
NA indicates not applicable.
This group includes the 9 sustained responders from Table 2 who provided a blood sample 6 months after completion of treatment.
This group includes all 29 patients from Table 2.
Serial blood samples were obtained for 29 patients infected with HCV genotype 1 (24 with genotype 1a, 5 with genotype 1b), and they were studied further (Tables 2 and 3; Figures 3, 4, 5, 6, 7). These patients were all enrolled in an observational study of HCV kinetics and quasispecies evolution during therapy.25 Clinical and demographic characteristics of these patients have been detailed elsewhere (see Ni et al,24 Table 1, patients 1-29). Briefly, patients ranged in age from 19 to 72 years (mean age, 46.1 years); 17 were men and 12 were women; 5 were African American and the rest were white. All patients had elevated serum aminotransferases. Liver biopsies before treatment showed a mean inflammatory grade of 2.27 (range, 1-3)26 and a mean fibrosis stage of 2.11 (range, 1-4).26,27 These patients provided 3 blood samples 1 week before the start of therapy (baseline), 4 weeks after initiation of therapy, and 24 weeks after completion of 48 weeks of therapy. Viral loads were assessed at frequent intervals throughout treatment and follow-up.
Summary of patient treatment, responses, and pretreatment CXCL10 levels
Treatment group . | No. patients . | . | . | . | . | Mean CXCL10, pg/mL before therapy, ± SD . | ||||
|---|---|---|---|---|---|---|---|---|---|---|
| . | Total . | SVR . | Nonresponders . | Breakthrough . | Relapse . | . | ||||
| A | 8 | 3 | 3 | 1 | 1 | 2421 ± 1324 | ||||
| B | 15 | 6 | 5 | 2 | 2 | 1894 ± 1468 | ||||
| C | 6 | 2 | 2 | 0 | 2 | 1802 ± 969 | ||||
| Total | 29 | 11 | 10 | 3 | 5 | 2020 ± 1322 | ||||
Treatment group . | No. patients . | . | . | . | . | Mean CXCL10, pg/mL before therapy, ± SD . | ||||
|---|---|---|---|---|---|---|---|---|---|---|
| . | Total . | SVR . | Nonresponders . | Breakthrough . | Relapse . | . | ||||
| A | 8 | 3 | 3 | 1 | 1 | 2421 ± 1324 | ||||
| B | 15 | 6 | 5 | 2 | 2 | 1894 ± 1468 | ||||
| C | 6 | 2 | 2 | 0 | 2 | 1802 ± 969 | ||||
| Total | 29 | 11 | 10 | 3 | 5 | 2020 ± 1322 | ||||
Patients in groups A, B, and C received 48 weeks of treatment with pegylated IFNα-2a (Pegasys, Roche), 180 μg per week, by subcutaneous injection. Patients in treatment group B also received ribavirin (Copegus, Roche) at 1000 to 1200 mg/d in 2 divided doses based on body weight (those weighing > 75 kg received the higher dose). Patients in group C received pegylated IFNα-2a alone for the first 5 weeks, then received a further 48 weeks of therapy with pegylated IFNα-2a plus ribavirin dosed according to weight. There were no statistically significant differences in the response rates of patients in the 3 groups. The right-most column shows the mean CXCL10 levels (± SD) for each group at baseline. There was no statistically significant difference in the level of CXCL10 in pretreatment plasma samples from patients in the 3 groups.
Antiviral therapy
Patients were treated with pegylated IFNα-2a (Pegasys; Roche, Nutley, NJ) at 180 μg per week by subcutaneous injection. Patients in treatment group A (Table 2) were treated with pegylated IFNα-2a alone for 48 weeks; those in treatment group B also received ribavirin (Copegus; Roche) at 1000 to 1200 mg/d in 2 divided doses based on body weight (those weighing > 75 kg received the higher dose). Patients in group C received pegylated IFNα-2a alone for the first 5 weeks, then received 48 weeks of therapy with pegylated IFNα-2a plus ribavirin dosed according to weight. This last group was the result of a change in standard therapy for HCV infection after initiation of the study; because data were published about the benefits of ribavirin treatment, it was no longer considered ethical to test the effects of pegylated IFNα-2a alone on viral parameters.
Sample preparation
Blood was collected into Vacutainer (Becton Dickinson, Franklin Lakes, NJ) tubes coated with acid citrate–dextrose solution A and processed immediately after collection. Immediate processing may be particularly important for chemokine studies, in light of reports that chemokine gene transcription can change dramatically during storage of whole blood for periods of as little as 1 hour.28 Plasma was collected by centrifugation at 500g and stored in aliquots at –80°C until studied. Peripheral blood mononuclear cells (PBMCs) were prepared as previously described24 and stored for flow cytometric analysis. Samples that had been divided into aliquots were thawed immediately before assay and were not reused.
Chemokine measurements
All plasma samples were brought to 50 mM EDTA (ethylenediaminetetraacetic acid) before study by addition of 0.1 volume of 500 mM EDTA, pH 8.0. In preliminary experiments, we found that the addition of EDTA improved the reproducibility of our measurements, perhaps because of the inhibition of the coagulation pathway in plasma fractions. The human Chemokine Kit I Cytometric Bead Array system (BD Biosciences, San Jose, CA) was used as per the manufacturer's instructions for analysis of serum, except for the addition of EDTA to plasma samples. CXCL9 and CXCL10 measurements obtained in Cytometric Bead Array assays were confirmed by enzyme-linked immunosorbent assay (ELISA; R&D Systems, Minneapolis, MN) according to the manufacturer's instructions. CXCL11 levels were determined by ELISA (R&D Systems) according to the manufacturer's instructions. ELISAs were read on a Fusion from PerkinElmer (Boston, MA).
Flow cytometric analysis
Freshly thawed PBMCs were stained and analyzed as previously described.24 Antibodies used for this work included anti-CD20 (clone 2H7, mouse immunoglobulin G2b [IgG2b], κ), anti-CD3 (clone UCHT1, mouse IgG1, κ), and anti-CXCR3 (clone 1C6/CXCR3, mouse IgG1, κ), all from BD Biosciences. Twenty thousand cells, gated by forward and right-angle light scatter for lymphocytes, were analyzed on a FACSCalibur flow cytometer (BD Immunocytometry Systems, San Jose, CA). In control experiments, we verified that cryopreserved PBMCs retained expression of CXCR3 (Figure S1, available on the Blood website; see the Supplemental Figure link at the top of the online article).
Data analysis
Cytometric bead array data were collected on a FACSCalibur using CellQuest software and analyzed using BD Cytometric Bead Array software (both from BD Biosciences). Flow cytometric data were acquired using CellQuest and analyzed using FlowJo (TreeStar, Ashland, OR). All statistical analyses were performed with Prism (GraphPad Software, San Diego, CA). Nonparametric statistics were used to compare populations (Mann-Whitney test, Kruskal-Wallis test, Dunn multiple comparison test). The Friedman test was used to evaluate changes in chemokine levels over time. Contingency tables were evaluated using chi-square analysis. Two-tailed P values were calculated for all tests, and a P value of less than .05 was considered significant.
Results
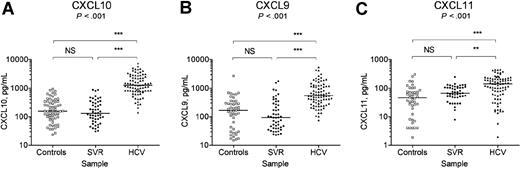
To learn whether chemokine changes contributed to the observed changes in peripheral blood lymphocyte subsets in patients with HCV,24 we measured the levels of a number of chemokines in plasma prepared from the donated blood of patients with HCV not currently on IFN-ribavirin treatment, sustained responders, and self-reported healthy controls. All 3 of the chemokines that bind to the receptor CXCR3 were increased in plasma from individuals with current HCV infection (Figure 1). We observed significant increases in the plasma levels of CXCL10 (Figure 1A), CXCL9 (Figure 1B), and CXCL11 (Figure 1C) in patients with HCV not currently on antiviral therapy. In all cases, control subjects and patients who had already achieved SVR were not significantly different from each other (P > .05, Dunn multiple comparison test), while patients with HCV had significant elevations of each chemokine compared with either control subjects or sustained responders. The greatest increase was in CXCL10, with median levels in patients with HCV (1267 pg/mL) more than 8 times as high as those in control subjects (155.2 pg/mL) or in patients who had already achieved an SVR (130.5 pg/mL). CXCL10 levels were higher among patients with higher inflammation and fibrosis scores on liver biopsy, although this difference was not statistically significant (P > .05, Kruskal-Wallis test; data not shown). Of note, plasma CXCL10 levels were higher among African American patients with HCV infection than among whites with HCV infection (P = .038, Mann-Whitney test); in contrast, in HCV-uninfected individuals, CXCL10 levels were somewhat lower among African Americans than among whites (P = .051). We did not observe any race-specific differences in CXCL9 or CXCL11 levels in patients with HCV or in healthy donors. No correlations were noted between CXCL10 levels and patient sex or viral load (data not shown).
Plasma CXCL9, CXCL10, and CXCL11 levels are elevated in patients with current HCV infection. (A) CXCL10 was measured by cytometric bead array, and levels were confirmed by ELISA in control subjects (n = 58), sustained responders (SVR; n = 51), and patients with HCV (n = 82). (B) CXCL9 was measured by cytometric bead array, and levels were confirmed by ELISA in control subjects (n = 44), sustained responders (n = 50), and patients with HCV (n = 82). (C) CXCL11 was measured by ELISA in control subjects (n = 44), sustained responders (n = 47), and patients with HCV (n = 81). Lines across each column represent the median value for each set of measurements. Values of P at the top of each graph were calculated by the Kruskal-Wallis test. Dunn multiple comparison test was used as a posttest to compare each group of samples to each other group; NS indicates not significant; **P < .01; ***P < .001.
Plasma CXCL9, CXCL10, and CXCL11 levels are elevated in patients with current HCV infection. (A) CXCL10 was measured by cytometric bead array, and levels were confirmed by ELISA in control subjects (n = 58), sustained responders (SVR; n = 51), and patients with HCV (n = 82). (B) CXCL9 was measured by cytometric bead array, and levels were confirmed by ELISA in control subjects (n = 44), sustained responders (n = 50), and patients with HCV (n = 82). (C) CXCL11 was measured by ELISA in control subjects (n = 44), sustained responders (n = 47), and patients with HCV (n = 81). Lines across each column represent the median value for each set of measurements. Values of P at the top of each graph were calculated by the Kruskal-Wallis test. Dunn multiple comparison test was used as a posttest to compare each group of samples to each other group; NS indicates not significant; **P < .01; ***P < .001.
Because CXCL9, CXCL10, and CXCL11 are all bound by the receptor CXCR3, we measured CXCR3 expression on PBMCs. We observed CXCR3 expression on subsets of both T and B lymphocytes from healthy control subjects (Figure 2A) as well as patients with HCV (Figure 2B). T-cell expression of CXCR3 was consistent with previous reports.29,30 CXCR3 expression was also observed on a subset of non-B, non-T cells that included cells expressing natural killer markers (data not shown). The frequency of total peripheral blood lymphocytes bearing CXCR3 varied widely between individuals and was not correlated with plasma levels of chemokines binding to CXCR3 in the same individual (data not shown). As a group, patients with HCV had significantly higher frequencies of B cells expressing CXCR3 than did healthy control subjects (Figure 2C). This increase was most striking in patients with normal to low numbers of circulating B cells (Figure 2D). CXCR3 expression was not significantly increased on T lymphocytes (Figure 2C) or on non-B, non-T cells (data not shown) from patients with HCV.
Increased expression of CXCR3 on B cells from patients with HCV infection. (A) PBMCs from a healthy donor were stained for CD3, CD20, and CXCR3. T and B cells identified by staining for CD3 or for CD20, respectively, were analyzed for expression of CXCR3. Numbers in dot plots represent the percentage of gated cells within the region indicated. (B) PBMCs from a patient with HCV were stained for CD3, CD20, and CXCR3. T and B cells identified by staining for CD3 or CD20, respectively, were analyzed for expression of CXCR3. (C) Frequency of T lymphocytes and B lymphocytes expressing CXCR3 among healthy donors and patients with HCV. Patient samples came from chronically infected patients who had not received antiviral therapy for at least 6 months. Lines across each column represent the median value for each group. Values of P were calculated by the Mann-Whitney test. (D) Frequency of CD20+ B lymphocytes expressing CXCR3 plotted against the frequency of PBMCs expressing CD20 in the same sample for the 29 patients listed in Table 2. Samples were obtained 1 week before the start of antiviral therapy. The symbols used indicate the outcome of therapy (▪, no response; ▵, SVR; ×, transient response followed by breakthrough or relapse). The values are correlated for the patients as a group (Spearman r = –0.6407, P = .001) and for nonresponders to antiviral therapy (Spearman r = –0.8788, P = .001).
Increased expression of CXCR3 on B cells from patients with HCV infection. (A) PBMCs from a healthy donor were stained for CD3, CD20, and CXCR3. T and B cells identified by staining for CD3 or for CD20, respectively, were analyzed for expression of CXCR3. Numbers in dot plots represent the percentage of gated cells within the region indicated. (B) PBMCs from a patient with HCV were stained for CD3, CD20, and CXCR3. T and B cells identified by staining for CD3 or CD20, respectively, were analyzed for expression of CXCR3. (C) Frequency of T lymphocytes and B lymphocytes expressing CXCR3 among healthy donors and patients with HCV. Patient samples came from chronically infected patients who had not received antiviral therapy for at least 6 months. Lines across each column represent the median value for each group. Values of P were calculated by the Mann-Whitney test. (D) Frequency of CD20+ B lymphocytes expressing CXCR3 plotted against the frequency of PBMCs expressing CD20 in the same sample for the 29 patients listed in Table 2. Samples were obtained 1 week before the start of antiviral therapy. The symbols used indicate the outcome of therapy (▪, no response; ▵, SVR; ×, transient response followed by breakthrough or relapse). The values are correlated for the patients as a group (Spearman r = –0.6407, P = .001) and for nonresponders to antiviral therapy (Spearman r = –0.8788, P = .001).
Serial samples were obtained from the patients listed in Table 2, who had enrolled in a clinical study of HCV dynamics and quasispecies evolution during antiviral therapy with pegylated IFNα-2a with or without ribavirin.25 Their clinical and demographic characteristics have been reported previously.24 Patients were enrolled in 1 of 3 treatment groups (See “Patients, materials, and methods” for details). Serum viral RNA was measured at frequent intervals before, during, and after treatment. The success of antiviral therapy was assessed at day 29, week 12, at the end of therapy, and 24 weeks after completion of therapy (Table 2). There were no significant differences between treatment groups in the rates of SVR (Table 3); note that this study was not designed to test the efficacy of the different treatment regimens. The details of the treatment and response profiles will be reported elsewhere. Two of the patients who achieved an SVR declined to donate a sample of blood for analysis at the 72-week time point. As summarized in Table 3, 11 patients in this group had an SVR; 10 patients did not respond to antiviral therapy; 8 patients had transient responses but became viremic again either during therapy (breakthrough) or after completion of therapy (relapse). Patients in groups A, B, and C had similar levels of plasma chemokines before the start of therapy (Table 3 and data not shown).
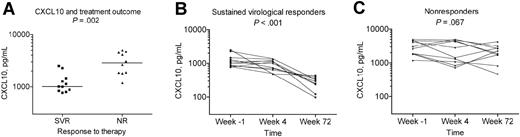
We measured levels of CXCL9, CXCL10, and CXCL11 in plasma samples collected at points 1 week before initiation of therapy (baseline), 29 days after initiation of therapy, and 6 months after completion of therapy. As shown in Figure 3A, baseline CXCL10 levels were significantly higher in the 10 patients who were complete nonresponders to therapy than in the 11 patients who achieved an SVR. This observation has been repeated with samples from a second group of 34 patients, from whom only a single pretreatment sample was available (data not shown). Furthermore, CXCL10 levels declined in samples collected during and after antiviral therapy in patients who achieved sustained control of HCV infection (Figure 3B). After completion of therapy, sustained responders had plasma levels of CXCL10 comparable to those in healthy control subjects (Figures 3B and 1A). In contrast, in patients who did not respond to antiviral therapy, CXCL10 levels remained elevated at the 4-week and 72-week time points (Figure 3C). While patients whose viral loads declined only transiently during therapy did not show a specific pattern of CXCL10 elevation at baseline, they are included in the analyses discussed below.
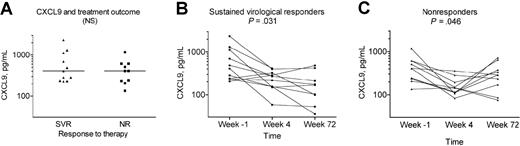
Levels of CXCL9 were also measured in serial plasma samples from the same group of patients. Pretreatment samples showed no consistent differences in CXCL9 levels between patients who subsequently failed therapy and those who subsequently developed a sustained response to antiviral therapy (Figure 4A). Levels of CXCL9 declined during therapy in both responders and nonresponders (Figure 4B-C). Among sustained responders, levels of CXCL9 remained low after completion of therapy (Figure 4B). In nonresponders, the drop in CXCL9 was transient (Figure 4C). CXCL9 levels were not significantly different in sustained responders after treatment, when compared with healthy control subjects (Figure 1B).
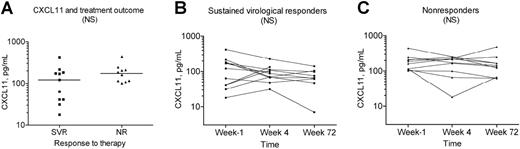
Levels of CXCL11 were measured in serial plasma samples from the same group of patients. There was no association between pretreatment levels of CXCL11 and the outcome of treatment (Figure 5A). CXCL11 levels did not show consistent changes during or in the first 6 months after treatment among sustained responders (Figure 5B) or nonresponders (Figure 5C) to therapy. When samples from a larger group of sustained responders, who had been clear of detectable serum HCV RNA for periods of up to 6 years, were analyzed, CXCL11 levels were not significantly higher in this group than in healthy control subjects (Figure 1C). Thus, CXCL11 may eventually return to normal levels, perhaps more slowly than do CXCL10 and CXCL9. Together, the results of repeated measurements of CXCL10, CXCL9, and CXCL11 over time demonstrate that the plasma level of each of these chemokines is subject to distinct regulatory influences. Of the 3 chemokines that stimulate CXCR3, CXCL10 is most closely associated with the outcome of treatment for HCV infection.
Early responses to antiviral therapy are a key predictor of treatment responses after completion of therapy; patients infected with genotype 1 who fail to demonstrate significant reductions in HCV load by 12 weeks of therapy are very unlikely to be cured.31 Among the 29 patients studied here, we found that the level of CXCL10 in plasma collected before the start of treatment was associated with early responses to treatment (Figure 6). The effectiveness of antiviral therapy was assessed after 4 weeks (Figure 6A) and after 12 weeks (Figure 6B). Fourteen patients demonstrated a more than 2 log10 reduction in viral load at 4 weeks; median pretreatment CXCL10 levels in this group were 1005 pg/mL. Fifteen patients showed poor early responses to therapy, with reductions in viral load of less than 1 log10 after 4 weeks. Median pretreatment CXCL10 levels in this group were 2307 pg/mL. After 12 weeks of therapy, 18 patients demonstrated an early virologic response (EVR). In this group, the median CXCL10 measured before the start of treatment was 1023 pg/mL. Patients who failed to demonstrate an EVR had greater levels of CXCL10 before the start of therapy, with a median measurement of 2639 pg/mL.
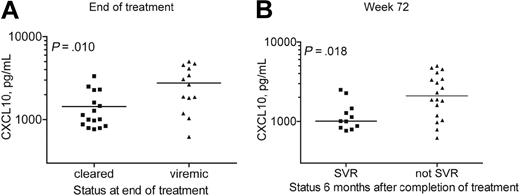
Later responses to therapy were also correlated with CXCL10 levels in baseline plasma samples. At the end of 48 to 52 weeks of therapy, 16 patients were free of measurable serum HCV RNA; these patients had median CXCL10 levels of 1072 pg/mL before treatment (Figure 7A). The 13 patients who were viremic at the completion of therapy had median CXCL10 levels of 2639 pg/mL before the start of therapy (Figure 7A). SVR was assessed 6 months after completion of therapy (Figure 7B). Eleven patients in this group of 29 remained free of detectable HCV RNA at this time point; their pretreatment levels of CXCL10 were lower than in the 18 patients who were viremic at this time point. The latter group includes nonresponders as well as individuals who responded transiently at some point during treatment.
Plasma CXCL10 levels in sustained responders versus nonresponders to antiviral therapy. Serial samples were obtained from patients described in Table 2. (A) CXCL10 levels measured 7 days before the start of therapy are lower in those who subsequently achieve an SVR (n = 11) than in those who subsequently have no reduction in HCV RNA during or after antiviral therapy (NR; n = 10). Lines across each column represent the median for each set of measurements. Value of P was calculated by the Mann-Whitney test. (B-C) CXCL10 levels were measured in plasma obtained 7 days before initiation of antiviral therapy, 29 days after initiation of therapy, and 24 weeks after completion of therapy. Results are plotted separately for patients who subsequently achieved an SVR (B) and for patients who did not respond to antiviral therapy (C). Value of P (comparing the levels of CXCL10 at different points during treatment) was calculated by the Friedman test, a nonparametric repeated measures analysis of variance (ANOVA).
Plasma CXCL10 levels in sustained responders versus nonresponders to antiviral therapy. Serial samples were obtained from patients described in Table 2. (A) CXCL10 levels measured 7 days before the start of therapy are lower in those who subsequently achieve an SVR (n = 11) than in those who subsequently have no reduction in HCV RNA during or after antiviral therapy (NR; n = 10). Lines across each column represent the median for each set of measurements. Value of P was calculated by the Mann-Whitney test. (B-C) CXCL10 levels were measured in plasma obtained 7 days before initiation of antiviral therapy, 29 days after initiation of therapy, and 24 weeks after completion of therapy. Results are plotted separately for patients who subsequently achieved an SVR (B) and for patients who did not respond to antiviral therapy (C). Value of P (comparing the levels of CXCL10 at different points during treatment) was calculated by the Friedman test, a nonparametric repeated measures analysis of variance (ANOVA).
Discussion
Chemokines are central regulators of leukocyte mobilization and entry into inflamed tissues. These small proteins are generally believed to act locally, associating noncovalently with glycosaminoglycans on cell surfaces and the extracellular matrix near the site of production and release.16 The first steps in leukocyte migration into the tissues are tethering and rolling of leukocytes along vascular endothelia, often mediated by interactions of selectins or α4 integrins with their ligands.16,32 Chemokine recognition causes leukocytes to stop rolling and to undergo tight integrin-mediated adhesion followed by integrin-mediated directed migration across endothelial barriers, toward higher chemokine concentrations.15,16
CXCL9, CXCL10, and CXCL11 all bind with different affinities to the receptor CXCR3. CXCR3, in turn, is expressed by effector TH1 cells as well as subsets of other T and B cells.15 We found significant increases in the plasma levels of all 3 of these chemokines in patients with HCV compared with healthy donors and to recovered patients with HCV. In serial samples from patients with HCV undergoing antiviral treatment, we found that CXCL10 levels decline during successful antiviral treatment, but they remain elevated during and after treatment in nonresponders to therapy. Of note, pretreatment levels of CXCL10 were significantly lower in patients who went on to achieve an SVR than in those who failed to respond to therapy. Early responsiveness to therapy was also associated with lower levels of CXCL10 at baseline. CXCL9 and CXCL11 levels at baseline did not show significant associations with the outcome of therapy. These results suggest that pretreatment levels of CXCL10 may have predictive value in determining the likelihood that treatment with pegylated IFNα and ribavirin will be successful. Other groups have also noted a correlation between CXCL10 levels in patient blood and the outcome of therapy with standard IFN19 or with pegylated IFN plus ribavirin.33 The frequency of peripheral blood B cells expressing CXCR3 is also significantly increased in patients with HCV. The mechanisms leading to enhanced CXCR3 expression on HCV patient B lymphocytes are not yet known.
Plasma CXCL9 levels in sustained responders versus nonresponders to antiviral therapy. Serial samples were obtained from patients described in Table 2. (A) CXCL9 levels measured 7 days before the start of therapy are lower in those who subsequently achieve an SVR (n = 11) than in those who subsequently have no reduction in HCV RNA during or after antiviral therapy (NR; n = 10). Lines across each column represent the median for each set of measurements. Value of P was calculated by the Mann-Whitney test. (B-C) CXCL9 levels were measured in plasma obtained 7 days before initiation of antiviral therapy, 29 days after initiation of therapy, and 24 weeks after completion of therapy. Results are plotted separately for patients who subsequently achieved an SVR (B) and for patients who did not respond to antiviral therapy (C). Value of P (comparing the levels of CXCL9 at different points during treatment) was calculated by the Friedman test.
Plasma CXCL9 levels in sustained responders versus nonresponders to antiviral therapy. Serial samples were obtained from patients described in Table 2. (A) CXCL9 levels measured 7 days before the start of therapy are lower in those who subsequently achieve an SVR (n = 11) than in those who subsequently have no reduction in HCV RNA during or after antiviral therapy (NR; n = 10). Lines across each column represent the median for each set of measurements. Value of P was calculated by the Mann-Whitney test. (B-C) CXCL9 levels were measured in plasma obtained 7 days before initiation of antiviral therapy, 29 days after initiation of therapy, and 24 weeks after completion of therapy. Results are plotted separately for patients who subsequently achieved an SVR (B) and for patients who did not respond to antiviral therapy (C). Value of P (comparing the levels of CXCL9 at different points during treatment) was calculated by the Friedman test.
The 8 African American patients with HCV in this study, as a group, had higher levels of plasma CXCL10 (but not CXCL9 or CXCL11) than did the 58 white patients. Historically, African American patients with HCV have a lower rate of response to antiviral therapy with IFNα and ribavirin than do white patients.5,34,35 The African American control subjects did not have higher levels of CXCL10 than did white control subjects. It will be important to confirm these observations with larger groups of African American and white patients. These results suggest that there may be a relationship between elevated plasma CXCL10 and resistance to the antiviral effects of type I IFNs.
Models for chemokine function typically involve the presentation of chemokines on endothelial surfaces near the site of chemokine production or release. The high levels of these chemokines in the plasma may be a consequence of high local production in the liver; that is, they may represent a type of overflow from surfaces already saturated with chemokines. Alternatively, they may be produced elsewhere, for instance in cells of hematopoietic origin.36 Widespread production and secretion of chemokines may interfere with the gradient sensing needed for lymphocytes to enter specific tissues.16 Indeed, soluble plasma chemokines may act as antagonists for leukocyte migration.37,38 Chemokines at high concentration might induce chemorepulsion.39,40 Thus, while T cells in the HCV-infected liver express CXCR3,21,23 it is not clear that the chemokines we measure in the plasma can promote specific T-cell migration into the liver.
Plasma CXCL11 levels in sustained responders versus nonresponders to antiviral therapy. Serial samples were obtained from patients described in Table 2. (A) CXCL11 levels measured 7 days before the start of therapy are lower in those who subsequently achieve an SVR (n = 11) than in those who subsequently have no reduction in HCV RNA during or after antiviral therapy (NR; n = 10). Lines across each column represent the median for each set of measurements. Value of P was calculated by the Mann-Whitney test. (B-C) CXCL11 levels were measured in plasma obtained 7 days before initiation of antiviral therapy, 29 days after initiation of therapy, and 24 weeks after completion of therapy. Results are plotted separately for patients who subsequently achieved an SVR (B) and for patients who did not respond to antiviral therapy (C). Value of P (comparing the levels of CXCL11 at different points during treatment) was calculated by the Friedman test.
Plasma CXCL11 levels in sustained responders versus nonresponders to antiviral therapy. Serial samples were obtained from patients described in Table 2. (A) CXCL11 levels measured 7 days before the start of therapy are lower in those who subsequently achieve an SVR (n = 11) than in those who subsequently have no reduction in HCV RNA during or after antiviral therapy (NR; n = 10). Lines across each column represent the median for each set of measurements. Value of P was calculated by the Mann-Whitney test. (B-C) CXCL11 levels were measured in plasma obtained 7 days before initiation of antiviral therapy, 29 days after initiation of therapy, and 24 weeks after completion of therapy. Results are plotted separately for patients who subsequently achieved an SVR (B) and for patients who did not respond to antiviral therapy (C). Value of P (comparing the levels of CXCL11 at different points during treatment) was calculated by the Friedman test.
It is thought that IFNγ secreted by activated T cells is crucial for the control of HCV replication.12 Natural killer (NK) cells and HCV-specific T cells must traffic to the liver to kill infected hepatocytes or to control viral replication by nonlytic mechanisms such as directed IFNγ secretion. In rodent models, the accumulation of NK and T cells in the infected liver is orchestrated by production of specific chemokines, which recruit waves of antigen-specific and nonspecific mononuclear cells.41 Some of these cells mediate control of viral replication and some, nonspecific inflammation. In a mouse model of hepatitis B virus (HBV) infection, CXCL9 and CXCL10 were not required for the recruitment and antiviral function of HBV-specific cytotoxic T lymphocytes, but blocking these chemokines prevented hepatic inflammation.42,43 It is possible that CXCR3-binding chemokines in the plasma do not contribute to recruitment of antigen-specific T cells for control of viral replication, but instead to a neutral or detrimental inflammatory reaction.
Members of the CXCR3-binding chemokine family are known to antagonize responses to CC chemokines including CC chemokine ligand 5 (CCL5) (regulated on activation, normal T expressed and secreted; RANTES), eotaxins, and several monocyte-macrophage chemoattractant proteins.16,44,45 Data from patient and chimpanzee studies support an important role for CCL5 in either spontaneous12 or therapeutic46 clearance of HCV infection.12,46 It is difficult to accurately measure plasma CCL5 levels or activity because of release of this chemokine by activated platelets.47
Plasma CXCL10 levels measured before start of therapy correlate with early responses to therapy. (A) CXCL10 levels measured 7 days before the start of therapy were lower in those whose serum viral load declined by > 2 log10 during the first 29 days of therapy than in those whose serum viral load declined by < 1 log10 during the first 29 days of therapy. (B) CXCL10 levels measured 7 days before the start of therapy were lower in patients in whom serum HCV RNA had declined by > 2 log10 by 12 weeks of therapy than in those whose serum viral load declined by < 1 log10 after 12 weeks of antiviral therapy. Measurements from all 29 patients are shown. Lines across each column represent the median for each set of measurements. Value of P was calculated by the Mann-Whitney test.
Plasma CXCL10 levels measured before start of therapy correlate with early responses to therapy. (A) CXCL10 levels measured 7 days before the start of therapy were lower in those whose serum viral load declined by > 2 log10 during the first 29 days of therapy than in those whose serum viral load declined by < 1 log10 during the first 29 days of therapy. (B) CXCL10 levels measured 7 days before the start of therapy were lower in patients in whom serum HCV RNA had declined by > 2 log10 by 12 weeks of therapy than in those whose serum viral load declined by < 1 log10 after 12 weeks of antiviral therapy. Measurements from all 29 patients are shown. Lines across each column represent the median for each set of measurements. Value of P was calculated by the Mann-Whitney test.
CXCR3 binding chemokines may be proteolytically processed after release, and such processing may reduce the ability of these chemokines to act as agonists for CXCR3.16 Processing of CXCL11 at its amino terminus changes it to a CXCR3 antagonist.48 Work is ongoing to determine whether plasma CXCL10 in patients with HCV is truncated at the amino terminus, and whether there is any relationship between the relative frequencies of truncated or full-length chemokines and the outcome of antiviral therapy.
In summary, we have observed that patients with HCV infection have increased plasma levels of 3 chemokines that can stimulate CXCR3. CXCR3 expression was increased among peripheral blood B lymphocytes, but not T lymphocytes, in patients with HCV. CXCL10 levels before the start of antiviral therapy were lower among those who had an EVR and then went on to have an SVR than among those who failed to respond to antiviral therapy. Elevated CXCL10 measured in the plasma may represent overproduction in the liver, or it may be produced by cells distant from the liver as part of a broader antiviral response. It remains to be determined whether the measured CXCL10 plays a neutral, positive, or negative role in the migration of effector T cells to the infected liver. Antagonism, if it occurs, may result from interference with the signaling of other chemokines such as CCL5, competition for recognition between the soluble chemokine and chemokines presented at the site of infection, or amino-terminal processing of the chemokines leading to altered functional effects on target cells.
Plasma CXCL10 levels measured before start of therapy correlate with long-term responses to therapy. (A) CXCL10 levels measured 7 days before the start of therapy were lower in patients in whom serum HCV RNA was undetectable at the end of antiviral therapy than in those who remained viremic at the end of antiviral therapy. (B) CXCL10 levels measured 7 days before the start of therapy were lower in patients in whom serum HCV RNA remained undetectable 24 weeks after completion of therapy than in those who were viremic 24 weeks after completion of antiviral therapy. Measurements from all 29 patients are shown. Lines across each column represent the median for each set of measurements. Value of P was calculated by the Mann-Whitney test.
Plasma CXCL10 levels measured before start of therapy correlate with long-term responses to therapy. (A) CXCL10 levels measured 7 days before the start of therapy were lower in patients in whom serum HCV RNA was undetectable at the end of antiviral therapy than in those who remained viremic at the end of antiviral therapy. (B) CXCL10 levels measured 7 days before the start of therapy were lower in patients in whom serum HCV RNA remained undetectable 24 weeks after completion of therapy than in those who were viremic 24 weeks after completion of antiviral therapy. Measurements from all 29 patients are shown. Lines across each column represent the median for each set of measurements. Value of P was calculated by the Mann-Whitney test.
Prepublished online as Blood First Edition Paper, April 28, 2005; DOI 10.1182/blood-2005-01-0126.
Supported by the National Institutes of Health (grants U01AI49712 and R01AI60561).
D.B. and S.M. performed the research, analyzed the data, and wrote the paper; A.E.I. and E.H. performed the research; T.J.C., A.M.D., E.D.C., A.H.T., and I.M.J. recruited patients, provided samples for research, and analyzed and interpreted the results; C.M.R. provided analysis and interpretation of results and is head of the laboratory; L.B.D. was principal investigator, performed the research, analyzed the data, interpreted the results, and wrote the paper.
D.B. and S.M. contributed equally to this work.
The online version of the article contains a data supplement.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 U.S.C. section 1734.
We thank Gertrudis Soto and Drs Barbara O'Sullivan and Furqaan Ahmed for assistance with patient samples and patient data. We thank the staff at Rockefeller University's Outpatient Clinic for facilitating sample collection. We thank Candace Perez and Dr Patricia Holst for expert laboratory management. We acknowledge the support of Roche Pharmaceuticals for providing the pegylated IFN and ribavirin used in treatment, and Roche Molecular Systems for providing test kits used to measure HCV RNA levels during therapy.



This feature is available to Subscribers Only
Sign In or Create an Account Close Modal