Abstract
We assessed late mortality in 854 individuals who had survived 2 or more years after autologous hematopoietic cell transplantation (HCT) for hematologic malignancies. Median age at HCT was 36.5 years, and median length of follow-up was 7.6 years. Overall survival was 68.8% ± 1.8% at 10 years, and the cohort was at a 13-fold increased risk for late death (standardized mortality ratio [SMR] = 13.0) when compared with the general population. Mortality rates approached those of the general population after 10 years among patients at standard risk for relapse at HCT (SMR = 1.1) and in patients undergoing transplantation for acute myeloid leukemia (AML; SMR = 0.9). Relapse of primary disease (56%) and subsequent malignancies (25%) were leading causes of late death. Relapse-related mortality was increased among patients with Hodgkin disease (HD; relative risk [RR] = 3.6), non-Hodgkin lymphoma (NHL; RR = 2.1), and acute lymphoblastic leukemia (ALL; RR = 6.5). Total body irradiation (RR = 0.6) provided a protective effect. Nonrelapse-related mortality was increased after carmustine (RR = 2.3) and with use of peripheral blood stem cells (RR = 2.4). Survivors were more likely to report difficulty in holding jobs (RR = 9.4) and in obtaining health (RR = 7.7) or life insurance (RR = 8.4) when compared with siblings. Although mortality rates approach that of the general population after 10 years in certain subgroups, long-term survivors of autologous HCT continue to face challenges affecting their health and well-being.
Introduction
Autologous hematopoietic-cell transplantation (HCT) has become increasingly popular since the mid to late 1980s.1 Mobilization and collection of hematopoietic cells from peripheral blood with the attendant faster hematopoietic recovery has made this approach the treatment of choice for patients with relapsed lymphoma and acute leukemia.2 Improvement in transplantation strategies and supportive care has resulted in a growing number of long-term survivors of autologous HCT. These survivors are potentially at risk for treatment-related complications adversely affecting their long-term survival as well as their health and well-being. Several studies have described late mortality in patients undergoing allogeneic HCT3-5 as well as the functional status of these survivors.6-8 To our knowledge, there are no reports addressing late mortality or functional status among long-term survivors of autologous HCT. Results presented here describe overall and cause-specific mortality among patients who received autologous HCT for hematologic malignancies and specific aspects of functional status such as marital status, employment, and problems with health and life insurance experienced by the long-term survivors of autologous transplantation.
Patients, materials, and methods
The Bone Marrow Transplant Survivor Study (BMTSS), a collaborative effort between the City of Hope Cancer Center and the University of Minnesota, examines the long-term outcomes of individuals who have survived 2 or more years after undergoing HCT as well as similar outcomes in age- and sex-matched siblings. The present report from BMTSS is restricted to individuals who met the following eligibility criteria: (1) primary diagnosis of acute myeloid leukemia (AML), acute lymphoblastic leukemia (ALL), non-Hodgkin lymphoma (NHL), or Hodgkin disease (HD); (2) autologous HCT between 1981 and 1998; and (3) survival of at least 2 years from HCT irrespective of current disease status. The Human Subjects committees at the participating institutions approved the BMTSS protocol. Informed consent was provided according to the Declaration of Helsinki.
Mortality analysis
Vital status information was obtained from several sources, including medical records, National Death Index (NDI), and Social Security Death Registry. Vital status of the BMTSS subjects was ascertained as of June 30, 2003. Information on cause of death was obtained from the NDI Plus program or the medical records. This information was used to categorize the cause of death as (1) a direct consequence of original diagnosis; (2) treatment-related sequelae, defined as death where nonacute treatment effects were considered to be the major contributing factor to the death (eg, subsequent malignant neoplasms, cardiopulmonary toxicity); or (3) nontreatment-related causes, such as deaths due to external causes (eg, suicide, car accidents). Information on primary diagnoses and therapeutic agents used for preparative regimens was obtained on all eligible cases from the institution performing the transplantation.
Standardized mortality ratios (SMRs) were used to quantify the risk of death in this cohort. Person-years at risk were computed beginning on the date 2 years from date of HCT and included time to either the date of death or date of censoring (June 30, 2003) for those still alive. To compute the SMRs, an expected number of deaths were calculated9 using age- and sex-specific US mortality rates reported by the National Center for Health Statistics.10 Patients were grouped by age into 5-year intervals. All-cause SMRs were computed for all deaths. Only deaths with known causes, not due to recurrence of the primary disease, were included in cause-specific SMRs for subsequent malignant neoplasms and cardiac, pulmonary, and external causes.
Survival functions were estimated by the product-limit method by age and by diagnosis. To compare survival curves for this cohort with the age-comparable US population, an expected number of deaths for each year since diagnosis was calculated based on the US age- and sex-specific mortality rates, yielding an expected survival function for each sex.
Potential risk factors for late deaths were analyzed using Cox regression models. Age at transplantation (categorized as younger than 18 years, 18 to 45 years, older than 45 years), sex, race, primary diagnosis, disease status at transplantation (standard risk of relapse at HCT and high risk of relapse at HCT), and preparative regimens were included as covariates in the regression model. Patients considered to be at standard risk for relapse included those in first or second complete remission. All other patients were placed into the high-risk category. End points were time to death from any cause, time to relapse-related death, and time to death not related to relapse.
Analysis of marital status, employment, and health/life insurance
Data on specific aspects of functional well-being such as marital status, employment, and problems with health and life insurance experienced by the long-term survivors of autologous HCT were collected for the surviving members of the study cohort who were 18 years of age or older at study participation, using the BMTSS questionnaire. For comparison purposes, 319 nearest-age siblings completed the BMTSS questionnaire. This questionnaire was designed to capture a wide range of information, including demographic characteristics, marital status, insurance coverage, education, income, and employment.
Results
Patient characteristics
Table 1 summarizes the characteristics of the 854 patients who had survived at least 2 years after autologous HCT. The median age at HCT was 36.5 years, and the cohort had been followed for a median of 7.6 years. Primary diagnoses included NHL (46%), HD (29%), AML (19%), and ALL (7%). Most (68.5%) had received peripheral blood stem cells alone or in combination with bone marrow. Cyclophosphamide was used in the conditioning regimen for 97% of the cohort, etoposide in 75%, and total body irradiation in 68% of patients.
Overall survival and SMRs
Of the 854 patients who had survived 2 years after autologous HCT, 251 (29.4%) subsequently died. Most of the deaths (76.5%) occurred in the 2- to 5-year period after autologous HCT, while only 8 deaths (3.2%) occurred after 10 years from HCT, and none were observed beyond 15 years from HCT.
Table 2 summarizes the relative mortality in this population. Overall, late death occurred 13 times more often than expected in the age- and sex-matched general population (SMR = 13.0; 95% confidence interval [CI], 11.5 to 14.7). Increased SMRs were seen in both males (SMR = 10.4; 95% CI, 8.8 to 12.1) and females (SMR = 17.3; 95% CI, 14.0 to 20.9). Patients who were at a high risk for relapse at HCT were at a 17-fold increased risk for late death (SMR = 17.1; 95% CI, 14.3 to 20.1) when compared with the general population, whereas those at a standard risk for relapse at HCT were at a 10-fold higher risk for late death (SMR = 10.2; 95% CI, 8.4-12.1). Relative mortality was highest in subjects undergoing HCT at age less than 18 years (SMR = 60.2; 95% CI, 40.9 to 83.3). Increased relative mortality was also observed across all diagnoses, with the highest values among individuals with a primary diagnosis of ALL (SMR = 43.8; 95% CI, 28.0 to 63.1) and HD (SMR = 28.2; 95% CI, 22.6 to 34.3). Patients undergoing HCT in the earlier years had a higher risk of late death (1980 to 1984: SMR = 49.2; 1985 to 1989: SMR = 22.8) than those undergoing transplantation more recently (1990 to 1994: SMR = 12.5; 1995 to 1999: SMR = 8.7).
Table 3 summarizes the SMRs for this cohort by time since HCT. Relative mortality was highest in the 2- to 5-year period after autologous HCT (SMR = 54.8; 95% CI, 47.3 to 62.9), declined in the 6- to 10-year period (SMR = 5.1; 95% CI, 3.8 to 6.6), with a further decline among those followed for more than 10 years after HCT (SMR = 1.7; 95% CI, 0.7 to 3.0). Certain subgroups of patients followed for more than 10 years from HCT demonstrated mortality rates that were no different from those of the general population—and these included patients undergoing transplantation for AML (SMR = 0.9; 95% CI, 0 to 3.7) as well as patients from all diagnoses who were at standard risk for relapse at HCT (SMR = 1.1; 95% CI, 0.2 to 2.8).
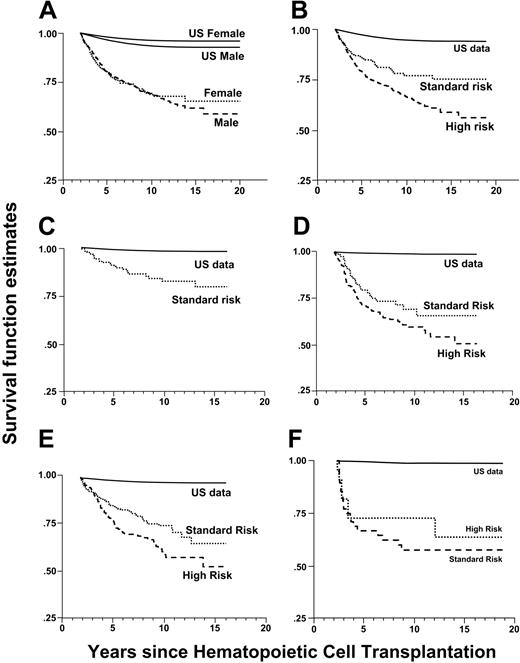
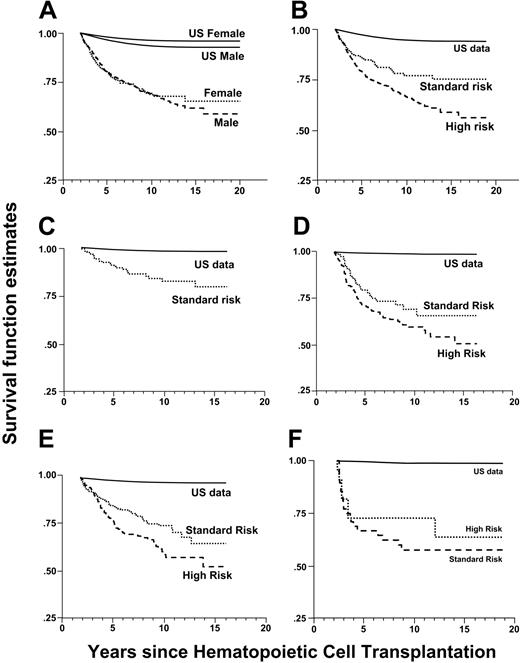
The overall survival was 80.4% ± 1.4% at 5 years and 68.8% ± 1.8% at 10 years from HCT for the 854 patients who had survived at least 2 years after autologous HCT. All-cause mortality experience from 2 years after HCT for the entire cohort and by diagnosis (Figure 1) was compared with age-adjusted expected survival rates for the US population. Individuals with a primary diagnosis of AML had the best overall survival, with cumulative mortality of 17.2% at 10 years, while those with a primary diagnosis of ALL had the lowest overall survival, with a cumulative mortality rate of 39.6% at 10 years.
Specific causes of death
Table 4 shows the distribution of specific cause-of-death categories and the cause-specific SMRs. Relapse of primary disease was the leading cause, with 140 late deaths (56%) attributed to a recurrence of the primary disease. Late death was attributed to treatment-related causes in 108 patients (43%), including 62 (25%) with subsequent malignancy, 6 (2.4%) with cardiac toxicity, 5 (2%) with pulmonary complications, and 35 (13.5%) with other treatment-related sequelae. External causes accounted for late death in 3 patients (1%).
Late deaths attributable to primary disease accounted for a 27-fold higher mortality rate than would be expected in the age- and sex-matched US population. The risk of late death due to primary disease was increased in both male (SMR = 25.4) and female (SMR = 28.5) patients and across all primary diagnoses, with higher relative mortality among patients with HD and ALL than among patients with AML and NHL.
Subsequent malignancy accounted for a 12-fold higher mortality rate than expected from population estimates. A total of 62 deaths due to subsequent malignancies were observed in this cohort. These subsequent malignancies included therapy-related myelodysplasia or AML (n = 40), NHL (n = 2), and solid nonhematopoietic malignancies (n = 20). The 20 fatal solid tumors included the following: malignant neoplasm of bone (n = 1); malignant neoplasm of the brain (n = 3); squamous cell carcinoma of the esophagus (n = 1); hepatocellular carcinoma (n = 1); malignant neoplasm of the liver, not specified primary or secondary (n = 1); malignant neoplasms of bronchus or lung (n = 2); soft tissue sarcoma (n = 2); Merkel cell carcinoma (n = 1); and adenocarcinoma, site unspecified (n = 8). The cohort was at a 5.6-fold increased risk for late deaths due to pulmonary dysfunction when compared with the general population. The risk of late death due to pulmonary dysfunction was increased among males (SMR = 6.7) and among HD survivors (SMR = 29.2). The risk of late death due to cardiac complications was increased among females (SMR = 4.4). The risk of late death due to external causes was not significantly increased in this population when compared with the general population.
Multiple regression analysis for late mortality
Table 5 summarizes the results from the multiple regression analysis for late death from any cause as well as risk of relapse-related and nonrelapse-related late mortality.
Late death due to any cause. The risk of late mortality due to any cause was 2-fold higher among individuals older than age 45 years at HCT when compared with those 45 and younger. When compared with the patients undergoing transplantation for AML, the risk of late mortality was 2-fold among patients undergoing transplantation for NHL and 3-fold for those undergoing transplantation for HD or ALL. The risk of late mortality due to any cause was 1.4-fold higher among individuals at high risk for relapse at time of HCT when compared with those at standard risk for relapse. Total body irradiation and etoposide provided a protective effect such that the risk of late death was 2-fold higher among patients who did not receive total body irradiation compared with those who did and among those who did not receive etoposide relative to those who did receive etoposide in their preparative regimens.
Late death due to relapse. Patients undergoing transplantation for NHL were at a 2-fold higher risk, those underoing transplantation for HD were at a 3.6-fold higher risk, and those undergoing transplantation for ALL were at a 6.5-fold higher risk for relapse-related mortality when compared with those undergoing transplantation for AML. Furthermore, patients at high risk for relapse at HCT were at a 1.4-fold increased risk for relapse-related mortality when compared with those at standard risk. Total body irradiation provided a protective effect such that the risk of relapse-related mortality was 1.7-fold higher among patients conditioned without total body irradiation when compared with those who did receive total body irradiation.
Nonrelapse-related late death. Nonrelapse mortality was increased 2.3-fold among individuals who received carmustine as part of their preparative regimen compared with those who did not. Etoposide offered a protective effect, with nonrelapse mortality increased 2.3-fold among patients not exposed to etoposide when compared with those who had received etoposide as part of their preparative regimen. Patients undergoing transplantation with peripheral stem cells were at a 2.4-fold increased risk for nonrelapse-related mortality when compared with those undergoing transplantation with their bone marrow. The excess risk of nonrelapse mortality among patients receiving peripheral blood stem cells was largely contributed by deaths due to secondary myelodysplasia and AML (29 deaths among patients undergoing transplantation with peripheral blood stem cells, as compared with 6 deaths due to secondary myelodysplasia/acute myeloid leukemia among patients undergoing transplantation with marrow alone and 5 deaths among patients undergoing transplantation with a combination of marrow and peripheral blood stem cells).
All-cause mortality in a cohort of 2-year survivors after autologous HCT. (A) Sex-specific survival for hematologic malignancies for the entire cohort. (B) Mortality for hematologic malignancies for the entire cohort by risk of relapse at HCT. (C) Mortality for acute myeloid leukemia at standard risk for relapse at HCT. Few patients in the high-risk category prevented us from presenting results in the high-risk category. (D) Mortality for Hodgkin disease by risk of relapse at HCT. (E) Mortality for non-Hodgkin lymphoma by risk of relapse at HCT. (F) Mortality for acute lymphoblastic leukemia by risk of relapse at HCT.
All-cause mortality in a cohort of 2-year survivors after autologous HCT. (A) Sex-specific survival for hematologic malignancies for the entire cohort. (B) Mortality for hematologic malignancies for the entire cohort by risk of relapse at HCT. (C) Mortality for acute myeloid leukemia at standard risk for relapse at HCT. Few patients in the high-risk category prevented us from presenting results in the high-risk category. (D) Mortality for Hodgkin disease by risk of relapse at HCT. (E) Mortality for non-Hodgkin lymphoma by risk of relapse at HCT. (F) Mortality for acute lymphoblastic leukemia by risk of relapse at HCT.
Marital, employment, and health/life insurance status
Of the 574 patients in this cohort who were alive and 18 years or older at the time of study participation, 374 (65.2%) responded to the BMTSS questionnaire, 153 (26.6%) declined to participate, and current contact information was not available for 47 (8.2%) patients. Thus, 71% of the individuals who were successfully contacted participated in this part of the study. The participants did not differ from the nonparticipants in the distribution of characteristics such as risk of relapse at HCT, primary diagnosis, and most conditioning agents received. Participants were more likely than nonparticipants to have received total body irradiation (75% versus 66%, P = .03) and less likely to have received carmustine (21% versus 30%, P = .03). There was an overrepresentation of females, (45% versus 36%, P = .05) and whites (85% versus 68%, P < .001) among the participants, and participants were older at time of HCT (median age, 38.0 versus 34.3 years, P = .02) and at time of survey (median age, 45.9 versus 42.3 years, P = .005). The participants had been followed for a shorter time since autologous HCT than the nonparticipants (median, 6.6 versus 8.5 years, P < .001).
Sixty-six percent of the patients reported that they were currently married, similar to the marital status of the sibling comparison group (69%, relative risk [RR] = 1.0, P = .9). Factors independently associated with being currently unmarried included race/ethnicity other than Hispanic or white (RR = 2.5, P = .03), yearly household income of less than $20 000 (RR = 6.9, P < .001) or between $20 000 and $60 000 (RR = 3.0, P < .001), and age at survey 45 years or younger (RR = 1.8, P = .002).
HCT survivors were more likely to report a health problem preventing them from holding a job when compared with siblings (15% versus 2%, RR = 8.3, P < .001). Older study participants were 2.6-fold more likely to report difficulty in holding a job when compared with younger participants.
HCT survivors were also more likely to report difficulty in obtaining or retaining health (27% versus 5%, RR = 7.7, P < .001) or life insurance (33% versus 5%, RR = 8.4, P < .001). Participants 45 years of age or younger at survey completion reported difficulty in obtaining or retaining health insurance (RR = 1.6, P = .04). However, 93% of the survivors had health insurance coverage at the time of study participation, and this proportion did not differ significantly from the siblings (95%, P = .4). On the other hand, only 62% of the survivors had life insurance at study participation, compared with 76% of the siblings (P < .001).
Discussion
Although most autologous transplantation recipients survive the acute complications, little information is available about late mortality experienced by this patient population and specific aspects of functional status such as marital status, employment, and problems with health and life insurance by the long-term survivors of autologous HCT. Our goal was to characterize the late mortality experience of long-term survivors of autologous HCT, thus setting the stage for further interventions to decrease late deaths.
This study of 854 2-year or longer autologous HCT survivors shows that the probability of surviving 5 years was 80% and surviving 10 years was 69%. This cohort was at a 13-fold increased risk for experiencing a late death when compared with the general population. However, beyond 10 years of follow-up, the mortality rates approached those of the general population among patients undergoing transplantation for AML or among patients at standard risk for relapse at HCT, irrespective of specific hematologic diagnosis.
In our study, 5-year overall survival rates for the 2-year autologous HCT survivors by diagnosis were as follows: HD, 73%; NHL, 78%; AML, 91.1%; ALL, 68%. A recent report from the American Cancer Society indicated the 5-year overall survival for patients diagnosed at all stages and treated with conventional chemotherapy and radiation to be as follows: HD, 84%; NHL, 56%; and leukemia, 46%.11 However, it is difficult to compare these rates with patients in our study, first because patients undergoing autologous HCT are selected because of the presence of poor prognostic factors or refractory disease and, second, our study consists of patients who had survived at least 2 years after HCT before entry into the cohort.
Twenty-nine percent of the patients in the current study experienced a late death. Fifty-six percent of these late deaths were due to relapse of the primary disease, accounting for most of the late mortality among those undergoing transplantation for AML, ALL, NHL, and HD. Subsequent malignant neoplasms were the most frequent cause of nonrelapse-related death. Compared with the general population, the cohort was at a 12-fold increased risk for late deaths due to second malignant neoplasms. The incidence of subsequent malignant neoplasms after HCT is known to be significantly higher than that of the cancer incidence rate in the general population and is related largely to the use of radiation and chemotherapy.12-19 Reports in the literature have focused on the increased risk of therapy-related myelodysplasia and acute myeloid leukemia (t-MDS/t-AML) in survivors of autologous HCT for HD and NHL.16,17,20-26 Although most deaths from subsequent malignancies were due to t-MDS/AML, extended follow-up of this cohort has demonstrated increasing mortality from nonhematologic second cancers.
Patients with a primary diagnosis of NHL, HD, and ALL were at an increased risk for relapse-related late death, as were those patients who were at a high risk for relapse at HCT, suggesting a need for better therapeutic options for these patients. On the other hand, total body irradiation was associated with a significantly reduced risk of relapse-related late mortality.
Nonrelapse-related late mortality was increased among patients conditioned with carmustine, an observation probably related to the risk of carmustine-related pulmonary complications. Pulmonary toxicity among HCT survivors has been well documented.27-29 Therapeutic agents implicated include carmustine, total body irradiation, busulfan, and cyclophosphamide.30-37 Carmustine has been included in preparative regimens for HD and NHL.2 Toxic pulmonary reactions, including chronic interstitial fibrosis and decrease in lung diffusing capacity, have been recognized in 16% to 64% of patients exposed to carmustine in combination with a variety of other agents.30-37 Toxicity related to the use of carmustine is dose dependent and is suspected to be caused by damage to the glutathione system.38 In the current study, late pulmonary complications were associated with significantly increased late mortality, and carmustine was identified as a risk factor for nonrelapse-related late mortality. Exposure to chemotherapy and radiation prior to HCT could potentially have contributed to the pulmonary toxicity in this population and was not evaluated in this analysis.
The risk of nonrelapse mortality was also increased among patients receiving peripheral blood stem cells as compared with those receiving an autograft from their marrow. The excess risk of nonrelapse mortality among patients receiving peripheral blood stem cells was largely contributed by deaths due to t-MDS/AML. A higher risk of t-MDS/AML has been demonstrated among recipients of CD34-enriched cells isolated from peripheral blood after chemotherapy priming and growth factors, as compared with autologous transplantation using CD34+ cells from the bone marrow without pretreatment.15,39 Potential explanations offered for this observation include harvesting of hematopoietic precursor cells damaged by chemotherapy at a time before they have completed DNA repair or an overrepresentation of damaged cells in the mobilized product.
The risk of late death due to cardiac complications was 4-fold higher among female survivors of autologous HCT when compared with an age- and sex-matched cohort from the general population. Cardiac complications may result from high-dose chemotherapy or irradiation administered during conditioning40 or could result from pre-HCT administration of anthracyclines.41 Furthermore, female survivors of childhood cancer have been reported to be at a higher risk for doxorubicin-related cardiotoxicity.42 Information regarding exposure to anthracyclines prior to transplantation was not available in the current cohort.
An assessment of long-term survival after autologous HCT must take into consideration the quality of the survivor's life. Although there are some reports describing survival, clinical performance, and social reintegration of patients undergoing allogeneic HCT,8,44 there are no reports describing specific aspects of functional well-being such as marital status, employment, and problems with health and life insurance experienced by long-term survivors of autologous HCT. The current study revealed that approximately two thirds of the adult cohort was currently married, and this marital rate did not differ significantly from that of the sibling comparison group.
A previous study of 5-year or longer survivors of allogeneic transplantations had shown that 11% of the survivors were unable to return to full- or part-time work or school.43 In the current study, 15% of the survivors report that health problems keep them from holding a job or attending school, a significantly higher proportion than that reported by the siblings.
Previous investigations of the insurance coverage of survivors of childhood cancer found clear evidence of discrimination, particularly in employment-related health insurance.44-46 More recent studies of older survivors treated according to contemporary protocols indicate improved access to insurance,45,46 probably because of public awareness of the improved prognosis and because of legislation prohibiting discrimination and promoting insurance portability.47,48 Our data indicate that although the rate of health insurance coverage for long-term survivors of autologous HCT is similar to that of the sibling group, a significantly higher proportion of survivors report difficulty in obtaining health and life insurance. Furthermore, life insurance coverage is significantly lower among HCT survivors when compared with the siblings, although it is difficult to attribute this purely to the transplantation procedure itself, because the difficulty with life insurance could be attributed to the underlying history of cancer for which transplantation was used as a treatment modality.
This study describes the late mortality experience of a large cohort of patients who underwent autologous HCT and survived at least 2 years after transplantation. This study differs from previous reports on late deaths after HCT in several respects. There have been no reports in the literature describing the late mortality experience in a large cohort of patients followed for an extended time after autologous HCT. Furthermore, this study used the services offered by the National Death Index and Social Security Death Registry in addition to the medical records to obtain a complete and comprehensive record of the deaths experienced by this cohort. The NDI is a central, computerized index of death record information submitted under contractual agreement to the National Center for Health Statistics by the state vital statistics offices. The Social Security Administration Death master file is a database containing death notices for enrollees in the US Social Security program. Using resources such as the National Death Index and the Social Security Administration Death master file in addition to medical records represents strengths of this study, because they allow for a near-complete ascertainment of follow-up of this cohort and have enhanced the accuracy of information for determination of mortality status in the current study.49 Although most late deaths were due to primary disease, this study demonstrates that with follow-up beyond 10 years from HCT, the mortality rates normalize to that of the general population among individuals with a primary diagnosis of AML and among individuals from all diagnoses who were at a standard risk for relapse at HCT. Assessment of specific aspects of functional well-being such as marital status, employment, and problems with health and life insurance experienced by the long-term survivors of autologous HCT in this study represents an important contribution, albeit incomplete, to the obstacles faced by long-term survivors of autologous HCT. This study begins to identify some of the areas that could benefit from intervention strategies, potentially resulting in improvement in certain aspects of quality of life.
Prepublished online as Blood First Edition Paper, February 8, 2005; DOI 10.1182/blood-2005-01-0035.
Supported in part by R01 CA078938 from the National Cancer Institute and by The Lymphoma-Leukemia Society of America Clinical Scholar Award 2191-02.
All authors participated in the design of the study as well as the interpretation of the results.
An Inside Blood analysis of this article appears in the front of this issue.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 U.S.C. section 1734.