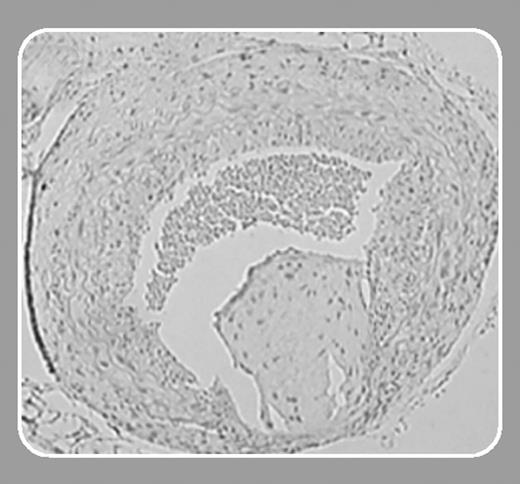
Elevated plasma levels of fibrinogen are strongly associated with human vascular disease. The Northwick Park Heart Study, which prospectively followed more than 1500 men for a mean of 10 years, found that elevated plasma fibrinogen at recruitment was independently associated with subsequent cardiovascular risk, with an increase in baseline plasma fibrinogen of approximately 0.7 g/L (70 mg/dL) being associated with a 39% increase in cardiac death and a 60% increase in nonfatal myocardial infarction.1 However, it is unknown whether elevated plasma fibrinogen plays a causal role in vascular disease progression. On the one hand, elevated plasma fibrinogen may promote vascular disease by increasing blood viscosity, by promoting fibrin formation, by enhancing platelet-platelet interactions, or by other mechanisms. On the other hand, elevated plasma fibrinogen could simply be a marker of vascular disease that in itself does not contribute to disease progression. For example, it is possible that elevated plasma fibrinogen could result from the chronic inflammation that characterizes atherosclerosis. Kerlin and colleagues (page 1728) have examined this important issue by studying thrombosis and vascular disease progression in transgenic mice that carry an extra copy of the murine fibrinogen locus. These Hifib mice have modest (approximately 2-fold) elevations of plasma fibrinogen yet no evidence of underlying inflammation.2 The authors demonstrate that Hifib mice exhibit enhanced fibrin formation under basal conditions, as evidenced by elevated plasma D-dimer levels. In addition, they show that Hifib mice that also carry a loss-of-function mutation in the thrombomodulin gene (TMPro) exhibit enhanced fibrin deposition in the liver compared with wild-type mice or animals with isolated hyperfibrinogenemia or thrombomodulin deficiency. These studies demonstrate that a modest increase in fibrinogen expression can promote fibrin formation in vivo and that the impact of elevated plasma fibrinogen on fibrin deposition within different vascular beds may depend on modifier genes that regulate fibrinogen metabolism.FIG1
Does elevated plasma fibrinogen cause vascular disease? Kerlin et al show that hyperfibrinogenemia alters vascular remodeling induced by ligation of the carotid artery, producing augmented intimal hyperplasia compared with wild-type controls. However, when one considers mechanistic links between hyperfibrinogenemia and coronary heart disease, potential effects on thrombus formation and atherogenesis usually top the list. Interestingly, Kerlin et al found no significant effect of hyperfibrinogenemia on platelet-dependent thrombus formation after carotid artery injury, and previous studies have shown that hyperfibrinogenemia does not accelerate atherogenesis in hyperlipidemic mice.3,4 Therefore, the studies by Kerlin and colleagues are important in that they demonstrate that modest elevations of plasma fibrinogen can alter fibrin formation and modify how blood vessels remodel. A piece of the “cause-and-effect” puzzle has been answered. However, it is still unclear whether modest hyperfibrinogenemia contributes to the development of atherothrombotic diseases—in particular, coronary heart disease and myocardial infarction. Further studies are necessary to resolve this important question.