Abstract
In the present study the clinicopathologic and immunophenotypic features of 82 patients with a CD30– peripheral T-cell lymphoma, unspecified, presenting in the skin were evaluated. The purpose of this study was to find out whether subdivision of these lymphomas on the basis of cell size, phenotype, or presentation with only skin lesions is clinically relevant. The study group included 46 primary cutaneous CD30– large cell lymphomas and 17 small/medium-sized T-cell lymphomas as well as 17 peripheral T-cell lymphomas with both skin and extracutaneous disease at the time of diagnosis. Patients with primary cutaneous small- or medium-sized T-cell lymphomas had a significantly better prognosis (5-year-overall survival, 45%) than patients with primary cutaneous CD30– large T-cell lymphomas (12%) and patients presenting with concurrent extracutaneous disease (12%). The favorable prognosis in this group with primary cutaneous small- or medium-sized T-cell lymphomas was particularly found in patients presenting with localized skin lesions expressing a CD3+CD4+CD8– phenotype. In the primary cutaneous T-cell lymphoma (CTCL) group and in the concurrent group, neither extent of skin lesions nor phenotype had any effect on survival. Our results indicate that peripheral T-cell lymphomas, unspecified, presenting in the skin have an unfavorable prognosis, irrespective of the presence or absence of extracutaneous disease at the time of diagnosis, cell size, and expression of a CD4+ or CD8+ phenotype. The only exception was a group of primary cutaneous small- or medium-sized pleomorphic CTCLs with a CD3+CD4+CD8– phenotype and presenting with localized skin lesions.
Introduction
Mature or peripheral T-cell or natural killer (NK) cell lymphomas are uncommon, accounting for approximately 12% of all non-Hodgkin lymphomas in the Western world.1 These peripheral T/NK-cell lymphomas frequently involve the skin, either as primary or as secondary manifestation of the disease. With respect to the primary cutaneous T-cell lymphomas (CTCLs), both in the European Organization for Research and Treatment of Cancer (EORTC) classification for primary cutaneous lymphoma2 and in the World Health Organization (WHO) classification,3 mycosis fungoides (MF), Sézary syndrome (SS), the group of the primary cutaneous CD30+ lymphoproliferations, and subcutaneous panniculitis-like T-cell lymphomas are recognized as distinct well-defined entities, which together constitute approximately 85% of all primary CTCLs.2 In the EORTC classification most cases of primary CTCL that do not belong to one of these entities are included in the group of CD30– large-cell CTCLs and in the provisional group of CD30– small/medium-sized pleomorphic CTCLs. Distinction between the 2 categories, which is based on the presence of more or less than 30% large neoplastic T cells, is considered useful because of a significant difference in survival between the groups.4,5 The EORTC classification does not include cases presenting with prior or concurrent extracutaneous disease, and it does not make further distinction between cases with a CD4+ T-cell phenotype and those with a CD8+ T-cell phenotype, although recent studies have suggested that epidermotropic CD8+ CTCL with a cytotoxic phenotype should be considered as a distinct disease entity.6 In the WHO classification most of these CD30– large-cell and small/medium-sized pleomorphic CTCLs are classified as peripheral T-cell lymphomas (PTLs), unspecified, and rare cases as extranodal T/NK-cell lymphoma, nasal type. In the group of PTLs, unspecified, no further subdivision is made by site of presentation (eg, distinction between primary and secondary cutaneous involvement), cell size, or phenotype.
In ongoing attempts to evaluate the clinical usefulness of the EORTC and WHO classifications, we evaluated the clinicopathologic features of 82 patients with PTL, unspecified, presenting in the skin. The primary goal of this study was to find out whether subdivision of these lymphomas on the basis of cell size, phenotype, or presentation with or without concurrent extracutaneous involvement is clinically and prognostically relevant.
Patients and methods
Patient selection
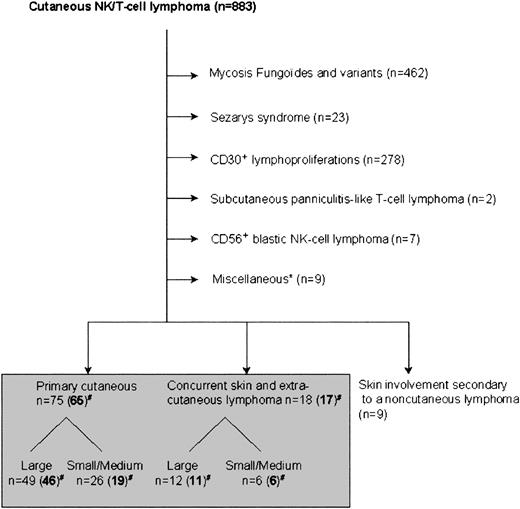
Between October 1985 and December 1999, a total of 883 patients with skin manifestations of a T/NK-cell lymphoma were included in the registry of the Dutch Cutaneous Lymphoma Group (Figure 1). For this study 3 groups of patients were selected for further evaluation: patients with primary cutaneous CD30– large T-cell lymphoma (n = 49), patients with primary cutaneous CD30– small/medium-sized pleomorphic CTCL (n = 26), and a group of 18 patients with both cutaneous and extracutaneous involvement of a CD30– T-cell lymphoma at the time of first diagnosis. Nine patients with history of a primarily noncutaneous T/NK-cell lymphoma—including 5 patients with a nasal T/NK-cell lymphoma, 3 with an angioimmunoblastic T-cell lymphoma (AITL), and 1 with a nodal PTL, unspecified—who developed specific skin lesions during follow-up were not included in this study.
Patients with cutaneous T/NK-cell lymphomas included in the registry of the Dutch Cutaneous Lymphoma Group between October 1985 and December 2000. *“Miscellaneous” includes patients with T-cell leukemia (n = 4), HIV-related CTCL (n = 2), adult T-cell lymphoma/leukemia (n = 2), and T-lymphoblastic lymphoma (n = 1). #Numbers in parentheses denote number of patients included in this study.
Patients with cutaneous T/NK-cell lymphomas included in the registry of the Dutch Cutaneous Lymphoma Group between October 1985 and December 2000. *“Miscellaneous” includes patients with T-cell leukemia (n = 4), HIV-related CTCL (n = 2), adult T-cell lymphoma/leukemia (n = 2), and T-lymphoblastic lymphoma (n = 1). #Numbers in parentheses denote number of patients included in this study.
The 2 groups of primary CTCLs were defined according to the criteria of the EORTC classification.2 In all cases adequate staging procedures, including physical examination, complete blood cell counts, computed tomography of chest and abdomen, and a bone marrow biopsy, had failed to demonstrate extracutaneous disease at time of diagnosis. The third group of patients, who also presented with skin lesions but after staging appeared to have also extracutaneous disease at the time of first diagnosis, was included to find out whether patients presenting with skin-limited disease had a better prognosis. These cases do not represent primary CTCLs and are not included in the EORTC classification. Following the criteria of the WHO classification, all 93 patients were classified as having PTL, unspecified.3
In all cases the clinical records and the results of routine histology and immunostaining performed at diagnosis were reviewed. In cases in which the original paraffin blocks were available, additional staining was performed using antibodies against CD3ϵ, CD4, CD8, CD20, CD79a, CD30, CD56, CD68, TIA-1, and granzyme B, if not performed previously.
Biopsy samples of all cases were re-evaluated at a multiheaded microscope by 3 expert (dermato)pathologists (C.J.L.M.M., P.M.K., R.W.) and a consensus diagnosis was reached.
From the initial study group of 93 cases, 11 cases were excluded: 2 patients because of insufficient follow-up data, 3 patients with unavailable or uninterpretable histology, and 6 patients in whom after thorough clinical and histologic review a diagnosis of MF was considered more likely. The final study group consisted of 82 cases.
In all cases the diagnosis of T-cell lymphoma was based on demonstration of mature, although often incomplete, T-cell phenotype, including expression of surface CD3 (sCD3) as assessed by a positive membrane staining with monoclonal antibody Leu-4 on frozen sections in all but 7 cases. Staining for CD30 antigen was completely negative in most cases, expressed by few (< 5%) scattered neoplastic cells in some cases, and weakly expressed by approximately 25% of the neoplastic T cells in one case.
Statistical analysis
Variables analyzed for prognostic value were as follows: age at diagnosis; sex; extent of skin lesions at presentation (ie, single or localized [a solitary or multiple skin lesions restricted to one anatomic region] vs “multifocal” [2 or more anatomic regions involved]); the presence of extracutaneous disease at the time of diagnosis; occurrence of spontaneous resolution; type of therapy (multiagent chemotherapy vs radiotherapy vs monoagent chemotherapy vs no or only palliative skin-directed therapies such as psoralen and ultraviolet A [PUVA], topical steroids, and excision); tumor cell size (more vs less than 30% large neoplastic T cells); and phenotype (CD3+CD4+CD8– phenotype vs CD3+CD4–CD8+ phenotype vs CD3+CD4–CD8– phenotype vs CD3+CD4+CD8+ phenotype). Disease-free survival (DFS) was calculated as the time of relapse or disease-related death after reaching a complete remission. Cases that did not reach remission were excluded; patients without a relapse or death unrelated to lymphoma were censored. Survival duration was calculated from time of diagnosis to date of death or censoring. Overall survival was estimated using the method of Kaplan and Meier.7 For overall survival analysis, deaths were taken into account whatever the cause. Prognostic factors in the entire group were evaluated by overall survival univariate and multivariate analyses using a Cox proportional hazards model. Factors significant at the .1 level in univariate analysis were included in a stepwise regression multivariate analysis. Comparisons between different subgroups of patients were performed using the χ2 of Fisher exact test for categorical variables (cross-table) or the Mann-Whitney test for continuous variables and log rank for survival data. For statistical analysis the software package for social sciences (SPSS 10.0; SPSS, Chicago, IL) was used.
Results
Characteristics of the total group of 82 patients with PTL, unspecified
Clinical features. The clinical characteristics and follow-up data of the total group of 82 patients are summarized in Table 1. The total group included 50 males and 32 females (male-female ratio, 1.6:1), with a median age of 68 years (range, 8-87 years). The duration of skin lesions prior to diagnosis varied between 1 and 100 months, but was usually short (median, 6 months). Most patients presented with nodular or tumorous skin lesions, which were either solitary (21 of 82 [26%]), localized (11 of 82 [13%]), or multifocal (50 of 82 [61%]). Partial (n = 10) or even complete {n = 3) spontaneous disappearance of skin lesions had been noted in 13 of the 82 patients.
Initial therapy was variable, but consisted in most cases of doxorubicin-based systemic chemotherapy, radiotherapy, or a combination of both. In general, radiotherapy was the first choice of treatment in patients presenting with only localized skin lesions, whereas patients presenting with multifocal skin lesions or with concurrent cutaneous and extracutaneous disease were treated with doxorubicin-based chemotherapy with or without additional radiotherapy. Complete remission was achieved in 22 (71%) of 31 patients treated with radiotherapy and in 10 (28%) of 36 patients treated with doxorubicin-based chemotherapy. However, complete remissions were generally short-lived. The median DFS for complete responders was only 8 months (95% confidence interval [CI], 2-14 months). No correlation between initial type of treatment and clinical outcome was detected.
After a median follow-up of 19 months (range, 1-179 months) 60 patients (73%) had died of lymphoma and 9 (11%) had died of unrelated disease, whereas only 13 patients were alive, with (n = 1) or without (n = 12) lymphoma. The overall 5-year survival was 20% (Table 1).
Histologic features. Histologically, these lymphomas showed considerable variation. On the basis of the cytomorphology of the neoplastic cells, most cases would have been classified as pleomorphic T-cell lymphoma in the updated Kiel classification.8 A minority showed a monotonous proliferation of blast cells with the appearance of immunoblasts, in 2 cases even resembling large anaplastic T cells, but with negative CD30 staining in repetitive stainings. Based on the presence of more or less than 30% large cells within the tumor population, 57 cases were classified as large-cell and 25 cases as small- or medium-sized-cell lymphoma. There was a variable admixture with small lymphocytes and histiocytes, and less commonly with eosinophils and plasma cells. Considerable numbers of admixed B cells (5%-10%) were observed in 6 biopsies.
With respect to the architecture of the neoplastic infiltrates, these were either diffuse (49%), nodular (33%), or band-like (18%). Pronounced epidermotropism was observed in 27% of cases, with no significant differences between the different subgroups. In 3 cases there was extensive infiltration of the follicular epithelium. Angiocentricity with marked angiodestruction was observed in 8 cases; 5 of these 8 cases belonged to the group of primary cutaneous small/medium-sized pleomorphic T-cell lymphomas.
Immunophenotype. The phenotypes of the neoplastic T cells in all 82 cases are summarized in Table 2. A CD3+/CD4+/CD8– phenotype was observed in 59 cases, a CD3+/CD4–/CD8+ phenotype in 12 cases, a CD3+/CD4–/CD8– phenotype in 9 cases, and a CD3+/CD4+/CD8+ phenotype in 2 cases. Coexpression of CD56 was noted in 3 cases. Expression of TIA-1 by more than 50% of the neoplastic cells was observed in 17 of 55 cases tested, including 5 (13%) of 38 cases with a CD3+/CD4+/CD8– phenotype and 8 (89%) of 9 cases with a CD3+/CD4–/CD8+ phenotype. Granzyme B was always expressed by a minor proportion of the TIA-1+ neoplastic T cells, except for 2 cases with a CD3+/CD4–/CD8+ and a CD3+/CD4–/CD8– phenotype, respectively, showing expression of both TIA-1 and granzyme B by more than 75% of the neoplastic T cells.
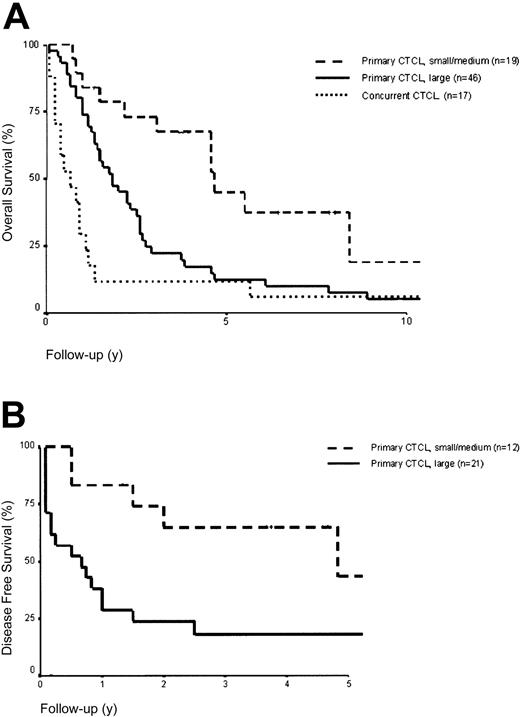
Prognostic factors in the total group of 82 patients. Univariate and multivariate analyses of overall survival were performed on the total group of 82 patients to identify independent prognostic risk factors. Univariate analysis showed that the following variables were adversely related to survival: concurrent extracutaneous disease at diagnosis (P = .0004), large cell size (P = .003), lack of spontaneous resolution (P = .004), age older than 70 years at diagnosis (P = .02), male sex (P = .05), and presentation with multifocal lesions (P = .005). Therapy (P = .19) was not significantly related to survival. Multivariate analysis showed that concurrent extracutaneous disease (relative risk [RR] = 3.5; 95%CI,1.9-6.8), large cell morphology (RR = 3.1; 95%CI, 1.7-5.7), presentation with multifocal lesions (RR = 2.3; 95%CI, 1.4-4.0), age older than 70 years (RR = 2.1; 95%CI, 1.3-3.6), and absence of spontaneous resolution of skin lesions (RR = 2.6; 95%CI, 1.1-5.9) were independent prognostic factors (Table 3). Kaplan-Meier overall survival and DFS curves of different subgroups are shown in Figure 2A and 2B, respectively.
Overall and disease-free survival curves. (A) Overall survival curves of different groups of patients with peripheral T-cell lymphomas presenting in the skin (n = 82). (B) Disease-free survival curves of complete responders with primary cutaneous small-/medium- and large-cell peripheral T-cell lymphomas (n = 33).There were only 3 complete responders in the concurrent group, which is therefore not shown.
Overall and disease-free survival curves. (A) Overall survival curves of different groups of patients with peripheral T-cell lymphomas presenting in the skin (n = 82). (B) Disease-free survival curves of complete responders with primary cutaneous small-/medium- and large-cell peripheral T-cell lymphomas (n = 33).There were only 3 complete responders in the concurrent group, which is therefore not shown.
Subgroup analysis
Since multivariate analysis demonstrated both cell size and the presence of extracutaneous disease at the time of diagnosis as the most significant prognostic parameters, the main features of the group of primary cutaneous CD30– large T-cell lymphomas, the group of primary cutaneous small/medium-sized pleomorphic T-cell lymphomas, and the group of peripheral T-cell lymphomas presenting with both cutaneous and extracutaneous disease will be described below. The main clinical features and the results of phenotyping of these 3 groups are summarized in Tables 1 and 2, respectively.
Primary cutaneous CD30–large T-cell lymphomas (n = 46). This group included 33 males and 13 females (male-female ratio, 2.5:1), with a median age of 68 years (range, 20-87 years). Although most patients presented with multifocal skin lesions (27 of 46 patients [59%]), a significant proportion had either a solitary lesion (15 of 46 patients [33%]) or localized skin lesions (4 of 46 patients [9%]) at presentation, which explains the relatively high number of patients treated with radiotherapy in this group (Table 1).
Following initial treatment, complete remission was achieved in only 21 (45%) of 46 patients, including 12 (63%) of 19 patients treated with radiotherapy and 5 (27%) of 18 patients treated with doxorubicin-based chemotherapy. The median overall survival for patients treated with radiotherapy was 28 months (95% CI, 12-44 months); the DFS for this group was 6 months (95% CI, 0-18 months). For patients treated with systemic chemotherapy, the median overall survival was 16 months (95% CI, 10-22) and DFS was 10 months (95% CI, 0-25 months). With respect to the extent of skin disease, complete remission following initial treatment was observed in 21 of 46 patients, including 13 (86%) of 15 patients with a solitary lesion, but only 1 (25%) of 4 patients with localized lesions and 7 (26%) of 27 patients presenting with multifocal lesions.
However, no difference in overall survival was found between patients with localized disease (median, 24 months; 95% CI, 13-35 months) and patients with multifocal disease (median, 21 months; 95% CI, 13-29 months). In patients presenting with a solitary tumor, radiotherapy (11 cases) and doxorubicin-based chemotherapy (4 cases) showed similar complete response rates (72% vs 75%), median DFS rates (6 months, 95% CI, 10-28 months vs 10 months, 95% CI, 10-24 months), and overall 5-year-survival rates (24% vs 25%). These data illustrate that most patients presenting with solitary or localized skin lesions rapidly developed generalized skin lesions and/or systemic disease. After a median follow-up of 21 months (range, 1-118 months), 42 patients had died (37 patients of lymphoma and 5 of an unrelated disease), whereas only 4 were still alive and in complete remission, 20, 31, 89, and 118 months after diagnosis. One of these 4 patients presented with a solitary nodule on the right shoulder, histologically characterized by the presence of a monotonous proliferation of CD3+CD4+CD8– blast cells with prominent eosinophilic nucleoli, suggesting a CD30+ anaplastic large T-cell lymphoma, but with negative CD30 stainings on 3 different (follow-up) biopsies. Another patient presented with a solitary tumor on the trunk, in which approximately 25% of the CD3+CD4+ large pleomorphic T cells expressed CD30. Both patients had initially been treated with radiotherapy. The other 2 patients had presented with multifocal skin lesions, which had disappeared spontaneously in one of them. Five-year overall survival in this group of 46 patients was 12%.
Statistical analysis showed no significant difference (P = .98) in overall survival between the 34 patients with a CD3+CD4+CD8– phenotype (median survival, 21 months; 95% CI, 11-31 months) and the 6 patients with a CD3+CD4–CD8+ phenotype (median survival, 28 months; 95% CI, 14-42 months; Table 4).
Primary cutaneous small/medium-sized cell CD30–pleomorphic T-cell lymphoma. This group included 6 men and 13 women, with a median age of 69 years (range, 45-87 years). Ten patients presented with multifocal skin lesions, 5 with localized disease, and only 4 with a solitary lesion. In a relatively large proportion of patients (32%), partial (4 cases) or even complete (2 cases) spontaneous clearing of the skin lesions was noted.
Histologically, 5 of 19 patients showed marked angiocentricity and angiodestruction. Previous studies on this group, including 3 cases with a CD4+ phenotype and 2 cases with a CD8+ phenotype, had shown that they were Epstein-Barr virus (EBV)–negative.9 In the whole group, 13 cases (68%) had a CD3+CD4+CD8– phenotype; 4 cases (21%), a CD3+CD4–CD8+ phenotype; and 2 cases (10%), a CD3+CD4–CD8– phenotype (Table 2).
Following initial treatment, 12 (63%) of 19 patients reached a complete remission, including 10 (83%) of 12 treated with radiotherapy and 2 (40%) of 5 patients treated with doxorubicinbased chemotherapy. The median DFS for the complete responders was 58 months (95% CI, 0-120 months). After a median follow-up of 47 months (range, 9-120 months), 8 patients had died of lymphoma, 3 had died of unrelated disease, and 8 were alive with (n = 1) or without (n =7) lymphoma. Overall 5-year survival was 45%. Univariate and multivariate analysis for overall survival showed that patients presenting with localized disease had a better prognosis (P = .03). Overall median survival was significantly better in patients with localized disease (median survival not reached) than in patients presenting with multifocal skin lesions (median survival, 54 months; 95% CI, 22-88 months). Patients with a CD4+ phenotype tended to have a better prognosis, but this was only borderline statistically significant (P = .05). Owing to the small number of patients, the significance of these findings should be considered with caution. Nevertheless, 6 of the 7 patients presenting with solitary or localized skin lesions and having a CD3+/CD4+ phenotype are alive at the time of writing, as compared with 2 of 12 of the remaining cases in this group.
Taken together, patients with a primary cutaneous CD30– small/medium-sized pleomorphic T-cell lymphoma had a much better prognosis than did patients with a primary cutaneous CD30– large T-cell lymphoma. However, this favorable prognosis appears to be restricted to patients with a CD4+ lymphoma with solitary or localized skin lesions.
PTL, unspecified, presenting with both cutaneous and extracutaneous disease. This group contained 6 cases with a predominance of small/medium-sized neoplastic T cells and 11 cases with a predominance of large neoplastic T cells. Statistical analysis did not reveal significant differences between the 2 groups (data not shown). The results for the total group of 17 patients (11 males and 6 females, with a median age of 65 years [range, 8-85 years]) are presented in Table 1. Most (13) of the 17 patients presented with multifocal skin lesions. Concurrent extracutaneous disease at presentation involved lymph nodes (14 cases), bone marrow (2 cases), peripheral blood (2 cases), oropharynx (2 cases), central nervous system (CNS; 1 case), and lung and adrenal glands (1 case).
Initial treatment, which consisted of multiagent chemotherapy in 13 of 17 patients, resulted in a complete remission in only 3 of 17 cases; 8 patients showed a partial response. The prognosis is clearly worse in this group than in the primary cutaneous CD30– groups (P < .0001). After a median follow-up period of 8 months (range, 1-179 months), 15 patients had died of lymphoma and one of unrelated disease, whereas only one patient was still alive after a follow-up of 179 months. The overall 5-year survival was 12%.
Discussion
In the present study, 82 patients with a PTL, unspecified, with skin lesions as first manifestation of the disease were evaluated. The goal of this study was to find independent parameters of survival in this heterogeneous group of lymphomas. More specifically, we wondered if presentation with only skin lesions, the extent of skin lesions, cell size, or the presence of a CD4+ or CD8+ T-cell phenotype had any effect on survival.
Considering the whole group, these patients appeared to have a poor prognosis, with an overall survival at 5 years of 20%, which is consistent with the results of previous studies.10-12 It was found that primary cutaneous small/medium-sized T-cell lymphomas had a much better prognosis than primary cutaneous CD30– large T-cell lymphomas and patients presenting with both cutaneous and extracutaneous disease. The difference in survival between primary cutaneous large-cell and small/medium-sized-cell lymphomas is consistent with the results of previous studies.4,5 A new finding in the present study was that this favorable prognosis was observed only in cases with a CD3+CD4+CD8– phenotype and presenting with solitary or localized skin lesions. Five of 6 patients in this small subgroup were still alive, compared with 8 of 76 patients who did not belong to this group.
Primary cutaneous CD30– small/medium-sized pleomorphic T-cell lymphoma is a diagnosis by exclusion. Confronted with a CTCL with a neoplastic infiltrate showing a predominance of small- to medium-sized pleomorphic T cells, the clinician should exclude diagnoses of tumor stage MF, SS, lymphomatoid papulosis, subcutaneous panniculitis-like T-cell lymphoma, and pseudo–T-cell lymphoma. Particularly, differentiation from (tumor stage) MF and pseudo–T-cell lymphomas may be difficult, and requires detailed analysis of clinical, histologic, and immunophenotypic data.13-15 In this study, 4 cases originally diagnosed as small/medium-sized pleomorphic CTCL were excluded, since in retrospect a diagnosis of MF was considered more likely. Pseudo–T-cell lymphomas characteristically present with a solitary plaque or nodule. Additional criteria favoring a pseudo–T-cell lymphoma include lack of an aberrant T-cell phenotype, lack of clonality, and a considerable admixture with reactive CD8+ T cells, B cells, and histiocytes.13,14 In a recent EORTC workshop on primary cutaneous small/medium-sized pleomorphic T-cell lymphomas, the large majority of submitted cases concerned patients presenting with a solitary lesion, which also proved to have an excellent prognosis (J. Wechsler, manuscript in preparation).
After exclusion of the small subgroup of CD3+CD4+CD8– small/medium-sized pleomorphic CTCLs with solitary or localized skin lesions, neither presentation with skin-limited disease, cell size, extent of skin lesions at presentation, nor phenotype had any significant effect on survival. All subgroups had a poor prognosis, with a median overall survival of 28 months or less (Table 4).
From a clinical point of view it is important to note that, apart from the group of primary cutaneous small/medium-sized CD4+ T-cell lymphomas, patients presenting with a solitary skin lesion or a few localized skin lesions had no better survival than patients presenting with multifocal skin lesions. In the group of primary cutaneous CD30– large T-cell lymphomas, which comprised 46 of 82 patients, the median overall survival for patients presenting with solitary, localized, or multifocal skin lesions was 24, 12, and 21 months, respectively. These observations illustrate that patients presenting with solitary or localized skin lesions almost without exception rapidly develop widespread disease.
The results of the present study also indicate that current treatment strategies in these PTLs, unspecified, are not effective, which is in agreement with the results of previous studies.10-12 Comparison of the type of treatment between survivors and nonsurvivors did not show major differences. In the group of 13 survivors, which included 9 patients presenting with only solitary or localized skin lesions, 8 patients had been treated with radiotherapy and only 3 with doxorubicin-based chemotherapy. Following the guidelines of the Dutch Cutaneous Lymphoma Group, most patients with only solitary or localized skin lesions at presentation were treated with radiotherapy, whereas patients presenting with multifocal skin lesions or with concurrent cutaneous and extracutaneous disease were generally treated with doxorubicin-based chemotherapy (CHOP [cyclophosphamide, doxorubicin, vincristine, and prednisone] or CHOP-like courses), with additional radiotherapy in some cases. Initial radiotherapy resulted in a complete remission in 22 (71%) of 31 patients. However, these complete remissions were generally short-lived, requiring additional multiagent chemotherapy soon afterward. In general, a beneficial effect of radiotherapy may be expected only in the subgroup of primary cutaneous CD3+/CD4+ small/medium-sized pleomorphic CTCLs presenting with solitary or localized skin lesions. The results of doxorubicin-based chemotherapy were equally disappointing, both in patients presenting with solitary or localized disease and in patients presenting with multifocal skin lesions or with concurrent extracutaneous disease. Complete remission was observed in only 10 (28%) of 36 patients, and the median DFS for complete responders was only 3 months (95% CI, 0-15 months). Recent studies suggest that more intensive regimens are also not effective in these PTLs, unspecified.10,11 Two patients in the present study were treated with intensive chemotherapy followed by autologous bone marrow transplantation, but they also experienced relapses and died of lymphoma (12 and 49 months after transplantation). It is fair to conclude that it is as yet unknown how such patients with a PTL, unspecified, can best be treated. Because of the inefficacy of current standard regimens, new therapies should be investigated in prospective trials.
Prepublished online as Blood First Edition Paper, May 15, 2003; DOI 10.1182/blood-2002-07-1960.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 U.S.C. section 1734.
The authors would like to thank Mrs S. Le Cessie for excellent statistical support.