Enthusiasm for the use of monoclonal antibodies, such as rituximab, has markedly changed the approach to patients with non-Hodgkin lymphomas (NHLs). Nevertheless, more effective therapies are needed. Radioimmunotherapy as a form of targeted radiation therapy may add significantly to our therapeutic options. Yttrium Y 90 ibritumomab tiuxetan, recently approved by the Food and Drug Administration, and iodine I 131 tositumomab have demonstrated a high level of activity in patients whose NHL has failed to respond to chemotherapy and rituximab. Toxicities have primarily included prolonged myelosuppression, with a potential risk of treatment-associated myelodysplastic syndrome and acute myelogenous leukemia. Ongoing clinical trials are attempting to better characterize the role of these promising agents.
Introduction
Treatment paradigms for the non-Hodgkin lymphomas (NHLs) have undergone a monumental change in the past 5 years since the US Food and Drug Administration (FDA) approved the anti-CD20 monoclonal antibody rituximab for the treatment of relapsed and refractory, follicular, low-grade NHL.1 Because of its activity, coupled with a favorable toxicity profile, rituximab has become almost ubiquitous in the treatment of most B-cell malignancies.
However, fewer than half of patients with follicular NHL respond to rituximab, and the median response duration is about a year. Although, on relapse, about 40% of those with a previous response of at least 6 months respond again.2 Mechanisms of resistance to rituximab and other unconjugated antibodies may involve inadequate serum antibody levels, insufficient binding of antibody due to lack of or loss of antigen expression on the lymphoma cells, poor access of antibody to the tumor cells, or failure of host effector mechanisms to eliminate tumor cells despite antibody binding. One potential solution to some of these issues may be afforded by radioimmunoconjugates (RICs), monoclonal antibodies to which a radioisotope is attached. Lymphoma cells are inherently radiosensitive; therefore, RICs may provide a form of targeted radiation therapy, not only to the cells that bind the antibody, but, due to a bystander or crossfire effect, to neighboring cells inaccessible to antibody or with insufficient antigen expression.
Selection of radioisotopes
The selection of the isotope has clinical implications that are at least theoretically important. For example, yttrium 90 (90Y) is a pure β-emitting isotope with the potential to deliver particles that deliver 5 times more energy to the tumor site than iodine 131 (131I; 2.3 MeV versus 0.81 MeV β energy; Table 1), with a path length of 5 mm versus 0.8 mm and a more favorable half-life (T1/2) of 2.5 days compared with 8 days, respectively. The nontumor distribution is primarily to the bone, although there is liver uptake as well. As a pure β emitter, it was necessary to use the surrogate γ emitter, indium 111 (111In) for purposes of dosimetry in the early 90Y RIC trials, and imaging in the later trials. In addition, its longer path length may provide an advantage, particularly for bulkier tumors or those with poor antibody penetration. The β emission characteristics of 131I include a relatively short path length that limits toxicity to normal surrounding tissues. The crossfire from these high-energy β particles kills not only CD20+ cells, but also neighboring tumor cells inaccessible to the antibody or expressing insufficient antigen. Also, dosimetry can be performed with 131I without using a substitute isotope. Nontumor distribution is primarily to the thyroid. The γ emissions of 131I increase the whole body dose and require shielding of hospital personnel and greater restrictions following discharge. Juweid et al,3 using the humanized anti-CD22 hLL2 antibody conjugated to either isotope, found more favorable tumor dosimetry with the 90Y RIC, using111In as the surrogate.
The most widely studied of the current generation of RICs used in patients with NHL are directed against CD20, linked to either131I or 90Y. CD20 provides an excellent target because it is expressed on the surface of most B cells and is neither shed nor internalized on antigen binding. However, the optimal radioisotope remains controversial.
Early studies
Early studies of RICs in NHL explored a variety of antibodies, primarily conjugated to 131I. Press et al4used iodine I 131 anti-CD37 in patients with relapsed and refractory indolent and aggressive NHL. Delayed myelotoxicity was the major adverse effect. Four of 5 patients experienced a complete remission (CR); the single patient who was CD37− attained a partial remission (PR). Kaminski et al noted activity using a similar antibody in 12 patients.5 Nevertheless, this anti-CD37 was abandoned because the marker proved insufficiently specific for B cells, given that T-cell depletion was also observed. Furthermore, it was not good for imaging and not adequately selective in radioactivity biodistribution characteristics to tumors relative to normal tissues, except in some patients with small tumor masses.
DeNardo and coworkers conducted a series of trials with Lym-1, a131I-labeled mouse IgGκ. The antibody recognizes a 31- to 35-kDa antigen presumed to be a polymorphic variant of the HLA-DR antigen, and thought to have a specific avidity for malignant B cells.6-8 Although responses were reported in patients with NHL and chronic lymphocytic leukemia (CLL), the criteria for response were not standard making the data difficult to interpret.9
Other investigators have reported on 131I-labeled OKB7, a murine IgG2b,10 and iodine I 131 LL2 (anti-CD22),11 among other RICs. Activity was noted in preliminary trials in which 90Y was conjugated with anti-idiotype antibodies; however, this approach was not considered practical.12 In a phase 1/2 study in 18 patients treated with a yttrium Y 90 anti-CD20 (tositumomab) RIC, Knox et al13 reported a response rate of 72% including 33% CRs, some of which were durable. Myelosuppression was the dose-limiting toxicity, and doses less than 40 mCi (1480 MBq) were considered effective and nonmyeloablative.
Structure of RICs
The 2 most widely studied of the current generation of RICs are yttrium Y 90 ibritumomab tiuxetan and iodine I 131 tositumomab. Yttrium Y 90 ibritumomab tiuxetan is composed of the murine parent of rituximab, ibritumomab (Y2B8), an IgG1 antibody, with tiuxetan (MX-DTPA), which functions as a bifunctional chelating reagent, forming a strong thiourea covalent bond, with stable retention of the90Y. This chelator binds the 111In for imaging and the 90Y for therapy. Iodine I 131 tositumomab is composed of the murine tositumomab (B-1) antibody, which is an IgG2a specific for CD20 to which 131I is linked by a chemical bond.
Yttrium 90 ibritumomab tiuxetan
The first radioimmunoconjugate to be approved by the FDA for the treatment of relapsed or refractory follicular/low-grade or transformed NHL, including rituximab-refractory follicular NHL, was yttrium Y 90 ibritumomab tiuxetan (IDEC Pharmaceuticals, San Diego, CA). The specific mechanisms of action of this RIC likely include antibody-dependent cellular cytotoxicity (ADCC), complement-mediated cytotoxicity (CDC), and induction of apoptosis.
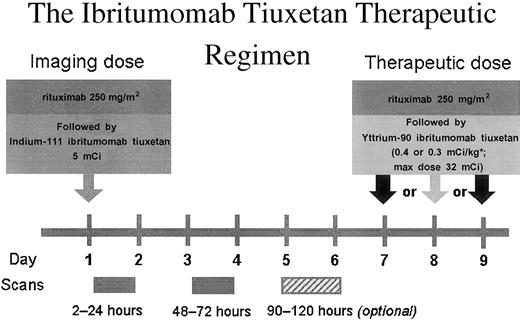
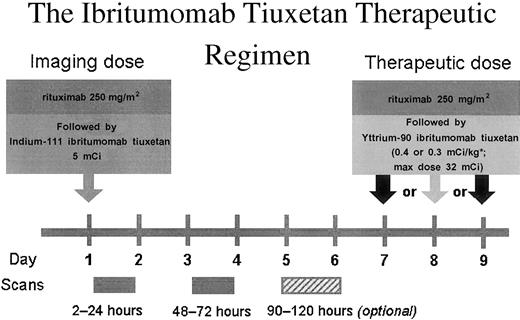
A single course of yttrium Y 90 ibritumomab tiuxetan is administered over about 8 days (Figure 1). On day one an initial unlabeled predose of 250 mg/m2 rituximab is delivered to clear the peripheral blood of B cells and further enable targeting of the radiolabeled isotope to the tumor cells. This predose is followed by an imaging dose of 111In yttrium Y 90 ibritumomab tiuxetan (5 mCi 111In; 185 MBq) because 90Y is a pure β emitter and, therefore, not suitable for imaging.14 Following the imaging dose, whole-body scans to determine favorable biodistribution of the radiolabeled antibody are performed at 2 to 24 hours (day 1), 48 to 72 hours (days 3-4), and (optional) 90 to 120 hours (days 4-5). The therapeutic dose of yttrium Y 90 ibritumomab tiuxetan is delivered on day 8 following another predosing of 250 mg/m2 rituximab. The drug is dosed at 0.4 mCi/m2 (14.8 MBq) for a platelet count of more than 150 000/mm3. The maximum allowable whole-body dose should not exceed 32 mCi (1184 MBq).
Schedule of administration of yttrium Y 90 ibritumomab tiuxetan.
*0.4 mCi/kg in patients with a platelet count of 150 000 or more cells/μL or 0.3 mCi/kg with a platelet count of 100 000 to 149 000 cells/μL. Maximum dose is 32.0 mCi.
Schedule of administration of yttrium Y 90 ibritumomab tiuxetan.
*0.4 mCi/kg in patients with a platelet count of 150 000 or more cells/μL or 0.3 mCi/kg with a platelet count of 100 000 to 149 000 cells/μL. Maximum dose is 32.0 mCi.
Dosimetry has demonstrated an 850-fold greater radiation dose to tumor than normal organs.15 However, dosimetry does not correlate with toxicity or efficacy. Yttrium Y 90 ibritumomab tiuxetan can be dosed on the basis of the patient's weight because the isotope remains bound to the antibody, the half-life of the isotope is short, and the urinary excretion is only 7% ± 3.2% after 7 days. Baseline bone marrow involvement and platelet counts have been shown to be accurate predictors of hematologic toxicity.16 17 Instead, 2 imaging studies to determine favorable biodistribution are currently required to ensure tumor targeting and to ensure that safe doses of radiation are delivered to normal organs.
The current requirement for imaging is neither diagnostic nor therapeutic, but rather a method to demonstrate appropriate biodistribution. Contingent on the results over time, this agent may possibly be used in the future without imaging.
Clinical trials
Because of the potential for myelosuppression, eligibility criteria for clinical trials with this agent specify less than 25% bone marrow involvement in a sample of at least 15% cellularity; for most studies a platelet count of at least 150 000/μL has also been required. In the initial phase 1/2 trial,16 the overall response rate in 32 patients with follicular/low-grade NHL was 82% including 26% CRs (Table 2). In the 14 patients with intermediate-grade NHL, the response rate was 43%, with 29% CRs. There were no responses in 3 patients with mantle cell lymphoma. Response could be predicted by tumor grade, tumor burden, whether or not the bone marrow was involved with lymphoma, and the extent of bone marrow involvement. The median time to progression was 12.9+ months and the response duration 11.7+ months. The major toxicity was myelosuppression, with median granulocyte and platelet nadirs of 1100/mm3 and 49 500/mm3, respectively. Hematologic nadirs with RICs occur later and are typically more protracted than those seen with chemotherapy. In this study, absolute neutrophil nadirs occurred at 50 and 43 days and with an additional 10.5 and 14 days, respectively, to recovery.
Yttrium Y 90 ibritumomab tiuxetan has been compared with rituximab in a randomized, phase 3 multicenter trial including 143 patients with relapsed or refractory low-grade/follicular or transformed NHL who had not received prior rituximab.19 The 2 treatment groups were similar with respect to age, presence of bone marrow involvement, number of prior chemotherapy regimens (median 2), resistance to last chemotherapy, bulky disease (≥ 5 cm), elevated lactic dehydrogenase (LDH) levels, International Prognostic Index (IPI) risk groups, performance status, and extranodal disease. Yttrium Y 90 ibritumomab tiuxetan was significantly more active with an overall response rate of 80% compared with 56% for rituximab (P = .002), 34% complete remission/unconfirmed complete remission (CR/CRu) with the RIC, and 20% with the unconjugated antibody. There was also a high likelihood of becoming polymerase chain reaction–negative for bcl-2.21 However, there was no difference in the response duration (10.9+ for rituximab and 11.5+ months for yttrium Y 90 ibritumomab tiuxetan). Nevertheless, the time to next therapy was not yet reached for yttrium Y 90 ibritumomab tiuxetan, but was 15.2 months for the rituximab control group. However, whether standardized criteria were used for initiating therapy is not clear. Grade 4 thrombocytopenia occurred in 5%. Additional analyses suggested that quality of life was better on the RIC arm.22
This agent is also active in the setting of bulky adenopathy, although the response rate decreases with increasing tumor size.16,23 In the phase 1/2 trial,16 41% of those with lesions 7 cm or larger responded, compared with 86% of those with smaller lesions. In a subsequent nonrandomized study,23 14 of 23 (61%) with lesions 7 cm or larger responded, including half of those with lesions larger than 10 cm. Four of 8 patients with splenomegaly responded, compared with 79% of those without splenomegaly.24 It is also safe and effective in geriatric patients with low-grade/follicular NHL.25
Despite the fact that the drug consists of an anti-CD20 monoclonal antibody, responses can be achieved in patients with follicular/low-grade NHL refractory to rituximab therapy, defined as those not responding to the drug or relapsing within 6 months of its administration.18 The overall response rate in 54 patients was 54% with 15% CRs. The median duration of response of 8.7+ months compared favorably with the 6.5 months following the prior chemotherapy response. The median time to progression had not been reached. The median absolute neutrophil count (ANC) nadir was 700/mm3with platelet counts of 50 000/mm3.
In the phase 1/2 study, the maximum tolerated dose in patients with normal blood counts (including platelet counts > 150 000/mm3) prior to therapy was found to be 0.4 mCi/kg (14.8 MBq), but was 0.3 in patients with mild thrombocytopenia (platelet count 100 000-149 000/mm3).26 A phase 2 study expanded this experience using 0.3 mCi/kg (11.1 MBq) to treat 30 patients with less than 25% bone marrow involvement and a platelet count of 100 000 to 149 000/μL.20 The response rate was 83% including 44% CRs. Grade 4 neutropenia, thrombocytopenia, and anemia were reported for 33%, 13%, and 3% of patients, respectively.
Toxicity
In the aggregate safety data from the phase 1/2 trial,16 the phase 3 study,19 the low-dose phase 2 trial in patients with pretreatment thrombocytopenia,20 and a study of the agent in patients refractory to rituximab,31 toxicities related to yttrium Y 90 ibritumomab were primarily hematologic. Unlike chemotherapy, after which nadir counts occur in about 1 to 2 weeks, the nadir with yttrium Y 90 ibritumomab tiuxetan occurs at about 7 to 9 weeks following therapy (Table 3). Median neutrophil nadirs were 800/mm3, platelet count 37 500/mm3, and hemoglobin level 10.3 g/dL. Grade 4 neutropenia and thrombocytopenia occurred in 32% and 8.5% of patients, respectively. Nevertheless, only 7.6% of patients were hospitalized for infections, few of which were by opportunistic organisms.32 This low rate of infections may be explained in part by relatively normal levels of IgM, T-cell counts, and a rapid recovery of natural killer (NK) cells.33 34 Serum immunoglobulins remained normal despite the profound B-cell depletion. Growth factors were administered to only 17% of patients. Red blood cell transfusions were administered to 18% of patients and platelets to 22%.
The reported frequency of human antimouse antibody or human antichimeric antibody (HAMA/HACA) following yttrium Y 90 ibritumomab is less than 2% with no serious adverse events.35 36
A potential toxicity of concern is secondary malignancies, particularly acute myelogenous leukemia (AML) and treatment-related myelodysplastic syndrome (tMDS), which have been reported in about 1.5% of treated patients at a median follow-up of less than 2 years.37This frequency may increase with longer follow-up. The causal factor for these secondary malignancies remains to be elucidated given that the population receiving yttrium Y 90 ibritumomab tiuxetan was pretreated with alkylating agents with or without external beam irradiation.
The most common nonhematologic toxicities include asthenia, nausea, infection, chills, fever, and abdominal pain. Less often, grades 1 and 2 nausea, vomiting, and abdominal pain have also been recorded.38 Nonhematologic toxicities are transient and easily managed with infrequent need for supportive care.
The limited available data suggest that patients treated with this agent can tolerate subsequent therapies.39 In a retrospective analysis of 58 patients who had a relapse following yttrium Y 90 ibritumomab tiuxetan and went on to subsequent chemotherapy, rituximab, or stem cell transplantation, 16 patients required growth factor support and 2 required chemotherapy dose reductions as a result of prolonged pancytopenia. Thirteen patients required hospitalization for neutropenic fever or thrombocytopenia. The toxicity encountered did not seem to be greater than matched controls at the same institution. Eight patients went on to autologous stem cell transplantation, with some successfully harvested following treatment with yttrium Y 90 ibritumomab tiuxetan. Other investigators also noted that high-dose chemotherapy with stem cell support can be safely delivered following yttrium Y 90 ibritumomab tiuxetan with successful engraftment.40 Anecdotal evidence suggests that patients who relapse after treatment can respond to subsequent rituximab therapy, even if previously resistant to the rituximab.41
Safety
Yttrium Y 90 ibritumomab tiuxetan can be administered in an outpatient setting with minimal risk to health care workers or family members because of the β-particle nature of the isotope, with minimal shielding or protective isolation required.42 Lucite shielding is used during the infusion to block the β emissions. Patients are released immediately after treatment. The only recommendations are to avoid contact with bodily fluids, as would be conducted for universal precautions. Release instructions include cleaning up spilled urine for 3 days during which time any body fluid containing material is disposed of to prevent its being handled. Such material can either be flushed down the toilet or placed in a plastic bag and discarded with the household trash. A condom should be used for the first week during sexual relations.
Iodine I 131 tositumomab
Iodine I 131 tositumomab (Corixa, Seattle, WA; and Glaxo SmithKline, Philadelphia, PA) is composed of an anti-CD20 monoclonal antibody (B1; tositumomab) linked to 131I. Tositumomab is a murine IgG2a anti-CD20 monoclonal antibody that affects cell kill by induction of apoptosis, CDC, and ADCC.43-45
Drug administration
B1 was first developed over 20 years ago46 and was approved by the FDA as an in vitro diagnostic agent in 1982. The radiolabeled antibody (iodine I 131 tositumomab) entered clinical trials in 1990 in both nonablative and ablative forms.
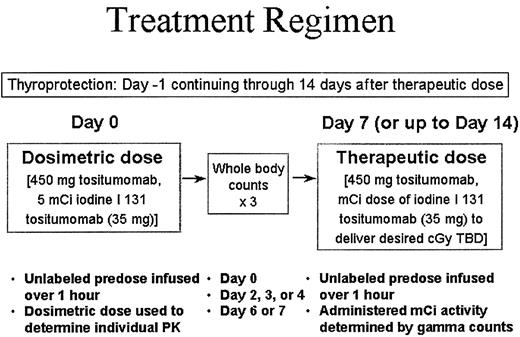
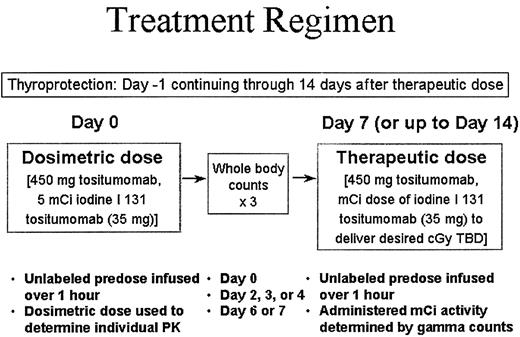
Therapy is administered over a 1- to 2-week period (Figure2). The patient receives oral thyroprotection (saturated solution of potassium iodide [SSKI]; Lugol solution) beginning on day 1 and continuing for 14 days following the therapeutic dose. On day 0 an unlabeled predose of 450 mg tositumomab is delivered over 1 hour to saturate accessible nontumor sites (eg, circulating B cells, splenic B cells) and, thereby, to increase tumor delivery of 131I. This predose is followed by a dosimetric dose of 5 mCi (185 MBq) iodine I 131 tositumomab (35 mg) to determine the whole-body clearance of the RIC. Three whole-body γ counts are obtained on day 0; day 2, 3, or 4; and day 6 or 7. On days 7 to 14 the therapeutic dose is delivered: 450 mg unlabeled tositumomab over 1 hour followed by the patient-specific millicurie dose of iodine I 131 tositumomab (35 mg). Whole-body counting allows for delivery of millicurie activity to achieve the desired total body absorbed centigray (cGy) dose. The desired total body dose (TBD) is 75 cGy for patients with platelet counts greater than or equal to 150 000/mm3, and 65 cGy for platelet levels of 100 000 to 149 000/mm3. The actual 131I activity administered to each patient to achieve the desired TBD varies from 32 to more than 230 mCi (1184-8510 MBq). Most states permit administration of this agent on an outpatient basis.
Phase 1 study
In the phase 1 trial,5 doses of iodine I 131 tositumomab were escalated by 10-cGy increments, beginning at 25 cGy. Increasing the predose of tositumomab from 0 to 95 to 475 mg was associated with a prolongation of the T1/2 of the iodine I 131 tositumomab from 63 to 73 to 85 hours. Increased tumor burden and splenomegaly were both associated with more rapid clearance of the radiolabeled antibody. The 475-mg dose of tositumomab provided superior tumor targeting. The maximum tolerated dose (MTD) of the radiolabeled antibody was 75 cGy in patients with a normal platelet count (> 150 000/mm3) such that the absorbed dose to the bone marrow was approximately 100 cGy, with higher doses resulting in unacceptable myelosuppression. The MTD was 65 cGy in those with a platelet count between 100 000 and 149 000/mm3.
Phase 2 studies
Because of the potential for prolonged myelosuppression, patient eligibility for clinical trials with all RICs has required less than 25% bone marrow involvement. In 1993, Kaminski and coworkers published the first efficacy data,47 which was updated in 1996,48 including 53 patients with follicular/low-grade or transformed NHL in whom prior chemotherapy had failed49(Table 4). The overall response rate to iodine I 131 tositumomab of 71% including 34% CRs was higher (83%) in de novo low-grade or transformed NHL than in de novo large cell NHL (41%). The median progression-free survival for responders was 12 months and 20.3 months for the complete responders. Of 16 patients who were retreated after relapse following iodine I 131 tositumomab therapy, 9 responded, including 5 CRs, with a median progression-free survival of 11.4 months. Five patients developed MDS between 1.2 to 7.5 years after treatment. All had received previous alkylating agents, with cytogenetic abnormalities suggesting that the MDS was secondary to prior treatment. Of interest was a 62% response rate in small lymphocytic lymphoma, with 21% CRs.50
Vose et al51 reported the first multicenter trial including 47 patients. The response rate was 57% (32% CR) with a low-grade histology and 60% (CR 50%) with transformed NHL. The median duration of response and CR were 9.9 months and 20 months, respectively.
Leonard et al56 reported the overall multicenter experience in 269 patients, 25% of whom were previously untreated. The bone marrow was involved in about half the patients, and almost one third had bulky disease. The CR rate of 33%, and the median duration of CR of 5 years, correlated with extent of and responsiveness to prior treatment; 58% CR (44% confirmed) as front-line therapy, and 29% and 22% for 1 to 3 and 4 or more prior regimens, respectively.
The multicenter pivotal trial52 included 60 patients with low-grade or transformed indolent NHL who failed at least 2 prior chemotherapy regimens (rituximab was not allowed to be a prior regimen), had relapsed within 6 months of completing that therapy, or were resistant to that regimen. Those with transformed NHL had to have received a regimen for aggressive NHL. All patients were required to have an ANC of 1500/mm3 and platelet levels of at least 100 000/mm3.
Almost all (98%) patients had stage III or IV disease and 56% had bone marrow involvement. They had received a median of 4 prior regimens (range, 2-13). Sixty percent of the patients had low-grade histology, 38% had transformed to an aggressive histology, and 1 patient (1.8%) was found to have mantle cell NHL on subsequent pathology review. Sixty-five percent had a tumor of at least 5 cm and 88% had at least 2 risk factors from the IPI.57
Responses were reported in 65% (81% in those with a low-grade histology, including 20% CRs). Response rates correlated with histology, tumor burden, prior radiotherapy, and the number of prior therapies. The patients' best response to their previous therapy had been a CR in 3%, PR 25%, stable disease (SD) 38%, and progression in 33%. In 74% of the patients, the duration was longer with iodine I 131 tositumomab (53%); in 28% the duration of response to their last chemotherapy was equivalent to that with iodine I 131 tositumomab; and in 26% there was a longer response to their last therapy. The median duration of response with iodine I 131 tositumomab of 6.5 months was also significantly longer than that of the last qualifying therapy (3.4 months), and the median duration of response for the complete responders has not been reached at a median follow-up of 47 months or longer, compared with 6.1 months for the patients' last therapy.52
A large, multicenter expanded access program providing drug to patients prior to its eventual commercial availability demonstrated that iodine I 131 tositumomab is effective and safe in community and academic settings.54 58
Iodine I 131 tositumomab is also active in patients who fail to respond or relapse within 6 months of receiving rituximab. Horning et al53 treated 38 such patients with iodine I 131 tositumomab. The overall response rate was 57% with 14% CRs, lasting a median of 16 months. The median time to progression for all patients and for responding patients was 6 months and 19 months, respectively. The median neutrophil nadir was 1200/mm3 and that for platelet counts was 90 000/mm3.
When used as initial treatment in 76 patients with follicular NHL,59 the response rate was 97% including a CR rate of 63%. The median duration of response had not been reached as of the publication.
Press and coworkers61 used myeloablative doses of131I anti-CD20 antibody either alone or in combination with chemotherapy.60 The progression-free survival was longer than with the patients' longest previous remission or from their last chemotherapy.60 Results in a subsequent phase 1/2 study of iodine I 131 tositumomab with etoposide and cyclophosphamide61 compared favorably with historical patients who received conditioning with total body irradiation and similar chemotherapy. This combined- modality approach has the potential to replace total body irradiation–based transplantation regimens.
Toxicity
Infusions of tositumomab are well tolerated, with only 4% of patients requiring a rate decrease because of an infusion reaction.51 The most common, nonhematologic adverse events are grade 1/2 asthenia (39%), fever and nausea (both 35% grade 1/2; 2% grade 3/4), and headache (21%, with < 1% grade 3/4). Chills, myalgias, anorexia, arthralgia, rash, and pruritus occur with a frequency of less than 20% (grades 1 and 2). Despite thyroid protection, an elevated thyroid-stimulating hormone level (TSH) occurs in 8.5%. However, in early series, baseline thyroid function was not obtained to identify underlying hypothyroidism.
The major toxicities of iodine I 131 tositumomab are mild to moderate, transient neutropenia, thrombocytopenia, and anemia. Nadir counts typically occur from 4 to 6 weeks after therapy with recovery to grade 2 by weeks 8 to 9 following the therapeutic dose. Grade 4 neutropenia occurs in 17%, thrombocytopenia in 3%, and anemia in 2%, with a median neutrophil nadir of 1100/mm3, platelet count 63 000/mm3, and hemoglobin level 11 g/dL. In this series, 12% of patients received platelet transfusions and 10% red blood cell transfusions. Myeloid growth factors or erythropoietin were given to 12% of patients. Some patients required more than one supportive measure.
Potential adverse events of real concern is AML and tMDS, which has been reported to occur in up to 6.3% of patients.49,52With additional patients and a median 3.2 years, the annualized incidence was 3.8%/y.62 The observation that there were no such events in patients receiving iodine I 131 tositumomab as their initial therapy lends support to the contribution of prior chemotherapy to this complication.
In patients who are treated with iodine I 131 tositumomab after receiving prior chemotherapy, the risk of HAMA is approximately 9%, whereas it has been reported to be 65% when the antibody is given as first-line treatment.59 This reaction may be associated with a flulike syndrome, but it does not appear to interfere with response to subsequent rituximab.63 Pretreatment with an immunosuppressive agent such as fludarabine can virtually eliminate the formation of HAMA.64
Patients in whom iodine I 131 tositumomab has failed can tolerate subsequent treatments.65,66 Kaminski et al66reported data on 76 patients who had received iodine I 131 tositumomab as their initial treatment for follicular NHL. Of the 22 who received subsequent therapy with at least one chemotherapy regimen, rituximab-based therapy, or stem cell transplantation, one patient required therapy to be discontinued because of cytopenias. Ratanatharathorn et al67 described 12 patients who underwent autologous or allogeneic stem cell transplantation after therapy with iodine I 131 tositumomab. All 5 patients who underwent autologous transplantation had a relapse and died, as did 1 of the patients receiving an allograft. Another patient died from a treatment-related cause. Thus, only 5 patients are alive, 4 without evidence of disease, and with short follow-up. This study demonstrates that transplantation may be complicated in heavily pretreated patients.
Safety
Release of patients from the hospital following iodine I 131 tositumomab therapy must be in compliance with state and federal regulations, notably those of the Nuclear Regulatory Commission. Patients can be released as long as the radiation dose to family members or other contacts is less than 500 mrem. Patient-specific release criteria are determined by total body residence time of the antibody based on the dosimetry and the measured dose rate at 1 m.68
Patients must be instructed about disposing of body wastes and interacting with others. Patients must sleep at least 6 feet from their partner and not sit near others for 4 or more hours, such as in a car or airplane. Contact with children or pregnant women should be avoided. The duration of these guidelines is generally around 7 days. This practice has been shown to be both safe and feasible with adequate patient, caregiver, and health care provider education related to radiation safety.
Other RICs
Other lymphoma-specific RICs being investigated include humanized LL2 anti-CD22, conjugated to either 131I or111In/90Y3,69 (Table5). Juweid et al3reported responses in 2 of 13 and 2 of 7 patients, respectively, with myelosuppression being the dose-limiting toxicity. Linden et al69 observed 3 partial responses in 9 patients on the study.
Lym-1 has been bound to 90Y70 and67Cu.71,72 Pharmacokinetic and dosimetry data appear to favor the 67Cu RIC.73 The latter was used to treat 12 patients with NHL, 7 of whom responded. The only significant adverse event was dose-limiting hematologic toxicity. Earlier in development are astatine, an α emitter that has been linked to rituximab and has shown in vitro activity against NHL cells,74 and 90Y-labeled anti-CD19, which showed activity comparable to the anti-CD20 conjugate in a lymphoma xenograft model.75
Discussion
RICs represent an important addition to the therapeutic armamentarium for patients with lymphoid malignancies. Yttrium Y 90 ibritumomab tiuxetan has recently become commercially available and wider use will bring familiarity with the product. After lengthy discussions with the FDA over the past few years, iodine I 131 tositumomba will finally be presented to the Oncologic Drug Advisory Committee to the FDA on December 17, 2002.
A number of clinical trials are focused on optimizing strategies for incorporating RICs into the treatment of patients with NHL. Currently, yttrium Y 90 ibritumomab tiuxetan is approved for use in relapsed or refractory follicular, low-grade, or transformed NHL, and in patients in whom rituximab therapy fails. In general, RICs should be used in patients in whom chemotherapy and rituximab have failed. For some patients who have had an initial, durable response to rituximab, a second course of that unconjugated antibody may induce a meaningful response.77 Whether it is advantageous to use an RIC as part of initial treatment or to reserve it for a salvage option is under investigation. Response rates with RICs inversely correlate with the extent of prior therapy, whereas the likelihood of toxicity increases, notably MDS.56 However, use of an RIC as initial therapy is currently investigational because of the potential adverse effects and a lack of data demonstrating prolongation of survival.
When physicians are eventually faced with how to decide among multiple RICs, one leading criterion in that determination will be the overall activity response rate and duration of response. Yet, the activity of an RIC may vary with specific indications; for example, the longer path length of 90Y may be preferable to 131I for bulky disease, whereas the lack of affinity of 131I to bone may induce less pronounced hematologic toxicity. Comparisons of results of RICs may be confounded by differences in patient features, including the type and amount of prior therapy and response to that therapy, and differences in response criteria.78 Another factor may be which RIC induces the least myelosuppression or lowest risk of secondary malignancies. One critical deciding factor may be which agent is the most convenient and cost-effective. Validating clinical utility and safety outside of well-controlled trials is key to the overall success of this new class of drugs.
However, direct comparisons of currently available RICs are of limited interest because the number of patients required to detect a meaningful difference in efficacy would be prohibitively large and may be more prominent in subsets of patients. Detecting important differences in toxicities would also be difficult. Both ibritumomab tiuxetan and tositumomab are associated with substantial grades 3 and 4 myelosuppression, but these occurrences are not as clinically relevant as are the risk of infections, and requirements for blood component or growth factor support, which are relatively low for both agents.
Attempts to optimize the use of RICs include pretargeting to safely improve biodistribution and improve efficacy.79 Weiden et al80 administered rituximab conjugated to streptavidin to bind to tumor-associated antigen receptors, followed by biotin-N-acetyl-galactosamine to remove nonlocalized conjugate from the circulation. The tumor-to–whole-body radiation dose following the chelate-biotin ligand labeled with 111In for imaging and 90Y for therapy was higher than previously observed without pretargeting; response rates in the 10 patients were considered encouraging, and toxicity was reportedly mild.
Most important, RICs should form the basis of more effective, multiagent therapies, combined with chemotherapy, other antibodies or biologics.81,82 Combining RICs with chemotherapy will be a challenge because of the overlapping myelosuppression, and sequencing these modalities may be the necessary alternative.64Press et al83 reported their experience with 6 cycles of CHOP (cyclophosphamide, hydroxydaunomycin, vincristine, prednisone) followed by iodine I 131 tositumomab in responding patients. The response rate of 80% was consistent with what has been reported with the RIC alone in this setting.55 The authors were appropriately cautious in noting that the study demonstrated feasibility, but a demonstration of efficacy required a randomized trial. The Southwest Oncology Group is currently conducting a randomized, prospective trial comparing (1) CHOP; (2) CHOP combined with rituximab; or (3) CHOP followed by iodine I 131 tositumomab.
For RICs to achieve their potential, they must be administered safely. It is critical for physicians to strictly adhere to the prescribed eligibility criteria, notably bone marrow involvement less than 25%, platelet counts more than 100 000/mm3, and no prior stem cell transplantation. Phase 1 trials are under way to determine if RICs can be safely given to patients with extensive (> 25%) bone marrow infiltration. The development of a collaborative treatment team and an institutional model for the delivery of RIC therapy is essential, with a hematologist/oncologist, nuclear medicine physician, radiation oncologist, radiation pharmacist, radiation safety officer, an oncology or radiation oncology nurse, and a coordinator to schedule all aspects of the therapy.
The availability of this exciting new class of agents affords great promise for developing effective, targeted treatment strategies. Nevertheless, further clinical development is required to optimize their activity while limiting toxicities. The rational and safe incorporation of these agents into multimodality regimens will hopefully increase the overall survival and cure rate for patients with NHL.
Prepublished online as Blood First Edition Paper, September 19, 2002; DOI 10.1182/blood-2002-06-1793.
Correspondence:Bruce D. Cheson, Georgetown University Hospital, Lombardi Cancer Center, 3800 Reservoir Rd NW, Washington, DC 20007.