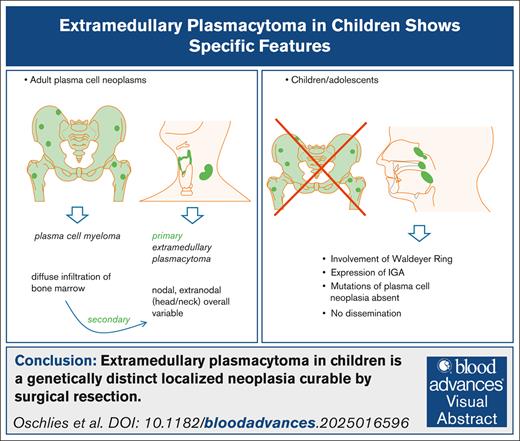
Key Points
EMPs in children and adolescents are localized extranodal diseases of the head and neck area, lacking dissemination.
Expression of immunoglobulin A and lack of genetic aberrations characterize this disease, which is curable by surgical resection.
Visual Abstract
Extramedullary plasmacytomas (EMPs) are exceedingly rare in children and adolescents. We describe clinical, pathological, and molecular features of 13 patients with EMP in this age group (8 males and 5 females; age 3-18 years). EMPs presented as localized disease involving the Waldeyer’s ring (n = 9), larynx (n = 2), ocular adnexa (n = 1), or epipharynx and conjunctiva simultaneously (n = 1). One patient with EMP of the tonsils had a concurrent Epstein-Barr virus infection. Twelve of 13 patients with follow-up information reached sustained complete remissions after surgical resection (median follow-up, 38 months). However, local relapses were observed in 3 patients. Irradiation was applied in only 1 patient with laryngeal involvement. Histologically, sheets of mature plasma cells with light chain restriction, low proliferation, and predominant expression of immunoglobulin A (11/13 [92%]) were observed. Epstein-Barr virus, CD56, and cyclin D1 were not detected in the plasma cells. Amyloidosis confined to the lesion was observed in 1 case. Clonal, mostly productive immunoglobulin gene rearrangements with somatic hypermutation (3.3%-5.7%) were detectable in all informative cases. Fluorescence in situ hybridization revealed absence of chromosomal abnormalities associated with plasma cell neoplasia (eg, breaks in IGH, MAF, FGFR3, and copy number alterations of 1p32, 1q21, RB1, and TP53). Targeted next-generation sequencing did not reveal any somatic alterations predicted as pathogenic. We conclude that EMP in children and adolescents is a plasma cell neoplasia with low malignant potential lacking systemic dissemination, differing clinically and molecularly from adult plasma cell myeloma.
Introduction
Plasma cell neoplasms are frequent diseases in adult patients but rare in children and adolescents. In fact, plasma cell myeloma involving the bone marrow is virtually never observed in children and adolescents aged <18 years.1,2 However, 7 cases of extramedullary plasmacytomas (EMPs; extraosseous and extranodal) in children have been reported in the literature so far and are summarized in supplemental Table 5.3-8 Both International Consensus Classification and World Health Organization classification solely describe EMPs in adults and distinguish them from systemic plasma cell neoplasia.9,10 A “pediatric type” of EMP is not mentioned in these classifications.9,10 Even in adults, systematic immunophenotypic and molecular analyses of EMPs are rare in the current literature.11-14 Molecular and clinical data of EMP in children and adolescents are limited to only a few case reports.3-8 Consequently, pathologists lack diagnostic references, and pediatric oncologists lack clinical experience to manage this disease. Here, we gathered clinical, histopathological, and molecular data of 13 cases of EMP in children and adolescents (aged ≤18 years). Cases were identified over a period of 13 years, mostly among patients reported to the German and Austrian Non-Hodgkin Lymphoma, Berlin-Frankfurt-Münster (NHL-BFM) study group. We identified rather homogenous clinical and molecular features, suggesting that EMP in children and adolescents represents a distinct biological subgroup within the spectrum of plasma cell neoplasms.
Material and methods
Selection of patients and samples
Eleven of 13 patients with EMP were registered into NHL-BFM study group registry, a population-based registry for children and adolescents of all subtypes of non-Hodgkin lymphoma including plasma cell neoplasia in Austria, Germany, Czech Republic, and Switzerland. Two additional patients not included in the NHL-BFM database were referred to the Hematopathology Section and Lymph Node Registry, Kiel, Germany, for diagnostic consultation. The biopsy samples of the patients were reviewed by hematopathology experts at initial diagnosis and reanalyzed for this study. Diagnostic criteria of EMP according to the current lymphoma classifications were met in all cases.9,10 Clinical data were retrieved from the NHL-BFM files and complemented by data from patient files by treating physicians as required (Table 1). Two patients (patients 12 and 13; Table 1) had previously been described in a case report.5 All other patients have not been reported before. Staging was performed using the revised International Pediatric Non-Hodgkin Lymphoma Staging System.15
Clinical features of 13 EMPs in children
| Patient . | Age (y)/gender . | Involved site . | Presenting symptoms . | Staging IPNHLSS . | Staging methods . | Urine/serum paraprotein (electrophoresis) . | Treatment . | Local relapse (time from ID) . | Follow-up, mo . | Outcome last FU . | Underlying Immuno-deficiency∗ . | Associated infection/autoimmune disorder† . |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 4/F | Tonsil | Snoring and frequent infections | I-EN | PET-CT, BMT, BMA, LP, and MRI | No‡/no | Resection at ID and relapse, w&w | Yes (2 and 3 years after ID) | 37 | Local relapse§ | No | No |
| 2 | 6/M | Palatal arch | Symptoms of adenoid hyperplasia and incidental finding of small tumor during adenectomy | I-EN | MRI, BMT, and bone scan | na/na | Resection, w&w | No | 12 | CR (CT) | No | No |
| 3 | 4/M | Tonsil (adenoid) | Progressing nasal breathing difficulties (3 weeks) | I-EN | PET-CT, BMT, and BMA | No/no | Resection, w&w | No | 24 | CR (PET-MRI) | No | No |
| 4 | 6/F | Eyelid | Tumor right upper median eyelid increasing over months | I-EN | MRI (whole body) and BMA | na/no | Incomplete resection, w&w | No | 12 | CR (MRI) | No | No |
| 5 | 3/M | Tonsil (adenoid) | Snoring, progressing enlargement of tonsils and adenoids, and cervical lymphadenopathy (5-6 months) | I-EN | MRI (whole body), BMA, and LP | na/na | Resection, w&w | No | 96 | CR (MRI) | No | No |
| 6 | 4/F | Tonsil (adenoid) | Upper airway obstruction | I-EN | PET-CT, BMT, BMA, and LP | No/no | Resection at ID and relapse, w&w | Yes (10 months and 3 years after ID) | 102 | CR (MRI), rebiopsy of initial site | No | No |
| 7 | 9/M | Larynx, vestibulum and supraglottis | Increasing dysphonia over 3-4 months; at diagnosis loss of voice | I-EN | PET-CT and BMA | No/no | Local irradiation (50.4 Gy), resection | No | 64 | CR (voice back to normal) | No | No |
| 8 | 6/M | Supraglottic tumor | Intermittent hoarseness for 3 years; progressing snoring and breathing difficulties for 6 months | I-EN | MRI, sonography, and laryngoscopy | na/no | Resection, w&w | No | 19 | CR (MRI, voice nearly normal) | No | Acute EBV (IgM+) infection |
| 9 | 18/F | Tonsil, bilateral | Clinical suspicion of EBV-associated tonsillitis | I-EN | CT, BMT, and FCM | No/no | Resection at ID and relapse, w&w | Yes (20 months after ID)|| | 24 | CR | No | Borderline EBV-IgM suspicion of EBV infection |
| 10 | 6/M | Adenoid | Reduced hearing and adenectomy | I-EN | BMT, FCM, and PET-MRI | No/no | Resection, w&w | No | 17 | CR | No | No |
| 11 | 15/F | Epipharynx, left conjunctiva | Adenoids and flat conjunctival lesion | II-EN | MRI and PET-CT | na/na | Resection, w&w | No | 243 | CR | No | No |
| 12 | 4/M | Epipharynx | Adenoid vegetations, chronic rhinitis, and recurrent otitis media | I-EN | MRI, bone scan¶, and BMA | No/no | Resection, w&w | No | 52 | CR | No | No |
| 13 | 4/M | Epipharynx | Adenoid vegetations, obstructive bronchitis, and breathing problems | I-EN | MRI, bone scan¶, and BMA | No/no | Resection, w&w | No | 85 | CR | No | No |
| Patient . | Age (y)/gender . | Involved site . | Presenting symptoms . | Staging IPNHLSS . | Staging methods . | Urine/serum paraprotein (electrophoresis) . | Treatment . | Local relapse (time from ID) . | Follow-up, mo . | Outcome last FU . | Underlying Immuno-deficiency∗ . | Associated infection/autoimmune disorder† . |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 4/F | Tonsil | Snoring and frequent infections | I-EN | PET-CT, BMT, BMA, LP, and MRI | No‡/no | Resection at ID and relapse, w&w | Yes (2 and 3 years after ID) | 37 | Local relapse§ | No | No |
| 2 | 6/M | Palatal arch | Symptoms of adenoid hyperplasia and incidental finding of small tumor during adenectomy | I-EN | MRI, BMT, and bone scan | na/na | Resection, w&w | No | 12 | CR (CT) | No | No |
| 3 | 4/M | Tonsil (adenoid) | Progressing nasal breathing difficulties (3 weeks) | I-EN | PET-CT, BMT, and BMA | No/no | Resection, w&w | No | 24 | CR (PET-MRI) | No | No |
| 4 | 6/F | Eyelid | Tumor right upper median eyelid increasing over months | I-EN | MRI (whole body) and BMA | na/no | Incomplete resection, w&w | No | 12 | CR (MRI) | No | No |
| 5 | 3/M | Tonsil (adenoid) | Snoring, progressing enlargement of tonsils and adenoids, and cervical lymphadenopathy (5-6 months) | I-EN | MRI (whole body), BMA, and LP | na/na | Resection, w&w | No | 96 | CR (MRI) | No | No |
| 6 | 4/F | Tonsil (adenoid) | Upper airway obstruction | I-EN | PET-CT, BMT, BMA, and LP | No/no | Resection at ID and relapse, w&w | Yes (10 months and 3 years after ID) | 102 | CR (MRI), rebiopsy of initial site | No | No |
| 7 | 9/M | Larynx, vestibulum and supraglottis | Increasing dysphonia over 3-4 months; at diagnosis loss of voice | I-EN | PET-CT and BMA | No/no | Local irradiation (50.4 Gy), resection | No | 64 | CR (voice back to normal) | No | No |
| 8 | 6/M | Supraglottic tumor | Intermittent hoarseness for 3 years; progressing snoring and breathing difficulties for 6 months | I-EN | MRI, sonography, and laryngoscopy | na/no | Resection, w&w | No | 19 | CR (MRI, voice nearly normal) | No | Acute EBV (IgM+) infection |
| 9 | 18/F | Tonsil, bilateral | Clinical suspicion of EBV-associated tonsillitis | I-EN | CT, BMT, and FCM | No/no | Resection at ID and relapse, w&w | Yes (20 months after ID)|| | 24 | CR | No | Borderline EBV-IgM suspicion of EBV infection |
| 10 | 6/M | Adenoid | Reduced hearing and adenectomy | I-EN | BMT, FCM, and PET-MRI | No/no | Resection, w&w | No | 17 | CR | No | No |
| 11 | 15/F | Epipharynx, left conjunctiva | Adenoids and flat conjunctival lesion | II-EN | MRI and PET-CT | na/na | Resection, w&w | No | 243 | CR | No | No |
| 12 | 4/M | Epipharynx | Adenoid vegetations, chronic rhinitis, and recurrent otitis media | I-EN | MRI, bone scan¶, and BMA | No/no | Resection, w&w | No | 52 | CR | No | No |
| 13 | 4/M | Epipharynx | Adenoid vegetations, obstructive bronchitis, and breathing problems | I-EN | MRI, bone scan¶, and BMA | No/no | Resection, w&w | No | 85 | CR | No | No |
BMA, bone marrow aspirate; BMT, bone marrow trephine biopsy; CR, complete remission; CT, computed tomography; F, female; FCM, flow cytometry; FU, follow up; ID, initial diagnosis; IPNHLSS, International Pediatric Non-Hodgkin Lymphoma Staging System; LP, lumbar puncture; M, male; MRI, magnetic resonance imaging; na, not available; nd, not done; PET, positron emission tomography; w&w, watch and wait.
No clinical evidence of an underlying immune defect or autoimmunity.
Associated infection specifically mentioned within the medical records and/or confirmed by serology.
Doubtful urine paraprotein measured once.
Child was lost to follow-up immediately after diagnosis of second local relapse.
The patient developed new adenoid-like proliferations 20 months after the initial diagnosis. Histopathology revealed a small area (10%) of the EMP and reactive hyperplasia in the remaining specimen; serum immune-fixation was negative at relapse.
Technetium (99Tc) bone scintigraphy.
Histopathology and immunohistochemistry
Histopathological and immunohistochemical features were assessed using archival slides and completed with additional analysis in cases with available paraffin material. Due to the retrospective nature of the study, completeness of data varied from case to case. Expression of CD20, κ and λ light chains, immunoglobulin G (IgG) and IgA, CD56, cyclin D1, Epstein-Barr virus (EBV; via EBV-encoded small RNA [EBER]-in situ hybridization), and Ki67 were analyzed by standard immunohistochemistry with approved protocols for diagnostic human tissue processing (Leica Bond automated stainer) and visual inspection. Amyloid subtyping was performed in 1 case as previously reported.16
FISH
Fluorescence in situ hybridization (FISH) for chromosomal translocations and numerical aberrations was performed on 2-μm slides from diagnostic specimens, as previously described.17 Probes for immunoglobulin heavy chain gene (IGH) break-apart, Cyclin D1 (CCND1) break-apart, 8q24 (MYC) break-apart, t(4p16.3;14q32) (FGFR3∷IGH), t(14q3;16q23) (IGH∷MAF), 1p32.2/1q21.3-q22 (CDKNC/CKS1B), 13q34/13q14.2 (RB1/LMP), and 17p13/17cen (TP53) were obtained from ZytoVision (Bremerhaven, Germany). Additional (molecular) cytogenetic data were available for individual cases.
DNA extraction
DNA extraction from formalin-fixed paraffin-embedded biopsy material was performed using GenRead or QIAamp DNA Mini DNA extraction Kit (Qiagen, Hilden, Germany) according to the manufactureŕs instruction. In case of partial infiltration of the whole tissue, macrodissection of the infiltrated area was performed. In all other cases, whole tissue slices were used for DNA extraction.
Immunoglobulin gene rearrangements
DNA from 12 of 13 patients was analyzed for clonal rearrangement of IGH and/or κ light chain using the BIOMED2 protocol.18
Next-generation sequencing (NGS)
From 7 patients, DNA of sufficient quality was available for further molecular analyses using 2 different assays. An AmpliSeq custom DNA panel covering 36 genes or mutational hot spots known to be recurrently mutated in B-cell lymphomas was used, as previously published.19-21 The panel included genes recurrently mutated in indolent pediatric B-cell lymphomas, such as MAP2K1, TNFRSF14, IRF8, and TP53.22,23 Data were analyzed as previously described.19,24 In addition, the EuroClonality next generation clonality (NDC) assay by Univ8 Genomics25 covering immunoglobulin rearrangements, somatic mutations in 72 lymphoma-related genes, as well as copy number variations and translocations, was used according to the manufacturer’s instructions. Data processing included the ARResT/interrogate pipeline,26 together with the Hyper tool for IGH somatic hypermutation analysis (supplemental Table 1). Filtering was based on the Univ8 analysis guide line (release February 2024) with the following settings. Sequence variant analysis was done on curated variants with at least 4 fragments containing the event (numerator) and/or at least 10% variant allel frequency to avoid detection of formalin-fixed paraffin-embedded biopsy material–associated artifacts. To identify clonal immune gene rearrangements, the following filter sets were used: reads (numerator) ≥5, genes ≥5%, percentage in locus ≥5%, and rearrangements with “X” in junction were excluded. To identify the IGH somatic hypermutation status, only productive IGH rearrangements with at least 2% somatic hypermutation were considered.
Because germ line DNA for interpretation of somatic alterations was not available, variant detection for both panels were done using in silico prediction by VarSome, including somatic variant classification by ClinVar annotation.27
This study was conducted according to the recommendations of the ethics advisory committee of the Medical Faculty of the University of Kiel for the use of archival tissue specimen (review number D447/10). All patients and/or their parents or legal guardians gave informed consent for the transfer of their data to the NHL-BFM study center (ethical vote NHL-BFM registry 2012-206-f-S and 76/12). Informed consent was obtained from the 18-year-old patient who was not registered in the NHL-BFM database.
Results
Clinical features
The clinical characteristics of patients with EMPs are summarized in Table 1. The series included 5 females and 8 males, with a mean age of 6.8 years (range, 3-18). The disease affected the Waldeyer’s ring in 10 of 13 patients, specifically the tonsils/adenoids in 6 and the epipharynx/palatal arch in 4 patients. The larynx was affected in 2 of 13 patients and the conjunctiva in 2 of 13 patients. One of the latter presented with concurrent involvement of the epipharynx (patient 11; Table 1). The patient’s symptoms were mostly related to airway obstruction due to nasopharyngeal involvement (Table 1). Two patients presented with complete loss of voice and hoarseness due to laryngeal involvement. In 1 patient, the disease manifested as a slowly growing tumor of the eye lid. Methods used for staging varied between cases. Twelve patients presented with International Pediatric Non-Hodgkin Lymphoma Staging System stage I-EN and 1 patient with stage II-EN disease (Table 1). B-symptoms were absent in all 12 patients, and serum lactate dehydrogenase levels were normal in 9 of 9 informative patients. None of the children showed symptoms or clinical features of systemic plasma cell disease. Of note, serum and/or urine electrophoresis did not demonstrate a clonal gammopathy in 10 of 10 informative patients (Table 1). However, in 5 of 6 patients with data, serum IgA was increased to 1.8- to 2.8-fold of the upper limit of normal. The bone marrow was investigated by bone marrow aspiration (9/13) and/or trephine biopsy (6/13) and did not reveal clonal plasma cell expansion in any case.
No immunodeficiency or autoimmune disorder was reported for the patients in this case series. Serological evidence of primary EBV infection with positive EBV viral capsid antigen–IgM serology was described in 1 child at the time of EMP diagnosis (patient 8; Table 1). A second patient (patient 9; Table 1) was reported to present with clinical features of ulcerative tonsillitis. A clinically suspected acute EBV infection was not definitely proven because sequential serological test for EBV did not distinguish between acute infection with low anti–viral capsid IgM and unspecific polyclonal B-cell stimulation with sufficient certainty. Other concomitant infections were not reported in the remaining 11 patients. Resection followed by watch and wait resulted in complete remission in 11 of 11 informative patients. Of these patients, 2 suffered from a localized relapse, underwent surgery for a second time, and reached complete remission again (patients 6 and 9; Table 1). One child with infiltration of the vocal cord received fractioned local irradiation with a complete dose of 50.4 Gy, which led to complete remission (patient 7; Table 1). The median follow-up for 12 patients was 38 months (range, 12-243). One patient was lost of follow-up immediately after the second local relapse, which was again treated by resection (patient 1). The voice of the 2 children with hoarseness due to laryngeal involvement (patients 7 and 8; Table 1) normalized completely in one and turned to an almost normal voice in the other.
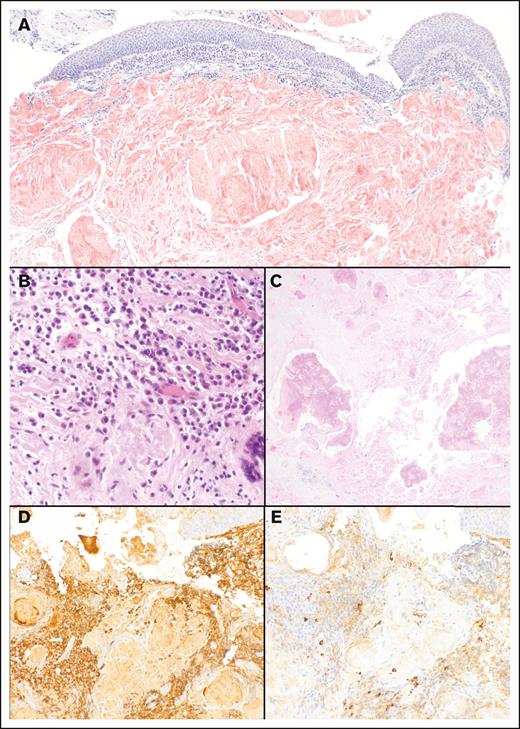
Histopathological features
The lesions consisted of sheets of mature to slightly pleomorphic plasma cells, with partially (n = 9) or completely effaced tissue architecture (n = 4). In 10 of 10 cases affecting the Waldeyer’s ring, remnants of attenuated reactive B-cell follicles were observed, with plasma cells expanded in the interfollicular areas. Approximately 30% to 90% of the entire surgically resected tumor samples were infiltrated by EMP (n = 12), indicating a considerable tumor mass. One case infiltrating the vocal cord presented with dense subepithelial depositions of amyloid, accompanied by small aggregates of mature plasma cells accounting for only 5% to 10% of the sample area (patient 7; Figure 1). Although the histology of the lesions is dominated by sheets of CD20– light chain–restricted plasma cells, small foci of CD20+ plasma cells or plasma blasts were observed in 3 of 13 patients. Areas with proliferation of small CD20+ B cells, reminiscent of plasmacytic-differentiated small B-cell lymphoma, were absent in all cases. A representative case of an IgA+ EMP arising in the tonsils is shown in Figure 2.
EMP with concurrent EBV infection (patient 8). (A,C,E) Tonsillar areas with infiltration by a plasmacytoma with sheets of plasma cells with monotypic expression of λ (A, om ×25; C, om ×200) and negativity for κ (E, om ×200). (B) These areas are EBV/EBER negative (om ×25). (B,D,F) Reactive areas contain EBV+ B cells (EBER; B, om ×25; and inset B′, om ×400) and polyclonal plasma cells (D [λ], om ×400; F [κ], om ×400).
EMP with concurrent EBV infection (patient 8). (A,C,E) Tonsillar areas with infiltration by a plasmacytoma with sheets of plasma cells with monotypic expression of λ (A, om ×25; C, om ×200) and negativity for κ (E, om ×200). (B) These areas are EBV/EBER negative (om ×25). (B,D,F) Reactive areas contain EBV+ B cells (EBER; B, om ×25; and inset B′, om ×400) and polyclonal plasma cells (D [λ], om ×400; F [κ], om ×400).
Histopathology of an EMP infiltrating the tonsil (patient 3). (A-B) An interfollicular expansion of CD20– (original magnification [om] ×25) (A) and IgA+ plasma cells (om ×25) (B) is seen. CD20 highlights B-cell follicles, which are in part attenuated. (C-D) Interfollicular areas contain sheets of mature plasma cells (hematoxylin and eosin; C, om ×100; D, om ×400). (E-F) The plasma cells are monotypic and express κ (om ×400) (E) but remain negative for λ light chain (om ×400) (F).
Histopathology of an EMP infiltrating the tonsil (patient 3). (A-B) An interfollicular expansion of CD20– (original magnification [om] ×25) (A) and IgA+ plasma cells (om ×25) (B) is seen. CD20 highlights B-cell follicles, which are in part attenuated. (C-D) Interfollicular areas contain sheets of mature plasma cells (hematoxylin and eosin; C, om ×100; D, om ×400). (E-F) The plasma cells are monotypic and express κ (om ×400) (E) but remain negative for λ light chain (om ×400) (F).
Plasma cells expressed either light chain κ (6/13) or λ (7/13). Heavy chains expressed by the plasma cells were mostly IgA (11/13) and, less frequently, IgG (2/13). Patient 9 presented with multifocal bilateral involvement of the tonsils, predominately composed of IgG λ+ plasma cells. Interestingly, in this patient, a separated minor area with IgA λ+ plasma cells was detectable. The amyloid observed in one was identified as κ light chain amyloid, the same light chain as expressed by the EMP (patient 7; Figure 1). EBV/EBER was negative in all cases tested (12/12). One of 2 EMP with positive serology for EBV-IgM displayed peritumoral EBV+ cells, whereas the plasma cells themselves were EBER negative (patient 6; Figure 3). EMP did not express CD56 (0/10) or cyclin D1 (0/12). Ki67 was low to moderate (5%-40%). In 3 EMPs, small foci with higher proliferation were observed and were associated with CD20 reactivity in plasma cells.
EMP involving the larynx (vestibular fold) with associated light chain amyloid (patient 7). (A) Tumor forming subepithelial amyloid is detectable in the Kongo red staining (om ×25). (B-C) Subepithelial mature plasma cells (B, om ×20) and amyloid depositions (C, om ×200) are present. (D-E) Plasma cells show expression of κ (D, om ×400) and remain negative for λ light chain (E, om ×400).
EMP involving the larynx (vestibular fold) with associated light chain amyloid (patient 7). (A) Tumor forming subepithelial amyloid is detectable in the Kongo red staining (om ×25). (B-C) Subepithelial mature plasma cells (B, om ×20) and amyloid depositions (C, om ×200) are present. (D-E) Plasma cells show expression of κ (D, om ×400) and remain negative for λ light chain (E, om ×400).
Clonal immunoglobulin gene rearrangements
A clonal immunoglobulin gene rearrangement was detected in all informative patients (12/12) using a polymerase chain reaction (PCR)–based protocol.28 Low DNA-quality hampered further molecular analyses of a single case, which, nevertheless, can be assumed clonal based on the light chain restriction.
In addition, clonal IGH rearrangement was confirmed by NGS in 5 of 7 patients, 4 of which were productive. Of these patients, productive κ or λ rearrangements were detected in 2 and 3 patients, respectively (Table 2; supplemental Table 2). The productive light chain rearrangement corresponded to the light chain expressed/detected by immunohistochemistry (Table 2). In one patient, a productive IGH and 2 productive light chain rearrangements were observed (patient 3; Table 2). Productive IGH genes were significantly mutated, with levels of somatic hypermutations ranging from 3.3% to 5.7%, compared to germ line sequences. The level of somatic hypermutation found in our cohort does not differ significantly from an unpublished cohort of systemic adult plasma cell myelomas (M.B. and C.B., data not shown). Only 1 patient displayed a clonal λ but no detectable IGH rearrangement (patient 8; Table 2). NGS failed to demonstrate clonal immunoglobulin gene rearrangements, despite clonality in the PCR-based protocol in 1 specimen. In the limited number of cases for which sequence data of IGH were available, a biased use of IGH-VJ segments was not observed (Table 2).
Immunohistochemical and molecular features of 13 EMPs in children
| Patient . | Immunophenotype cyclin D1/CD56/EBER/Ki67 . | Expressed immunoglobulin . | FISH . | Molecular analysis . | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| IGH-break . | RB1 Del . | TP53 Del . | 1p/1q . | Clonality (Biomed∗) . | IGH rearrangement (IGHV)† . | IGK/L rearrangement† . | Somatic variants . | |||
| 1 | –/–/–/5%-10% | IgA, κ | nd | nd | nd | nd | IGH | IGH V3-23 J2 (5.13%); IGH V3-33 J4 | IGK | None |
| 2 | –/–/–/5%-10% | IgA, λ | nd | nd | nd | nd | NE | nd | nd | nd |
| 3 | –/–/–/5%-10% | IgA, κ | - | - | - | - | IGH and IGK | IGH V3-48 J6 (5.73%) | IGK, IGL | None |
| 4 | –/–/–/5% | IgG, κ | - | - | - | - | nd | IGH D2-2 J4 | IGK | None |
| 5 | –/–/–/25% | IgA, κ | - | - | - | - | IGH | Not detected | Not detected | None |
| 6 | –/–/–/5%-10% | IgA, λ | nd | nd | nd | nd | IGH | nd | nd | nd |
| 7 | –/–/–/nd | IgG, κ | - | - | - | - | IGH | nd | nd | nd |
| 8 | –/–/–/5%-10% | IgA, λ | – | – | – | – | IGH | Not detected | IGL | None |
| 9 | –/–/–/5%-40% | IgA, IgG, λ‡ | – | – | – | – | IGH | IGH V1-18 D3-10 J3 (3.3%); IGH D7-27 J4 | IGL | None |
| 10 | –/nd/–/5%-40% | IgA, λ | – | – | – | – | IGH | IGH V3-11 J5 (5.1%); IGH D2-2 J6 | IGL | None |
| 11 | –/nd/–/5% | IgA, λ | – | – | – | – | IGH | nd | nd | nd |
| 12 | –/–/–/5% | IgA, λ | – | – | – | – | IGH | nd | nd | nd |
| 13 | –/–/nd/5%-10% | IgA, κ | nd | nd | nd | nd | IGH | nd | nd | nd |
| Patient . | Immunophenotype cyclin D1/CD56/EBER/Ki67 . | Expressed immunoglobulin . | FISH . | Molecular analysis . | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| IGH-break . | RB1 Del . | TP53 Del . | 1p/1q . | Clonality (Biomed∗) . | IGH rearrangement (IGHV)† . | IGK/L rearrangement† . | Somatic variants . | |||
| 1 | –/–/–/5%-10% | IgA, κ | nd | nd | nd | nd | IGH | IGH V3-23 J2 (5.13%); IGH V3-33 J4 | IGK | None |
| 2 | –/–/–/5%-10% | IgA, λ | nd | nd | nd | nd | NE | nd | nd | nd |
| 3 | –/–/–/5%-10% | IgA, κ | - | - | - | - | IGH and IGK | IGH V3-48 J6 (5.73%) | IGK, IGL | None |
| 4 | –/–/–/5% | IgG, κ | - | - | - | - | nd | IGH D2-2 J4 | IGK | None |
| 5 | –/–/–/25% | IgA, κ | - | - | - | - | IGH | Not detected | Not detected | None |
| 6 | –/–/–/5%-10% | IgA, λ | nd | nd | nd | nd | IGH | nd | nd | nd |
| 7 | –/–/–/nd | IgG, κ | - | - | - | - | IGH | nd | nd | nd |
| 8 | –/–/–/5%-10% | IgA, λ | – | – | – | – | IGH | Not detected | IGL | None |
| 9 | –/–/–/5%-40% | IgA, IgG, λ‡ | – | – | – | – | IGH | IGH V1-18 D3-10 J3 (3.3%); IGH D7-27 J4 | IGL | None |
| 10 | –/nd/–/5%-40% | IgA, λ | – | – | – | – | IGH | IGH V3-11 J5 (5.1%); IGH D2-2 J6 | IGL | None |
| 11 | –/nd/–/5% | IgA, λ | – | – | – | – | IGH | nd | nd | nd |
| 12 | –/–/–/5% | IgA, λ | – | – | – | – | IGH | nd | nd | nd |
| 13 | –/–/nd/5%-10% | IgA, κ | nd | nd | nd | nd | IGH | nd | nd | nd |
Overview of results of immunohistochemistry, FISH, and molecular analysis to identify clonal rearrangements and somatic variants are shown. For the EuroClonality NDC assay % of somatic hypermutation within productive IGH and only the productive light chain rearrangements are shown. nd was due to not having sufficient material available. Minus symbol represents negativity.
NE, not evaluable.
∗Clonality was analyzed using IGH/κ PCR Biomed.
†Clonality was analyzed using the EuroClonality NDC assay; it was also used to analyze the samples in respect to potential somatic variants. In the table, the clonal IGH and IGK/IGL rearrangement is provided.
‡Bilateral adenectomy with predominant areas IgG, λ and a small focus IgA, λ.
From patient 9 with bilateral multifocal involvement, macrodissected areas from both sides of the tonsils were investigated independently and demonstrated identical rearrangements by NGS and PCR-based immunoglobulin analysis, suggesting a class switch of a subclonal population within the EMP (supplemental Table 2).
Absence of chromosomal aberrations
The results of the FISH analyses are summarized in Table 2. FISH for chromosomal breaks/fusions (MAF, FGFR3, and IGH) and numerical aberrations (1p32/1q21, RB1, and TP53) revealed no pathological findings in 9 cases analyzed. Additional molecular cytogenetic investigations performed during the initial diagnostic process of patients 1 and 11 revealed no aberrations (patient 1, FISH for numerical aberrations of chromosomes 3, 7, and 18 and breaks of MALT1, BCL6, IGH, and MYC; patient 11, numerical aberrations of chromosomes 12 and 13 and breaks of MALT1, BCL10, and CCDN1). Furthermore, 3 cases investigated by FISH for a MYC break and 6 cases investigated for a CCDN1 break were negative.
Absence of somatic mutations
Targeted sequencing was available for 7 EMPs. Six cases were investigated by both the AmpliSeq and the EuroClonality NDC assays and one by the EuroClonality NDC assay only. Eleven (in 7 patients) and 7 potential protein changing variants (in 6 patients) were detected by the 2 assays, respectively. Of these variants, 2 of 18 were identified with both assays independently. By all tools applied, 16 of 18 variants were annotated as benign, likely benign, or of uncertain relevance (see supplemental Tables 3 and 4). A single in-frame deletion variant was not interpretable by VarSome. Only 2 variants were classified using the metascore by either 3 of 7 of the applied tools as pathogenic (ATM; c.2453T>C, p.Ile818Thr; variant allele frequency, 53%) or 1 of 6 (NOTCH1; c.6980G>A, p.Arg2327Gln; variant allele frequency, 46%). However, ClinVar revealed uncertain results for both of these variants (supplemental Table 3). Thus, no variant of likely pathogenic relevance was detected.
Discussion
In this study, we present a series of 13 EMPs arising in children and adolescents. Although very rare, our data prove that EMP belongs to the spectrum of B-cell lymphomas/lymphoproliferations of this age group. All cases presented as localized lesions in the head and neck area, mostly in the Waldeyer’s ring, without evidence of systemic plasma cell neoplasia. Six hitherto published cases of EMP in children show similar clinical features,3,4,6,8 including the 2 previously published case reports of patients, who are also part of our cohort and presented in our study with longer follow-up.5 The favorable outcome with sustained complete remissions after resection of the lesions suggests that surgery is a sufficient therapy in children and adolescents with EMP of the kind described in our study. Only 1 patient in our series and several cases of EMPs reported in the literature3,4,6-8 were treated with additional local irradiation. Given the achievement of complete remission by surgery alone in most cases presented here, we would postulate that local irradiation can be restricted to single cases, in which surgery alone seems insufficient or irradiation is indicated for other reasons by the treating oncologist. However, all patients have to be followed up carefully, because relapses may occur.
A series of IgA-expressing nodal and extranodal plasmacytomas with a low risk of progression to systemic plasma cell myeloma has previously been reported as a mixed-age cohort by Shao et al.7 This publication included 1 pediatric patient and 1 adult patient with an localized EMP of the larynx and the Waldeyer’s ring, respectively. Interestingly, these 2 patients from Shao et al showed features similar to the patients in our cohort; for example, expression of IgA and lack of dissemination.7 However, most cases in Shao et al (including 3 aged <18 years) were nodal IgA+ plasma cell proliferations involving multiple lymph nodes in patients suffering from immune system dysfunction.7 In contrast to the published cases, the children in our series showed neither clinical features of immunodeficiency or autoimmunity nor nodal involvement. Previous studies indicate that EMP may also present as extramedullary/extranodal localized disease with involvement of the upper aerodigestive tract showing low malignant potential in adult patients.14,29 Similar to the pediatric cases presented in our study, EMP in adults lack cyclin D1 expression and rarely express CD56.11 In contrast to pediatric and adolescent EMPs in our cohort, extramedullary/extranodal EMPs in adults frequently harbor immunoglobulin gene translocations.12 In adult EMP, it seems impossible to predict potential progression to systemic plasma cell neoplasia solely by histopathology.9,10,12,13 Whether the subgroup of adult EMPs with features comparable to the pediatric/adolescent disease of our study (localized extranodal presentation, lack of genetic aberrations, and expression of IgA) show a similar low malignant potential needs to be addressed by future systematic observations. So far, we can only state that EMPs with the features reported in our series do not represent a phenomenon restricted to children and adolescents but might be observed in adults as well.
Except for histopathology, EMPs do not share clinical and molecular features with plasma cell myeloma. Therefore, their classification as a variant of marginal zone lymphoma (MZL) with plasmacytic differentiation may be discussed.30 The current definition of MZL includes the presence of a small B-cell component, which is usually CD20+.14 However, the neoplastic cells reported in our cohort were completely differentiated as plasma cells, and a small B-cell component was not detected. Assuming EMP to be a subtype of MZL, 1 should expect a spectrum of differentiation between EMP and MZL in the age group analyzed. However, plasmacytic differentiation is rarely observed in MZL arising in children and adolescents.31,32 Pediatric nodal MZL (PNMZL) is considered an entity by the World Health Organization classification.10 However, recent histopathological and genomic studies demonstrate that PNMZL shows considerable overlap with follicular lymphoma of the pediatric type (PTFL); for example, by shared recurrent mutations (MAP2K, TNFRSF14, and IRF8).22,23,33 Neither the histopathological features of PNMZL/PTFL, such as expanded germinal centers, nor the molecular alterations of these entities were observed in our cohort. Furthermore, the clinical presentation of EMP is obviously different from PNMZL/PTFL because extranodal manifestations are absent in PNMZL/PTFL and the extent of male predominance of PNMZL/PTFL is missing among EMPs in this age group.10 Instead, the cases in our cohort may represent extranodal MZLs with involvement of mucosal sites and indolent behavior, of which only few cases have been reported.31,32,34 Our cases mostly involved lymphoepithelial sites, whereas extranodal MZLs seem to occur predominantly in organs that are not considered primary lymphatic organs (eg, conjunctiva and larynx). Whether and how the specific site is associated with pathogenesis need to be explored in future studies.
Given the rather benign course of the disease and the absence of genetic alterations known from other B-cell lymphomas, one might speculate that EMPs represent an immune reaction rather than a neoplasia. This interpretation would also be supported by the observation of 2 EMPs arising simultaneously with a primary EBV infection in our cohort. In addition, localization to immunological interface organs, such as the tonsils, and IgA expression may indicate that EMPs are driven by inflammation. However, several lines of evidence suggest a neoplastic nature of EMPs. First, EMPs are molecularly clonal expansions forming clinically detectable lesions, which show organ damage and require surgical resection. Second, in contrast to what we expect from inflammation, most EMPs do not recur after resection. Third, with the exception of 1 patient, and likely a second patient, suffering from simultaneous EBV infection, most patients did not show clinical features of inflammatory disease at the time of diagnosis. Because the majority of patients did not show concurrent EBV infection, we also have to conclude that at least no joint inflammatory cause of EMPs can be deduced from our data. Of note, all cases of EMPs in our series, including the 2 with likely concomitant EBV infection, were EBER-negative tumors; thus, EBV does not seem to be a direct oncogenic driver in this disease. In line with this interpretation, only 1 case of an EBV+ EMP was reported in the literature, and this case seems to differ from the cases of our cohort in several aspects, because it shares features with plasmablastic lymphoma.35 Fourth, an EMP in our cohort (patient 7) and 2 previous case reports4,8 were associated with localized light chain amyloid and show overlap with plasma cell proliferations named as “localized IG light chain amyloidosis,” a disorder commonly regarded as neoplastic.9,14,16 Thus, EMPs in children and adolescents are likely neoplastic proliferations of plasma cells with low malignant potential. To which extent inflammatory stimuli contribute to the clonal outgrowth of plasma cells remains uncertain so far. Future studies need to address the role of inflammation, including possible viral infections, in the pathogenesis of EMP. Moreover, age-overriding analyses of immunophenotypic and molecular features of EMPs will help delineate biological subtypes of plasma cell proliferations with low malignant potential in adults, following the blue print of pediatric-type follicular lymphoma.36-39
Acknowledgments
The authors thank Reina Zühlke, Dana Germer, Lorena Valles-Uriate, and Charlotte Botz-von Drathen (Department of Pathology, University Hospital Schleswig-Holstein) for excellent technical assistance. The authors are greatly indebted to the patients, families, and physicians who referred cases for consultation and provided clinical information.
This work was supported by the KinderKrebsInitiative Buchholz, Holm-Seppensen. The Non-Hodgkin Lymphoma, Berlin-Frankfurt-Münster Registry is supported by a grant from the Deutsche Kinderkrebsstiftung (DKS 2016.24, 2018.21, 2020.15, 2022.09, and 2024.22 [B.B. and W.W.]).
Authorship
Contribution: I.O., J.R., A. Alfert, F.C., K.K., M.B., and C.B. performed analysis and generated data; A. Attabarschi, S.M., I.S.-K., H.v.M., C.S., W.W., and B.B. provided patient data and material; I.O., W.W., B.B., and W.K. developed the concept of the study; I.O., J.R., and W.K. wrote the manuscript; I.O. made the figures; and all authors approved the final manuscript.
Conflict-of-interest disclosure: The authors declare no competing financial interests.
Correspondence: Ilske Oschlies, Hematopathology Section and Lymph Node Registry, Department of Pathology, University Hospital Schleswig-Holstein, Campus Kiel, Arnold-Heller-Str 3, Haus U33, D-24105 Kiel, Germany; email: ioschlies@path.uni-kiel.de.
References
Author notes
I.O., J.R., and A. Alfert contributed equally to this study.
Data access is provided upon request by contacting the corresponding author, Ilske Oschlies (ioschlies@path.uni-kiel.de).
The full-text version of this article contains a data supplement.

![EMP with concurrent EBV infection (patient 8). (A,C,E) Tonsillar areas with infiltration by a plasmacytoma with sheets of plasma cells with monotypic expression of λ (A, om ×25; C, om ×200) and negativity for κ (E, om ×200). (B) These areas are EBV/EBER negative (om ×25). (B,D,F) Reactive areas contain EBV+ B cells (EBER; B, om ×25; and inset B′, om ×400) and polyclonal plasma cells (D [λ], om ×400; F [κ], om ×400).](https://ash.silverchair-cdn.com/ash/content_public/journal/bloodadvances/9/15/10.1182_bloodadvances.2025016596/2/m_blooda_adv-2025-016596-gr1.jpeg?Expires=1764958937&Signature=GvcPY1v7XAV6PTRZRuNuQhbxgdcE2dPWtC2K-KPpyQeSYtVxYLV8MC7WGoOozk-ObklutOaOFLiDsAZpg~WR7QUVWXoJCKwCMtVHlXsE8-AZNeJj2P~4Kyl2VaDuFjlCPXtx81TwYppjV9XjFInEA8HcWN0KNIxCt0UiAScYH4MA6Ely2Qzhf2E69Gi2BCgchv0a6hDaHmM8-3ucUFWUrecDokWIaTP0fXTWDjxFNkZ3LvHT0q~z8EUAwqwyiAPg5lif-t8EW1jOpm2B~W6o-tfj269OiE7INg9-U--hRjSrjuxNSCljgRcK-AyNVASY5Had6JYTNGd1gWvhv6amqQ__&Key-Pair-Id=APKAIE5G5CRDK6RD3PGA)
![Histopathology of an EMP infiltrating the tonsil (patient 3). (A-B) An interfollicular expansion of CD20– (original magnification [om] ×25) (A) and IgA+ plasma cells (om ×25) (B) is seen. CD20 highlights B-cell follicles, which are in part attenuated. (C-D) Interfollicular areas contain sheets of mature plasma cells (hematoxylin and eosin; C, om ×100; D, om ×400). (E-F) The plasma cells are monotypic and express κ (om ×400) (E) but remain negative for λ light chain (om ×400) (F).](https://ash.silverchair-cdn.com/ash/content_public/journal/bloodadvances/9/15/10.1182_bloodadvances.2025016596/2/m_blooda_adv-2025-016596-gr2.jpeg?Expires=1764958937&Signature=xzj1nkiiIUc907bgRu9zIcjgElGVivFMteXSlTFOGZwdNpua87DXU~zfyIS9JOHiLKsEAd5P8bJwNEmgiqEHAw~SpZfCiHrGJ290n7aflYCNUrdLdbBBEawpCK2DTOAl4O~WarAutCqJb-VBMqW~S9aV3HRPg9LDqlZsr4Df5WMutS2BldOZzEPdr-eZdceob3lJa3HEBfUEh4fJj7c-vhFQperFRhb-WEJRjLYOTFKm8UH-JF0J8~CJnXT44-eE3eT0CEzn2zF2-nYfbtyYWE1epk5tYkAiFAEmFbqP-RLaejnPEXIInkao4Uc~LgwWhegppO-1e7bb5mI-NbMyYQ__&Key-Pair-Id=APKAIE5G5CRDK6RD3PGA)