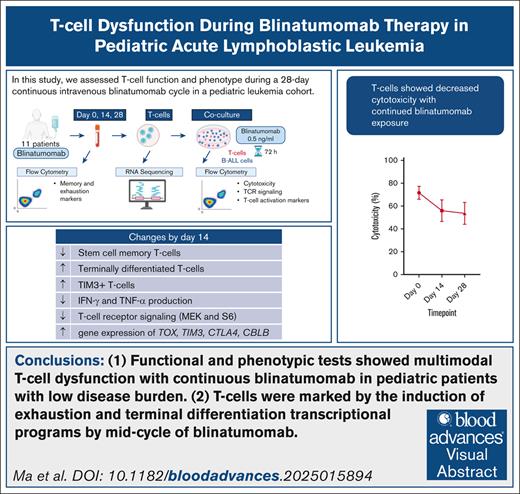
Visual Abstract
TO THE EDITOR:
Blinatumomab, a CD19/CD3 bispecific T-cell engager (BiTE) antibody, induces minimal residual disease (MRD) negativity in most children and adults (65%-93%)1-3 with MRD-positive relapsed/refractory (R/R) B-cell acute lymphoblastic leukemia (B-ALL). However, a proportion of patients exhibits a lack of response to blinatumomab (7%-35%)1-3 or a loss of response with repeat blinatumomab cycles (10%).4 Blinatumomab is typically administered as a 28-day continuous IV (cIV) infusion. Leukemic cells retain CD19 expression in most treatment failures5; data from a small study of adults with R/R B-ALL and high disease burden suggest T-cell dysfunction secondary to persistent stimulation of T cells from continued blinatumomab exposure as a key reason for treatment failure.6 Blinatumomab has been recently incorporated into B-ALL therapy in first remission in adults and children including patients with MRD negativity.7,8 However, age, leukemia burden, and previous chemotherapy intensity-related differences in immune function limit the extrapolation of T-cell dysfunction data from adults with R/R B-ALL and high disease burden to pediatric B-ALL in remission. Furthermore, the effects of continuous blinatumomab on T-cell receptor (TCR) signaling and the T-cell transcriptome remain poorly defined. Overall, a comprehensive assessment of the effects of continuous blinatumomab on T cells specifically in pediatric patients in complete remission is needed.
We conducted a prospective single-center observational cohort study that assessed changes in T-cell function and transcriptional programs, TCR signaling, and T-cell subsets (supplemental Methods; supplemental Table 1) during cIV blinatumomab in 11 pediatric patients (age = 1.0-21.4 years) with CD19+ leukemia and low disease burden. Blood samples were collected before blinatumomab (baseline) and at approximately days 14 (middle) and 28 (end) during a 28-day cIV blinatumomab infusion. Studies were done on samples from the first blinatumomab cycle, with rare exceptions. No patients received intravenous immunoglobulin within a month before sample collection. Most patients (9/11) were in first complete remission with 10 being MRD negative before receiving blinatumomab (Table 1; supplemental Table 2). Three patients had infant leukemia. All patients remained in remission at a follow-up time of 1.2 to 2.5 years.
Baseline patient characteristics of cohort
| Parameter . | n (%) Total cohort = 11 . |
|---|---|
| Age at initial diagnosis, y | |
| <1 | 3 (27) |
| 1-9.9 | 7 (64) |
| ≥10 | 1 (9) |
| Sex | |
| Female | 4 (36) |
| Male | 7 (64) |
| Ethnicity | |
| Not Hispanic or Latino | 5 (45) |
| Hispanic or Latino | 6 (55) |
| Initial diagnosis | |
| Standard-risk ALL | 5 (45) |
| High-risk ALL | 5 (45) |
| CD19+ MPAL | 1 (9) |
| Cytogenetics | |
| KMT2A rearranged∗ | 3 (27) |
| Philadelphia-chromosome positive | 2 (18) |
| Philadelphia-like (CRLF2 fusion) | 2 (18) |
| Hyperdiploidy | 2 (18) |
| Hypodiploidy | 1 (9) |
| iAMP21 | 1 (9) |
| Remission status | |
| CR1 | 9 (82) |
| CR2 | 2 (18) |
| MRD status before blinatumomab† | |
| Negative | 10 (91) |
| Positive | 1 (9) |
| Reason for blinatumomab | |
| Toxicity precluding chemotherapy | 4 (36) |
| Other | 7 (64) |
| Therapy before blinatumomab | |
| Induction | 6 (55) |
| Additional therapy | 5 (45) |
| Parameter . | n (%) Total cohort = 11 . |
|---|---|
| Age at initial diagnosis, y | |
| <1 | 3 (27) |
| 1-9.9 | 7 (64) |
| ≥10 | 1 (9) |
| Sex | |
| Female | 4 (36) |
| Male | 7 (64) |
| Ethnicity | |
| Not Hispanic or Latino | 5 (45) |
| Hispanic or Latino | 6 (55) |
| Initial diagnosis | |
| Standard-risk ALL | 5 (45) |
| High-risk ALL | 5 (45) |
| CD19+ MPAL | 1 (9) |
| Cytogenetics | |
| KMT2A rearranged∗ | 3 (27) |
| Philadelphia-chromosome positive | 2 (18) |
| Philadelphia-like (CRLF2 fusion) | 2 (18) |
| Hyperdiploidy | 2 (18) |
| Hypodiploidy | 1 (9) |
| iAMP21 | 1 (9) |
| Remission status | |
| CR1 | 9 (82) |
| CR2 | 2 (18) |
| MRD status before blinatumomab† | |
| Negative | 10 (91) |
| Positive | 1 (9) |
| Reason for blinatumomab | |
| Toxicity precluding chemotherapy | 4 (36) |
| Other | 7 (64) |
| Therapy before blinatumomab | |
| Induction | 6 (55) |
| Additional therapy | 5 (45) |
CR1, first complete remission; CR2, second complete remission; iAMP21, intrachromosomal amplification of chromosome 21; MPAL, mixed phenotypic acute leukemia.
All 3 patients with KMT2A-rearranged disease had infant leukemia; one of these 3 patients had CD19+ MPAL. Among the remaining 8 patients, 3 had National Cancer Institute high-risk B-ALL.
MRD negativity was defined as <0.01% disease by flow cytometry. The patient who was MRD positive (1.1%) achieved MRD negativity after blinatumomab.
Cytotoxicity was measured by flow cytometry after coculturing T cells and B-ALL cells with CD19/CD3 BiTE (supplemental Figure 1A). Overall, T cells showed a decline in cytotoxicity by the middle time point that persisted through the end of the cycle (mean cytotoxicity [baseline, middle, end] = 72%, 56%, 54%; Figure 1A; supplemental Figure 1B). However, cytotoxicity profiles displayed heterogeneity; minimal to no decline in cytotoxicity was seen in the 3 patients with markedly high baseline T-cell function. Although neurotoxicity-related blinatumomab dose reduction was a confounding factor for 2 of the 3 patients, the sustained T-cell function throughout the 28-day cycle in these patients suggests the need for further investigation of baseline T-cell function as a predictor of response durability. No association was observed between baseline T-cell function and the amount of previous chemotherapy (supplemental Figure 1C). Preblinatumomab frequencies of B cells suggested comparable antigen loads in those with or without sustained cytotoxicity; B cells were undetectable at later time points (supplemental Figure 1D).
T cells show functional, phenotypic, and transcriptional evidence of dysfunction during continuous blinatumomab. T cells collected at baseline (preblinatumomab), middle (day 14), and end time points (day 28) during a 28-day continuous blinatumomab infusion were analyzed. (A) Left plot: cytotoxicity of T cells. Line graph (right): time point-matched data; each line represents a patient. Green diamonds, cytotoxicity sustained; purple triangles, cytotoxicity not sustained. Vertical bracket: Mann-Whitney test comparison of baseline data. (B-E) Frequency of TSCM, TEMRA, TIM3+, IFN-γ+, TNF-α+, p-mTOR+, p-MEK+, and p-S6+ cells among all T cells. p-S6: marker of mTOR activity. (D-E) Data from intracellular flow cytometry analysis after coculture of T cells and B-ALL cells with CD19/CD3 BiTE antibody. Values relative to control cocultures (positive cells [%]with BiTE − positive [%]without BiTE) are shown. (F) Volcano plot of fold change vs statistical significance from DESeq differential gene expression analysis (day 14 vs day 0). Differentially expressed genes (FDR adjusted P < .15) in dark red. AFF3, a cofactor highly expressed in progenitors of exhausted T cells9; LAYN, MAGEH1, genes related to T-regulatory suppressive function10; LYST, lysosomal trafficking gene associated with T-cell dysfunction.11 Dotted vertical line: −log10 P value cutoff for defining differential expression. (G) Gene set enrichment analysis for T-cell exhaustion (acute lymphocytic choriomeningitis virus [LCMV] vs chronic [exhausted T cells] LCMV), TEMRA (naive T cells vs PD1 low [enriched for TEMRA] T cells), terminally differentiated effector (KLRG1 high [terminal effector] vs KLRG low12), and effector gene sets among genes ranked by day 14 vs day 0 expression. (A-E) Box plots: 25th to 75th percentiles. Whiskers: 1.5 × the interquartile range beyond 25th and 75th percentiles. Thick black horizontal line, median; red triangle, mean; blue circles, individual data points. P value (blue): Friedman test (TSCM, TIM3+, IFN-γ+, and TNF-α+) or 1-way repeated-measures analysis of variance (all others). Horizontal line (red): paired t test or Wilcox test (Holm-Sidak correction for multiple comparisons). ∗P < .05; ∗∗P < .01. N = 10 patients for panels A, D, and E and 11 patients for panels B, C, F, and G. DN, down; FDR, false discovery rate; GS, gene set; IFN-γ, interferon gamma; KLRG, killer cell lectin-like receptor subfamily G member; mTOR, mammalian target of rapamycin; NES, normalized enrichment score; PD1, programmed cell death protein 1; Tfh, T follicular helper; Th1, type 1 helper T cell; TNF-α, tumor necrosis factor alpha.
T cells show functional, phenotypic, and transcriptional evidence of dysfunction during continuous blinatumomab. T cells collected at baseline (preblinatumomab), middle (day 14), and end time points (day 28) during a 28-day continuous blinatumomab infusion were analyzed. (A) Left plot: cytotoxicity of T cells. Line graph (right): time point-matched data; each line represents a patient. Green diamonds, cytotoxicity sustained; purple triangles, cytotoxicity not sustained. Vertical bracket: Mann-Whitney test comparison of baseline data. (B-E) Frequency of TSCM, TEMRA, TIM3+, IFN-γ+, TNF-α+, p-mTOR+, p-MEK+, and p-S6+ cells among all T cells. p-S6: marker of mTOR activity. (D-E) Data from intracellular flow cytometry analysis after coculture of T cells and B-ALL cells with CD19/CD3 BiTE antibody. Values relative to control cocultures (positive cells [%]with BiTE − positive [%]without BiTE) are shown. (F) Volcano plot of fold change vs statistical significance from DESeq differential gene expression analysis (day 14 vs day 0). Differentially expressed genes (FDR adjusted P < .15) in dark red. AFF3, a cofactor highly expressed in progenitors of exhausted T cells9; LAYN, MAGEH1, genes related to T-regulatory suppressive function10; LYST, lysosomal trafficking gene associated with T-cell dysfunction.11 Dotted vertical line: −log10 P value cutoff for defining differential expression. (G) Gene set enrichment analysis for T-cell exhaustion (acute lymphocytic choriomeningitis virus [LCMV] vs chronic [exhausted T cells] LCMV), TEMRA (naive T cells vs PD1 low [enriched for TEMRA] T cells), terminally differentiated effector (KLRG1 high [terminal effector] vs KLRG low12), and effector gene sets among genes ranked by day 14 vs day 0 expression. (A-E) Box plots: 25th to 75th percentiles. Whiskers: 1.5 × the interquartile range beyond 25th and 75th percentiles. Thick black horizontal line, median; red triangle, mean; blue circles, individual data points. P value (blue): Friedman test (TSCM, TIM3+, IFN-γ+, and TNF-α+) or 1-way repeated-measures analysis of variance (all others). Horizontal line (red): paired t test or Wilcox test (Holm-Sidak correction for multiple comparisons). ∗P < .05; ∗∗P < .01. N = 10 patients for panels A, D, and E and 11 patients for panels B, C, F, and G. DN, down; FDR, false discovery rate; GS, gene set; IFN-γ, interferon gamma; KLRG, killer cell lectin-like receptor subfamily G member; mTOR, mammalian target of rapamycin; NES, normalized enrichment score; PD1, programmed cell death protein 1; Tfh, T follicular helper; Th1, type 1 helper T cell; TNF-α, tumor necrosis factor alpha.
With continued blinatumomab exposure, T cells showed enrichment of immunophenotypes reminiscent of terminal differentiation and exhaustion. Flow cytometry analysis of blood samples revealed a progressive decline in the frequency of stem cell memory T cells (TSCM), an elevated fraction of terminally differentiated T cells (effector memory T cells expressing CD45RA, TEMRA) at the middle time point, and an increased proportion of T cells expressing the exhaustion marker TIM3 at the middle and end time points (Figure 1B-C; supplemental Figure 2A-C). Frequencies of TIM3+TIGIT+ and PD1+TIM3+ T cells were increased by the middle time point (supplemental Figure 2D), reflecting immunophenotypes consistent with the upregulation of multiple inhibitory receptors seen in exhausted T cells.13 The progressive increase in absolute lymphocyte count from baseline to end (supplemental Figure 2E), in conjunction with the observed T-cell subset frequencies, supported an expansion of TEMRA and exhaustion immunophenotypes. The longitudinal TSCM, TEMRA, and TIM3+ profiles were largely reflective of changes in the frequencies of CD4+ TSCM, CD8+ TEMRA, and CD8+TIM3+ cells, respectively (supplemental Figure 3A-F). CD8+TIM3+ T cells were predominantly naive (7 patients) or TEMRA/mixed (4 patients) (supplemental Figure 3G), findings consistent with the reported upregulation of TIM3 in naive T cells in adults treated with blinatumomab.14 Patients with sustained cytotoxicity exhibited a higher percentage of effector memory and a lower proportion of naive T cells at baseline than those without sustained cytotoxicity (supplemental Figure 3H).
We assessed ex vivo BiTE-induced activation responses of T cells collected during cIV blinatumomab (supplemental Figure 4A). Multimodal dysfunction marked by impairments in the activation of several TCR signaling pathways and downstream cytokine effectors of cytotoxicity was observed by 14 days of blinatumomab. Interferon gamma (CD8+ T cells) and tumor necrosis factor alpha (CD4+ T cells) production responses declined during cIV blinatumomab (Figure 1D; supplemental Figure 4B-C). CD4+ and CD8+ T cells at the middle and end time points were marked by diminished BiTE-induced upregulation of key TCR signaling pathways (Ras-MEK-ERK and mammalian target of rapamycin; Figure 1E; supplemental Figure 4D-E) essential for optimal proliferation, effector differentiation, and metabolic reprogramming.15 p38-MAPK signaling was unchanged (supplemental Figure 4F).
RNA sequencing (RNA-seq) revealed the upregulation of multiple T-cell exhaustion-related genes at the middle time point. These included immune response regulators (RAB37, CBLB),16,17 checkpoint receptors (CTLA4, HAVCR2 [TIM3]),13 and transcription factors (TOX, MYB, IRF7)18,19 implicated in exhaustion as well as negative regulators of TCR signaling (UBASH3/STS1, SESN2)20,21 (Figure 1F). After 14 days of blinatumomab, the T-cell gene expression profile was enriched for exhaustion,22 TEMRA,23 and effector transcriptional programs (Figure 1G; supplemental Table 3). Consistent with the dynamics of TEMRA and TIM3+ T-cell frequencies observed via flow cytometry (increased at the middle time point followed by a decline by the end time point), T cells at baseline and end time points showed largely similar transcriptomes. Exhausted and terminally differentiated T cells are predisposed to apoptosis24; loss of exhausted T cells via apoptosis could explain the reversion to baseline profiles by the end of the cycle. Furthermore, bulk RNA-seq was performed on resting T cells; single-cell transcriptomics to investigate subpopulation-specific changes masked by bulk heterogeneity and RNA-seq after BiTE-induced activation may reveal the transcriptional programs underlying the dysfunction of these cells.
The combined functional, immunophenotypic, and transcriptional analysis of T cells from serial blood samples represents a key strength of the study. Our data provide insights that could inform strategies to mitigate blinatumomab-related T-cell dysfunction. Anti-TIM3 antibodies and CBL-B depletion restore T-cell function in preclinical models of cancer-related exhaustion, raising the need for functional studies of TIM3 and CBLB as candidate therapeutic targets for blinatumomab-related T-cell exhaustion.13,17 The T-cell dysfunction seen with blinatumomab supports the investigation of cycles with a shorter duration (<28 days) of continuous blinatumomab exposure. Furthermore, our data underscore the need for T-cell studies during subcutaneous blinatumomab, a currently investigational therapy that induces higher continuous drug levels.25 Our study has several limitations. The sample size was small. T cells were studied at limited time points during a single blinatumomab cycle; further studies are needed to assess T-cell function at distant post-cycle time points and during repeat blinatumomab cycles. Although T-cell dysfunction was observed in our cohort, the E1910 trial13 demonstrated improved survival with sequential blinatumomab in adults with MRD-negative B-ALL; thus, studies are needed to investigate whether T-cell dysfunction seen in ex vivo assays correlates with clinical outcomes.
In conclusion, our results demonstrate functional, phenotypic, and transcriptional evidence of T-cell dysfunction and impaired TCR signaling in pediatric patients receiving blinatumomab for B-ALL therapy in remission. Future studies are needed to elucidate the mechanisms leading to T-cell exhaustion and evaluate strategies that preserve T-cell function during blinatumomab therapy.
Acknowledgments: The authors extend their sincere gratitude to all the patients who participated in this study and their families. The authors thank the Flow Cytometry Core of The Saban Research Institute at Children’s Hospital Los Angeles for their assistance with flow cytometry studies. The authors sincerely acknowledge the Children’s Hospital Los Angeles Tumor Registry study personnel (Shahab Asgharzadeh and Rebekah Kennedy) for their contributions to this work. The authors thank Nirali Shah of the National Institutes of Health for her critical review and editorial assistance during the preparation of this manuscript. Figures were created with BioRender.com.
This work was supported by The Blake King Corporation, Malibu Triathlon, and The Saban Research Institute (Core Pilot Program for use of the Flow Cytometry Core) at Children’s Hospital Los Angeles.
Contribution: J.M. designed research, enrolled patients, processed samples, collected data, analyzed and interpreted data, prepared figures, and wrote the manuscript; A.L. processed samples, designed flow cytometry panels, collected data, analyzed and interpreted data, and prepared figures; A. Doan and T.R. extracted clinical data; T.Y.L. designed flow cytometry panels, collected data, and analyzed and interpreted data; L.J. interpreted data; C.P.W. designed flow cytometry panels and processed samples; S.-J.Y. analyzed and interpreted RNA sequencing data; A. Duong collected data; M.V. processed samples and collected data; C.P. supervised the project, designed research, collected data, analyzed and interpreted data, prepared figures, and wrote the manuscript; and all authors reviewed and approved the final manuscript.
Conflict-of-interest disclosure: C.P. reports equity holding in a private company, Pluto Immunotherapeutics, Inc; receiving royalties for technology licensed to Pluto that are unrelated to this study; and spouse being a former employee of Amgen and owning Amgen stock. The remaining authors declare no competing financial interests.
The current affiliation for J.M. is Pediatric Oncology Branch, Cancer for Center Research, National Cancer Institute, National Institutes of Health, Bethesda, MD.
The current affiliation for A.L., S.-J.Y., M.V., and C.P. is Department of Pediatrics, City of Hope Comprehensive Cancer Center, Duarte, CA.
Correspondence: Chintan Parekh, Department of Pediatrics, City of Hope Comprehensive Cancer Center, 1500 East Duarte Rd, Duarte, CA 91010; email: cparekh@coh.org.
References
Author notes
Presented in abstract form at the 66th annual meeting of the American Society of Hematology, San Diego, CA, 7 December 2024.
RNA sequencing data have been deposited in the Gene Expression Omnibus database (accession number GSE294241).
Data are available on request from the corresponding author, Chintan Parekh (cparekh@coh.org).
The full-text version of this article contains a data supplement.

![T cells show functional, phenotypic, and transcriptional evidence of dysfunction during continuous blinatumomab. T cells collected at baseline (preblinatumomab), middle (day 14), and end time points (day 28) during a 28-day continuous blinatumomab infusion were analyzed. (A) Left plot: cytotoxicity of T cells. Line graph (right): time point-matched data; each line represents a patient. Green diamonds, cytotoxicity sustained; purple triangles, cytotoxicity not sustained. Vertical bracket: Mann-Whitney test comparison of baseline data. (B-E) Frequency of TSCM, TEMRA, TIM3+, IFN-γ+, TNF-α+, p-mTOR+, p-MEK+, and p-S6+ cells among all T cells. p-S6: marker of mTOR activity. (D-E) Data from intracellular flow cytometry analysis after coculture of T cells and B-ALL cells with CD19/CD3 BiTE antibody. Values relative to control cocultures (positive cells [%]with BiTE − positive [%]without BiTE) are shown. (F) Volcano plot of fold change vs statistical significance from DESeq differential gene expression analysis (day 14 vs day 0). Differentially expressed genes (FDR adjusted P < .15) in dark red. AFF3, a cofactor highly expressed in progenitors of exhausted T cells9; LAYN, MAGEH1, genes related to T-regulatory suppressive function10; LYST, lysosomal trafficking gene associated with T-cell dysfunction.11 Dotted vertical line: −log10 P value cutoff for defining differential expression. (G) Gene set enrichment analysis for T-cell exhaustion (acute lymphocytic choriomeningitis virus [LCMV] vs chronic [exhausted T cells] LCMV), TEMRA (naive T cells vs PD1 low [enriched for TEMRA] T cells), terminally differentiated effector (KLRG1 high [terminal effector] vs KLRG low12), and effector gene sets among genes ranked by day 14 vs day 0 expression. (A-E) Box plots: 25th to 75th percentiles. Whiskers: 1.5 × the interquartile range beyond 25th and 75th percentiles. Thick black horizontal line, median; red triangle, mean; blue circles, individual data points. P value (blue): Friedman test (TSCM, TIM3+, IFN-γ+, and TNF-α+) or 1-way repeated-measures analysis of variance (all others). Horizontal line (red): paired t test or Wilcox test (Holm-Sidak correction for multiple comparisons). ∗P < .05; ∗∗P < .01. N = 10 patients for panels A, D, and E and 11 patients for panels B, C, F, and G. DN, down; FDR, false discovery rate; GS, gene set; IFN-γ, interferon gamma; KLRG, killer cell lectin-like receptor subfamily G member; mTOR, mammalian target of rapamycin; NES, normalized enrichment score; PD1, programmed cell death protein 1; Tfh, T follicular helper; Th1, type 1 helper T cell; TNF-α, tumor necrosis factor alpha.](https://ash.silverchair-cdn.com/ash/content_public/journal/bloodadvances/9/15/10.1182_bloodadvances.2025015894/2/m_blooda_adv-2025-015894-gr1.jpeg?Expires=1767709357&Signature=OwDQsHS7k06oXWLlulO0UzwvnsiE7KPvRwZarj1UzrcRU~v5MGajhiNUuygo3-SpaUa3f4dPly9XE0B4WgUhCtL-IDQ~88xuywPjfBpYXsrlMvzs2o45nv-6DSJPFm5iWqarXGNSV3ZrxQ4HM2aRdo99xVy7RDy-JMB2bj9E9H0mfladhY6owVLaZxHcedl832vtW6rruULTh3oJXTMm0UEyEEvnrnhRLAokoM~O-krVS~awfAs3x-VYVxenZWTQFOOU4KlzxVm0zCYtuqy4rcwbGu0xdUY9XtJxDuLa1SP8bOODB4Rv3tbxrIypJGhqWic04kJ4KpTW5WQgz7QGBQ__&Key-Pair-Id=APKAIE5G5CRDK6RD3PGA)