Key Points
Naratuximab emtansine has strong antitumor activity even in models with poor outcome genetic lesions or R-CHOP resistance.
PI3Kδ activation, IL-6 overexpression, and CD37 loss are resistance mechanisms to naratuximab emtansine.
Visual Abstract
CD37-directed antibody and cellular-based approaches have shown preclinical and promising early clinical activity. Naratuximab emtansine (Debio 1562; IMGN529) is an antibody-drug conjugate (ADC) incorporating an anti-CD37 monoclonal antibody conjugated to the maytansinoid DM1 as payload, with activity as a single agent and in combination with rituximab in patients with lymphoma. We studied naratuximab emtansine and its free payload in 54 lymphoma models, correlated its activity with CD37 expression, characterized two resistance mechanisms, and identified combination partners providing synergy. The activity, primarily cytotoxic, was more potent in B- than T-cell lymphoma cell lines. After prolonged exposure to the ADC, one diffuse large B-cell lymphoma (DLBCL) cell line developed resistance to the ADC due to the CD37 gene biallelic loss. After CD37 loss, we also observed upregulation of interleukin-6 (IL-6) and related transcripts. Recombinant IL-6 led to resistance. Anti-IL-6 antibody tocilizumab improved the ADC’s cytotoxic activity in CD37+ cells. In a second model, resistance was sustained by a PIK3CD activating mutation, with increased sensitivity to PI3Kδ inhibition and a functional dependence switch from MCL1 to BCL2. Adding idelalisib or venetoclax overcame resistance in the resistant derivative and improved cytotoxic activity in the parental cells. In conclusion, targeting B-cell lymphoma with the naratuximab emtansine showed vigorous antitumor activity as a single agent, which was also observed in models bearing genetic lesions associated with inferior outcomes, such as Myc Proto-Oncogene (MYC) translocations and TP53 inactivation or R-CHOP (rituximab, cyclophosphamide, doxorubicin, Oncovin [vincristine], and prednisone) resistance. Resistant DLBCL models identified active combinations of naratuximab emtansine with drugs targeting IL-6, PI3Kδ, and BCL2.
Introduction
Despite notable progress in recent decades, we still face challenges in achieving a cure for a substantial number of patients with lymphoma.1,2 An example is diffuse large B-cell lymphoma (DLBCL), the most prevalent type of lymphoma.3 More than half of patients with DLBCL can achieve remission, but ∼40% of them experience refractory disease or relapse after an initial positive response.3 Regrettably, the prognosis for many of these cases remains unsatisfactory despite introducing the most recent antibody-based or cellular therapies,3,4 underscoring the importance of innovating new therapeutic strategies and gaining insights into the mechanisms of therapy resistance.
CD37 is a transmembrane glycoprotein belonging to the tetraspanin family, primarily expressed on the surface of immune cells, principally in mature B cells but also at lower levels in T cells, macrophages/monocytes, granulocytes, and dendritic cells.5-8 CD37 plays a crucial role in various immune functions, including B-cell activation, proliferation, and signaling, although its precise role still needs to be fully elucidated. CD37 interacts with multiple molecules, including Spleen Associated Tyrosine Kinase (SYK), Lck/Yes-Related Novel Protein Tyrosine Kinase Proto-Onocogene (LYN), CD19, CD22, Phosphatidylinositol 4,5-Biphosphate 3-Kinase Catalytic Subunit Delta Isoform (PI3Kδ), Phosphatidylinositol-4,5-Bisphosphate 3-Kinase Catalytic Sununit Gamma (PI3Kγ), and different integrins.6-8 In mice, the lack of CD37 is paired with reduced T-cell–dependent antibody-secreting cells and memory B cells, apparently due to the loss of CD37-mediated clustering of α4β1 integrins Very Late Activation Protein 4 Receptor, Alpha 4 Subunit(VLA-4) on germinal center B cells and decreased downstream activation of PI3K/RAC-Alpha Serine/Threonine-Protein Kinase (AKT) signaling and cell survival.5 Reflecting the expression pattern observed in normal lymphocytes, CD37 exhibits elevated expression in all mature B-cell lymphoid neoplasms, including most lymphoma subtypes, and absence in early progenitor cells or terminally differentiated plasma cells.6,8-14 In DLBCL, CD37 expression has been reported between 40% and 90% of cases across multiple studies performed using different antibodies.9,10,14
CD37-directed antibody–based and, more recently, cellular-based approaches have shown preclinical7,10-22 and early promising clinical activity.23-31 Among the CD37-targeting agents, naratuximab emtansine (Debio 1562; IMGN529) is an antibody-drug conjugate (ADC) that incorporates the anti-CD37 humanized immunoglobulin G1 monoclonal antibody K7153A conjugated to the maytansinoid Mertansine (microtubulin inhibitor) (DM1), as payload, via the thioether linker, N-succinimidyl-4-(N-maleimidomethyl)cyclohexane-1-carboxylate.10
Based on the initial in vitro and in vivo evidence of antitumor activity in lymphoma and chronic lymphocytic leukemia (CLL),7,10 naratuximab emtansine entered the clinical evaluation as a single agent. The phase 1 study enrolled 39 patients with relapsed/refractory B-cell lymphoma.26 The overall response rate was 13% across all patients and 22% in patients with DLBCL, including the only observed complete remission (CR).26 In preliminary results of a phase 2 trial exploring the combination of naratuximab emtansine with the anti-CD20 monoclonal antibody rituximab, based on positive preclinical data,16 the overall response rate was 45% in 76 patients with DLBCL (CR, 32%), 57% in 14 patients with follicular lymphoma (CR, 36%), 50% in 4 patients with mantle cell lymphoma (MCL; CR, 50%).30
Here, we studied the pattern of activity of naratuximab emtansine across a large panel of cell lines derived from DLBCL and other lymphoma subtypes and characterized 2 resistance mechanisms to the ADC.
Material and methods
Methods are provided in the online supplemental Materials.
Results
Naratuximab emtansine has strong antitumor activity in lymphoma cell lines
The antitumor activity of naratuximab emtansine was assessed across 54 cell lines (Table 1). The panel comprised mainly models derived from DLBCL cell lines derived from DLBCL of the activated B-cell (ABC) type (ABC-DLBCL, n = 7) or of the germinal center B-cell (GCB) type (GCB-DLBCL, n = 20), as well as MCL (n = 10), marginal zone lymphoma (n = 6), T-cell lymphomas (n = 8), and others (CLL and primary mediastinal large B-cell lymphoma, n = 3; supplemental Table 1). The median 50% inhibitory concentration (IC50) in all the cell lines was 780 pM (95% confidence interval, 263 pM to 11.45 nM). Activity was stronger in B-cell lymphoma cell lines than in T-cell lymphoma cell lines (P < .001; Table 2). No differences were observed among B-cell lymphoma subtypes (Table 2). Among DLBCL cell lines, cell of origin (Table 2) and the presence of B-cell Lymphoma/Leukemia 2 Apoptosis Regulator (BCL2) or MYC translocations did not affect sensitivity to naratuximab emtansine (supplemental Figure 1A-C). At the same time, IC50 values were lower in cell lines bearing a TP53 inactivation (P = .025; supplemental Figure 1D). The observed antiproliferative activity of naratuximab emtansine was mainly cytotoxic. Induction of apoptosis was demonstrated in 33 of 54 lymphoma cell lines (61%; 1 nM naratuximab emtansine) using a caspase 3/7 activation assay (supplemental Table 2). We compared the activity of naratuximab emtansine and its toxin DM1 with what we previously obtained using the in vitro version of R-CHOP (rituximab, cyclophosphamide, doxorubicin, Oncovin [vincristine], and prednisone) on the same cell lines,32 and we did not observe any correlation (supplemental Figure 2).
IC50 values (MTT upon 72 hours of treatment) for naratuximab emtansine, its payload DM1, and CD37 surface levels by FACS
| Cell line . | MTT assay (72 h) . | MTT assay (72 h) . | FACS . | Cell line . | MTT assay (72 h) . | MTT assay (72 h) . | FACS . |
|---|---|---|---|---|---|---|---|
| Naratuximab emtansine IC50, pM . | DM1-me IC50, pM . | CD37/ISO (log2) . | Naratuximab emtansine IC50, pM . | DM1-me IC50, pM . | CD37/ISO (log2) . | ||
| SU-DHL-16 | 100 | 50 | 4.700 | JVM-2 | 400 | 30 | 2.585 |
| WSU-DLCL2 | 10 000 | 40 | 6.190 | Z-138 | 20 000 | 40 | 1.000 |
| SU-DHL-8 | 40 000 | 30 | 2.807 | GRANTA-519 | 780 | 20 | 4.087 |
| SU-DHL-4 | 200 | 150 | 5.977 | JeKo-1 | 30 | 12 | 2.000 |
| SU-DHL-10 | 50 | 25 | 4.858 | MAVER-1 | 800 | 15 | 4.000 |
| DB | 500 | 100 | 6.845 | SP-53 | 780 | 15 | 5.000 |
| OCI-Ly8 | 50 | 50 | 6.248 | MINO | 150 | 8 | 5.672 |
| OCI-Ly18 | 12 000 | 40 | 5.755 | REC-1 | 100 | 100 | 4.087 |
| OCI-Ly19 | 30 000 | 12 | 1.000 | SP-49 | 12 | 12 | 5.615 |
| SU-DHL-5 | 25 | 15 | 4.392 | UPN1 | 5 | 10 | 3.459 |
| OCI-Ly1 | 0.5 | 40 | 2.000 | KARPAS-1718 | 10 | 8 | 4.755 |
| DoHH2 | 30 000 | 30 | 3.170 | SSK41 | 150 | 10 | 3.459 |
| KARPAS-422 | 300 | 30 | 5.954 | VL51 | 20 000 | 40 | 3.000 |
| RC-K8 | 40 000 | 50 | 6.755 | ESKOL | 400 | 20 | 2.807 |
| VAL | 800 | 30 | 6.209 | HAIR-M | 250 | 40 | 2.322 |
| Farage | 40 | 10 | 6.066 | HC-1 | 780 | 30 | 3.700 |
| SU-DHL-6 | 120 | 20 | 4.644 | PCL-12 | 12 000 | 40 | 2.000 |
| Pfeiffer | 50 000 | 40 | 6.883 | MEC-1 | 15 000 | 50 | 2.000 |
| OCI-Ly7 | 50 | 50 | 6.658 | KARPAS-1106-P | 700 | 10 | 5.781 |
| TOLEDO | 15 000 | 50 | 3.459 | FE-PD | 25 000 | 30 | 1.585 |
| SU-DHL-2 | 3 000 | 40 | 5.672 | KARPAS-299 | 40 000 | 10 | 1.000 |
| RIVA | 150 | 30 | 3.170 | L-82 | 20 000 | 10 | 1.000 |
| OCI-Ly3 | 600 | 30 | 5.170 | Ki-JK | 40 000 | 5 | 1.000 |
| OCI-Ly10 | 250 | 15 | 5.833 | SU-DHL-1 | 30 000 | 8 | 0.000 |
| HBL-1 | 50 | 50 | 2.585 | H9 | 15 000 | 70 | 1.000 |
| TMD8 | 8 000 | 30 | 5.781 | HuT-78 | 13 000 | 100 | 1.585 |
| U-2932 | 15 000 | 30 | 4.585 | Mac-1 | 15 000 | 5 | 1.000 |
| Cell line . | MTT assay (72 h) . | MTT assay (72 h) . | FACS . | Cell line . | MTT assay (72 h) . | MTT assay (72 h) . | FACS . |
|---|---|---|---|---|---|---|---|
| Naratuximab emtansine IC50, pM . | DM1-me IC50, pM . | CD37/ISO (log2) . | Naratuximab emtansine IC50, pM . | DM1-me IC50, pM . | CD37/ISO (log2) . | ||
| SU-DHL-16 | 100 | 50 | 4.700 | JVM-2 | 400 | 30 | 2.585 |
| WSU-DLCL2 | 10 000 | 40 | 6.190 | Z-138 | 20 000 | 40 | 1.000 |
| SU-DHL-8 | 40 000 | 30 | 2.807 | GRANTA-519 | 780 | 20 | 4.087 |
| SU-DHL-4 | 200 | 150 | 5.977 | JeKo-1 | 30 | 12 | 2.000 |
| SU-DHL-10 | 50 | 25 | 4.858 | MAVER-1 | 800 | 15 | 4.000 |
| DB | 500 | 100 | 6.845 | SP-53 | 780 | 15 | 5.000 |
| OCI-Ly8 | 50 | 50 | 6.248 | MINO | 150 | 8 | 5.672 |
| OCI-Ly18 | 12 000 | 40 | 5.755 | REC-1 | 100 | 100 | 4.087 |
| OCI-Ly19 | 30 000 | 12 | 1.000 | SP-49 | 12 | 12 | 5.615 |
| SU-DHL-5 | 25 | 15 | 4.392 | UPN1 | 5 | 10 | 3.459 |
| OCI-Ly1 | 0.5 | 40 | 2.000 | KARPAS-1718 | 10 | 8 | 4.755 |
| DoHH2 | 30 000 | 30 | 3.170 | SSK41 | 150 | 10 | 3.459 |
| KARPAS-422 | 300 | 30 | 5.954 | VL51 | 20 000 | 40 | 3.000 |
| RC-K8 | 40 000 | 50 | 6.755 | ESKOL | 400 | 20 | 2.807 |
| VAL | 800 | 30 | 6.209 | HAIR-M | 250 | 40 | 2.322 |
| Farage | 40 | 10 | 6.066 | HC-1 | 780 | 30 | 3.700 |
| SU-DHL-6 | 120 | 20 | 4.644 | PCL-12 | 12 000 | 40 | 2.000 |
| Pfeiffer | 50 000 | 40 | 6.883 | MEC-1 | 15 000 | 50 | 2.000 |
| OCI-Ly7 | 50 | 50 | 6.658 | KARPAS-1106-P | 700 | 10 | 5.781 |
| TOLEDO | 15 000 | 50 | 3.459 | FE-PD | 25 000 | 30 | 1.585 |
| SU-DHL-2 | 3 000 | 40 | 5.672 | KARPAS-299 | 40 000 | 10 | 1.000 |
| RIVA | 150 | 30 | 3.170 | L-82 | 20 000 | 10 | 1.000 |
| OCI-Ly3 | 600 | 30 | 5.170 | Ki-JK | 40 000 | 5 | 1.000 |
| OCI-Ly10 | 250 | 15 | 5.833 | SU-DHL-1 | 30 000 | 8 | 0.000 |
| HBL-1 | 50 | 50 | 2.585 | H9 | 15 000 | 70 | 1.000 |
| TMD8 | 8 000 | 30 | 5.781 | HuT-78 | 13 000 | 100 | 1.585 |
| U-2932 | 15 000 | 30 | 4.585 | Mac-1 | 15 000 | 5 | 1.000 |
IC50 values were calculated using the 4-parameter log-dose calculation, and all values are in pM. Median fluorescence intense levels of surface CD37 were normalized to isotype, and all values from at least 2 independent experiments.
MTT, 3-(4,5-dimethylthiazol-2-yl)-2,5-dimethyltetrazolium bromide.
Antitumor activity of naratuximab emtansine in lymphoma cell lines
| . | No. . | Median IC50, pM . | 95% confidence interval . |
|---|---|---|---|
| B-cell lymphomas | 46 | 450 | 150-800 |
| T-cell lymphomas | 8 | 22 500 | 13 000-40 000 |
| ABC-DLBCL | 7 | 600 | 81-12 800 |
| GCB-DLBCL | 20 | 400 | 56-14 651 |
| MCL | 10 | 275 | 18-794 |
| MZL | 6 | 325 | 24-18 078 |
| CLL | 2 | 13 500 | 12 000-15 000∗ |
| PMBCL | 1 | 700 | n.a. |
| ALCL | 5 | 30 000 | 15 000-40 000∗ |
| SS | 2 | 14 000 | 13 000-15 000∗ |
| PTCL-NOS | 1 | 10 000 | n.a. |
| . | No. . | Median IC50, pM . | 95% confidence interval . |
|---|---|---|---|
| B-cell lymphomas | 46 | 450 | 150-800 |
| T-cell lymphomas | 8 | 22 500 | 13 000-40 000 |
| ABC-DLBCL | 7 | 600 | 81-12 800 |
| GCB-DLBCL | 20 | 400 | 56-14 651 |
| MCL | 10 | 275 | 18-794 |
| MZL | 6 | 325 | 24-18 078 |
| CLL | 2 | 13 500 | 12 000-15 000∗ |
| PMBCL | 1 | 700 | n.a. |
| ALCL | 5 | 30 000 | 15 000-40 000∗ |
| SS | 2 | 14 000 | 13 000-15 000∗ |
| PTCL-NOS | 1 | 10 000 | n.a. |
IC50 values were obtained after 72-hour treatment.
ALCL, anaplastic large-cell lymphoma; MZL, marginal zone lymphoma; n.a., not available; PMBCL, primary mediastinal large B-cell lymphoma; PTCL-NOS, peripheral T-cell lymphoma not otherwise specified; SS, Sezary syndrome.
The upper confidence limit is held at a maximum of samples.
In parallel, we also looked at the activity of DM1, the free payload of the ADC (Table 1). Its median IC50 was 30 pM (95% confidence interval, 20-40 pM), with no differences between B- and T-cell lymphoma origin (supplemental Table 4). Among DLBCL cell lines, no association was seen between sensitivity to DM1 and cell of origin, TP53 status, or BCL2 or MYC translocations (supplemental Figure 3).
There was no correlation between sensitivity to DM1 and to naratuximab emtansine when we considered all 54 B- and T-cell lymphoma cell lines (r = 0.07; P = .6; supplemental Table 3; supplemental Figure 4A). Conversely, a nonsignificant correlation was seen in the subgroup of cell lines derived from B-cell lymphoma (r = 0.28; P = .06; supplemental Figure 4B).
In vitro activity of naratuximab emtansine is correlated to the expression of its target
The surface expression of CD37 was determined for all 54 cell lines by flow cytometry (Table 1). Naratuximab emtansine IC50 values were inversely correlated with its target expression (Pearson correlation r = –0.32; P = .019; Figure 1A). The findings were corroborated using 2 RNA data sets that we had previously obtained on the same panel of cell lines used in this study.33,34 The ADC IC50 values were inversely correlated with CD37 RNA levels, measured in 51 B- and T-cell lymphoma cell lines via a microarray-based technology (Illumina HT-12 arrays; r = –0.5; P = .001; Figure 1B-C) and also when limiting the analysis to B-cell lymphoma cell lines (microarray, n = 43; r = –0.33; P = .03; RNA-Seq, n = 45; r = –0.3; P = .01; Figure 1D-F).
The in vitro cytotoxic activity of naratuximab emtansine correlated with CD37 expression. (A-F) Pearson correlations between naratuximab emtansine activity, measured by IC50 values, and CD37 protein surface expression, measured by FACS in both B- and T-cell lymphomas (A; n = 54); CD37 RNA levels, measured by the 2 different probes on the Illumina HT-12 arrays, in both B- and T-cell lymphomas (B-C; n = 51); or B-cell lymphoma only, measured with the Illumina HT-12 array (D-E; n = 43) or via total RNA-Seq in 45 B-cell lymphomas (F; n = 45). Illumina HT-12 arrays and RNA-seq data were available for 51 and 45 of the 54 cell lines, respectively.
The in vitro cytotoxic activity of naratuximab emtansine correlated with CD37 expression. (A-F) Pearson correlations between naratuximab emtansine activity, measured by IC50 values, and CD37 protein surface expression, measured by FACS in both B- and T-cell lymphomas (A; n = 54); CD37 RNA levels, measured by the 2 different probes on the Illumina HT-12 arrays, in both B- and T-cell lymphomas (B-C; n = 51); or B-cell lymphoma only, measured with the Illumina HT-12 array (D-E; n = 43) or via total RNA-Seq in 45 B-cell lymphomas (F; n = 45). Illumina HT-12 arrays and RNA-seq data were available for 51 and 45 of the 54 cell lines, respectively.
In agreement with the observed higher activity of the ADC in B- than T-cell lymphoma cell lines, B-cell lymphoma cell lines had higher CD37 protein and RNA levels than T-cell lymphomas (P < .001; supplemental Figure 5A-C). No difference in CD37 expression was seen based on TP53 status in DLBCL cell lines, despite the increased activity of naratuximab emtansine in this population of cells (supplemental Figure 5E-G).
To extend the findings of the relevance of CD37 expression for the ADC’s sensitivity to the clinical setting, we first defined GCB- and ABC-DLBCL CD37 gene expression signatures based on the top 100 genes correlated with CD37 in DLBCL clinical specimens (GSE10846 public data set; supplemental Table 4), and we then looked whether they were enriched in the transcripts more expressed in the DLBCL cell lines that were highly sensitive to naratuximab emtansine (IC50 < 800 pM) than in the resistant cell lines (IC50 > 10 nM). In line with what was seen for CD37 itself, supplemental Figure 6 shows that primary resistant cells had lower expression of genes correlated with CD37 in patients with DLBCL, and these were enriched among the transcripts higher in the sensitive cell lines.
Development of DLBCL cell lines with acquired resistance to naratuximab emtansine
To gain insights into potential mechanisms of resistance to naratuximab emtansine, the ADC-sensitive ABC-DLBCL Stanford University-Diffuse Histiocytic Lymphoma-2 (SU-DHL-2) and the GCB-DLBCL SU-DHL-4 were exposed to increasing concentrations of the drug, starting from the IC50, for several months until they acquired resistance to the CD37-targeting ADC. Both cell lines were also kept in culture with no drug exposure. After ∼7 months, the cells kept under the drug developed resistance to naratuximab emtansine. The resistance was demonstrated to be stable by treating the cells after 2 weeks with no drug exposure. The IC50 values of naratuximab emtansine were sevenfold higher in resistant SU-DHL-2 and 11-fold higher in resistant SU-DHL-4 than in their parental cells (Figure 2A,C). Resistance was limited to the ADC and not to its payload DM1 (Figure 2B,D). Multidrug resistance phenotype was excluded by measuring multidrug resistant 1/2 (coded by ABCB1/ABCC2 genes) expression via real-time polymerase chain reaction (supplemental Figure 7). Tetraspanins, including CD37, are enriched in the membrane of exosomes.6 Hence, we investigated whether exosome formation, possibly leading to CD37-targeting ADC trapping, might be involved in the mechanism of resistance. Nonetheless, growth of parental cells in conditioned media taken from the resistant cells or in an exosome-depleted medium did not affect sensitivity to naratuximab emtansine (supplemental Figure 8).
Acquired resistance to naratuximab emtansine in DLBCL cells. (A-D) MTT (3-[4,5-dimethylthiazol-2-yl]-2,5-dimethyltetrazolium bromide) assay (72 hours) in resistant and parental cells of SU-DHL-2 (A-B) and SU-DHL-4 (C-D) lines. Cell proliferation was evaluated in resistant and parental cells for naratuximab emtansine (Debio-1562) (left panels A and C) and its payload alone DM1 (right panels B and D). Bar plots correspond to IC50 values of resistant (red) and parental (blue) lines. (E-G) All data correspond to at least 3 independent experiments. Surface protein expression of CD37 by FACS in parental and naratuximab emtansine–resistant cell lines. ∗P < .05. MTT, 3-(4,5-dimethylthiazol-2-yl)-2,5-dimethyltetrazolium bromide.
Acquired resistance to naratuximab emtansine in DLBCL cells. (A-D) MTT (3-[4,5-dimethylthiazol-2-yl]-2,5-dimethyltetrazolium bromide) assay (72 hours) in resistant and parental cells of SU-DHL-2 (A-B) and SU-DHL-4 (C-D) lines. Cell proliferation was evaluated in resistant and parental cells for naratuximab emtansine (Debio-1562) (left panels A and C) and its payload alone DM1 (right panels B and D). Bar plots correspond to IC50 values of resistant (red) and parental (blue) lines. (E-G) All data correspond to at least 3 independent experiments. Surface protein expression of CD37 by FACS in parental and naratuximab emtansine–resistant cell lines. ∗P < .05. MTT, 3-(4,5-dimethylthiazol-2-yl)-2,5-dimethyltetrazolium bromide.
Loss of CD37 expression due to homozygous loss as a mechanism of resistance to naratuximab emtansine
Resistant and parental cells underwent surface expression of CD37 and CD20 by fluorescence-activated cell sorter (FACS), transcriptome analysis by RNA-Seq, and whole-exome sequencing (WES; supplemental Table 5).
The resistant SU-DHL-2 cells developed a dramatic decrease in the surface expression of CD37 compared with their parental cells, whereas the reduction in SU-DHL-4 was more limited (Figure 2E-G). The SU-DHL-4 resistant models also developed decreased expression of CD20, whereas SU-DHL-2 exhibited higher levels of surface CD20 (supplemental Figure 9A-C). The SU-DHL-4 resistant cells developed reduced sensitivity to rituximab both as a single agent and the combination of naratuximab emtansine plus rituximab, whereas SU-DHL-2 either parental or resistant exhibited no response to rituximab (supplemental Figure 9D-F). Furthermore, the addition of rituximab was cytotoxic and induced strong sub-G0 increase in parental SU-DHL-4 but not in resistant cells (supplemental Figure 9G).
In SU-DHL-2 cells, the downregulation of CD37 at the protein level was paired with a massive downregulation at the RNA level (log-fold change, −12.68; P < .01; false discovery rate < 0.01; supplemental Table 5). WES and real-time polymerase chain reaction demonstrated a complete lack of reads mapping on the CD37 gene, compatible with the occurrence of homozygous loss (supplemental Figure 10; supplemental Table 6). Thus, the resistance to naratuximab emtansine in the SU-DHL-2 models could be ascribed to the loss of its target due to a genetic event.
Activation of PI3Kδ due to gene mutations as a mechanism of resistance to naratuximab emtansine
Transcriptome profiling in the resistant SU-DHL-4 compared with their parental cells showed enrichment of gene sets involved in PI3K signaling, lipid metabolism, and cell death (supplemental Figure 11; supplemental Table 5). Resistant cells exhibited deregulation of the BCL2-family genes (supplemental Figure 12). WES identified a series of mutations in the resistant cells, but only 2 variants were expressed at messenger RNA. One was in the TRANK1 gene, associated with a rare sleep disorder.35 The other one was represented by a heterozygous missense mutation in the PIK3CD gene coding for PI3Kδ (supplemental Table 5). The latter induced a change from asparagine to threonine at the PI3Kδ amino acid 334 (N334T), and it appeared functionally relevant, being labeled as deleterious and possibly damaging according to the Sorting Intolerant From Tolerant (SIFT)36 and PolyPhen-237 algorithms. Moreover, N334T occurred at a hot spot for mutations occurring in individuals affected by activated PI3Kδ syndrome, as well as in DLBCL clinical specimens38-42 (supplemental Figure 13), and was known to determine an increased lipid kinase activity.42 Indeed, elevated levels of both total and p-AKT (Ser473) were observed in the SU-DHL-4 resistant lines (Figure 3A-B; supplemental Figure 14). Due to the observed BCL2 family gene deregulation and PIK3CD gene mutation, we exposed the SU-DHL-4 resistant cells and their parental counterpart to the BCL2 inhibitors venetoclax and sonrotoclax and to the PI3Kδ inhibitors idelalisib and roginolisib. The resistant cells were more sensitive to both BCL2 and PI3Kδ inhibitors than their parental cells. In SU-DHL-2 resistant, we did not appreciate the same increase in sensitivity, consistently with no PI3K/BCL2 deregulation (Figure 3C; supplemental Figure 15). Exposure to idelalisib dramatically decreased the phosphorylation of AKT in resistant cells (Figure 3A-B; supplemental Figure 14). In agreement with the high sensitivity to BCL2 inhibitors, compared with parental cells, the resistant cells presented a mild increase in the levels of p-BCL2(Ser70), which was slightly reduced after exposure to the PI3Kδ inhibitor (Figure 3A-B; supplemental Figure 14).
Secondary resistance to naratuximab emtansine determines elevated p-AKT, p-BCL2, and MCL1 and increased sensitivity to idelalisib and venetoclax, which can also overcome the resistance to the ADC. (A) Immunoblotting for AKT/p-AKT, BCL2/p-BCL2, and MCL1 in SU-DHL-4 parental and resistant. Representative of 2 independent experiments. (B) Data on the bar plots represent the protein quantification (normalized to vinculin and dimethyl sulfoxide [DMSO]). (C) MTT assay (72 hours) in resistant and parental cells of SU-DHL-4 upon increasing doses of venetoclax (upper) or idelalisib (bottom). Bar plots correspond to IC50 values of resistant (red) and parental (blue) lines. ∗P < .05. (D) Annexin-V/PI staining by FACS obtained in naratuximab emtansine–resistant and parental SU-DHL-4 exposed to naratuximab emtansine (625 pM), venetoclax (25 nM), or idelalisib (625 nM). Representative MTT plots showing the combination of naratuximab emtansine with venetoclax (E) or idelalisib (F) in parental (left) and resistant (right) cells of SU-DHL-4. ∗P < .05. PI, Propidium Iodide.
Secondary resistance to naratuximab emtansine determines elevated p-AKT, p-BCL2, and MCL1 and increased sensitivity to idelalisib and venetoclax, which can also overcome the resistance to the ADC. (A) Immunoblotting for AKT/p-AKT, BCL2/p-BCL2, and MCL1 in SU-DHL-4 parental and resistant. Representative of 2 independent experiments. (B) Data on the bar plots represent the protein quantification (normalized to vinculin and dimethyl sulfoxide [DMSO]). (C) MTT assay (72 hours) in resistant and parental cells of SU-DHL-4 upon increasing doses of venetoclax (upper) or idelalisib (bottom). Bar plots correspond to IC50 values of resistant (red) and parental (blue) lines. ∗P < .05. (D) Annexin-V/PI staining by FACS obtained in naratuximab emtansine–resistant and parental SU-DHL-4 exposed to naratuximab emtansine (625 pM), venetoclax (25 nM), or idelalisib (625 nM). Representative MTT plots showing the combination of naratuximab emtansine with venetoclax (E) or idelalisib (F) in parental (left) and resistant (right) cells of SU-DHL-4. ∗P < .05. PI, Propidium Iodide.
Moreover, we observed an increase of apoptotic and sub-G0 cells, indicative of augmented cell death induced by venetoclax and idelalisib (Figure 3D; supplemental Figure 16A). Each of the 2 agents was able to overcome resistance to the ADC when combined with naratuximab emtansine. Moreover, adding venetoclax or idelalisib to the ADC also benefited the parental cells (Figure 3E-F). Furthermore, pretreatment with idelalisib restored sensitivity to naratuximab emtansine in the SU-DHL-4 resistant cells (supplemental Figure 16B-C). To further explore the potential benefit of the combination of naratuximab emtansine with idelalisib or venetoclax, we tested the synergism of these combinations in ABC- and GCB-DLBCL cell lines with different levels of sensitivity to naratuximab emtansine: OCI-Ly10 (ABC; IC50, 250 pM), TMD8 (ABC; IC50, 8 nM), and Pfeiffer (GCB; IC50, 50 nM). Adding idelalisib or venetoclax was beneficial in both ABC (TMD8, OCI-Ly10) and GCB (Pfeiffer) cell lines (supplemental Figure 17).
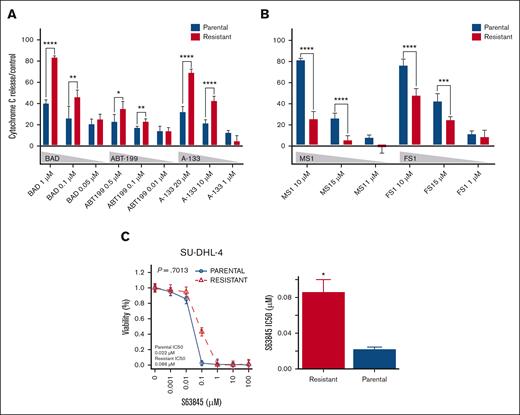
To better understand the functional consequences of the changes at the RNA and protein level of members of the BCL2 family on the acquired sensitivity to venetoclax, we performed BH3 profiling on the SU-DHL-4 resistant and parental cells at baseline or in the presence of idelalisib. The cells resistant to naratuximab emtansine depended on BCL2 and BCLXL to undergo apoptosis, whereas parental cells relied on Myeloid Cell Leukemia 1 Apoptosis Regulator (MCL1) and BFL1 (Figure 4A-B). Furthermore, idelalisib increased BCL2/BCLXL dependence in naratuximab emtansine–resistant cells but not in the parental counterpart cells (supplemental Figure 18). These observations are consistent with the data obtained by treating the resistant and the parental cells with idelalisib. Moreover, the BH3 profiling results were further supported by exposing the SU-DHL-4 resistant and parental cells to the MCL1 inhibitor S63845 (Figure 4C). In contrast to what was observed with BCL2 inhibition, sensitivity to MCL1 inhibition was higher in parental than in the naratuximab emtansine–resistant cells (Figure 4C). Despite their higher dependency on MCL1, the parental cells exhibited elevated MCL1, either RNA or protein levels, which were repressed upon idelalisib treatment (Figure 3A-B; supplemental Figures 12 and 14).
Naratuximab emtansine–resistant and parental SU-DHL-4 differ based on their dependency on antiapoptotic proteins. (A-B) BH3 profiling of naratuximab emtansine–resistant (red bars) and parental SU-DHL-4 (blue bars) exploring the role of BCL2/BCLXL (BAD), BCL2 (ABT-199), and BCLXL (A-133) (A), as well as MCL1 (MS1) and BFL1 (FS1) (B). (C) MTT results were obtained in naratuximab emtansine–resistant and parental SU-DHL-4, which were exposed to increasing concentrations of the MCL1 inhibitor S63845. Bar plots correspond to IC50 values of resistant (red) and parental (blue) lines. ∗P < .05.
Naratuximab emtansine–resistant and parental SU-DHL-4 differ based on their dependency on antiapoptotic proteins. (A-B) BH3 profiling of naratuximab emtansine–resistant (red bars) and parental SU-DHL-4 (blue bars) exploring the role of BCL2/BCLXL (BAD), BCL2 (ABT-199), and BCLXL (A-133) (A), as well as MCL1 (MS1) and BFL1 (FS1) (B). (C) MTT results were obtained in naratuximab emtansine–resistant and parental SU-DHL-4, which were exposed to increasing concentrations of the MCL1 inhibitor S63845. Bar plots correspond to IC50 values of resistant (red) and parental (blue) lines. ∗P < .05.
Finally, we aimed to demonstrate that the PIK3CD N334T mutations drove resistance to naratuximab emtansine in DLBCL models in vitro. To do this, we exploited the CRISPR-Cas9 technology to create the PIK3CD N334T mutation (A>C, at position chr1: 9717597, GRCh38/hg38), detected in the SU-DHL-4 naratuximab emtansine–resistant cells, into the genome of the SU-DHL-4 parental cells. The parental cells bearing the N334T mutation and, as control, parental cells in which we induced a silent mutation in the same locus (N334N; C>T, at position chr1: 9717598) were evaluated for AKT/p(S473)-AKT, BCL2/p(S70)-BCL2, and MCL1 and exposed to naratuximab emtansine. The parental cells with the PIK3CD N334T mutation exhibited very high levels of phosphorylated-AKT (RAC-Alpha Serine/Threonine-Protein Kinase) (p-AKT), a moderate increase of phosphorylated-BCL2 (B-cell Lymphoma/Leumekia 2) (p-BCL2) and MCL1 levels, and survived the high concentration of the ADC, whereas the cells carrying the N334N mutations did not (Figure 5; supplemental Figure 19). Similarly to what was observed in the SU-DHL-4 resistant compared with parental cells, parental with the PIK3CD N334T mutation showed improved sensitivity to idelalisib and venetoclax, whereas the response to the MCL1 inhibitor S63845 was reduced (supplemental Figure 20).
PIK3CD N334T mutation induces p-AKT, p-BCL2, and MCL1 and confers resistance to naratuximab emtansine in the SU-DHL-4 parental cells. (A) Immunoblotting for AKT/p-AKT, BCL2/p-BCL2, and MCL1 in SU-DHL-4 parental and resistant. Representative of 2 independent experiments. (B) Data on the bar plots represent the protein quantification (normalized to vinculin and DMSO). (C) Representative MTT results obtained in parental SU-DHL-4 cells that have undergone genome editing to induce PIK3CD N334T mutation (red) or, as controls, a silent mutation in the same locus (N334N; yellow) and in parental SU-DHL-4 cells undertreated (blue) or transfected with a EGFP only (gray). Bar plot corresponds to IC50 values. ∗P < .05. eGFP, enhanced green fluorescent protein.
PIK3CD N334T mutation induces p-AKT, p-BCL2, and MCL1 and confers resistance to naratuximab emtansine in the SU-DHL-4 parental cells. (A) Immunoblotting for AKT/p-AKT, BCL2/p-BCL2, and MCL1 in SU-DHL-4 parental and resistant. Representative of 2 independent experiments. (B) Data on the bar plots represent the protein quantification (normalized to vinculin and DMSO). (C) Representative MTT results obtained in parental SU-DHL-4 cells that have undergone genome editing to induce PIK3CD N334T mutation (red) or, as controls, a silent mutation in the same locus (N334N; yellow) and in parental SU-DHL-4 cells undertreated (blue) or transfected with a EGFP only (gray). Bar plot corresponds to IC50 values. ∗P < .05. eGFP, enhanced green fluorescent protein.
The effect of the PIK3CD N334T mutation was further explored in additional in vitro models, either derived from ABC (SU-DHL-2) or GCB (OCI-Ly1) DLBCL subtypes. Consistently with the findings in SU-DHL-4 cells, in both cell lines, PIK3CD N334T mutation reduced the sensitivity to naratuximab emtansine but increased the response to idelalisib or venetoclax (supplemental Figure 21). Concordantly, in SU-DHL-2 and OCI-Ly1, the PIK3CD N334T mutation increased p-AKT and, at lesser extent, p-BCL2, which was reduced upon idelalisib exposure (supplemental Figure 22).
Resistance to naratuximab emtansine does not necessarily imply sensitivity to PI3Kδ inhibitors
We observed that the baseline transcriptome of the DLBCL cell lines with primary resistance to naratuximab emtansine–resistant cells was enriched in the gene expression signature derived from the naratuximab emtansine–resistant SU-DHL-4 compared with its parental counterpart (supplemental Figure 23). Furthermore, the transcripts higher in the resistant than in the parental SU-DHL-4 were enriched in the gene expression signatures of sensitivity to PI3K inhibitors43,44 (supplemental Figure 24). However, when we integrated the data of sensitivity to idelalisib that we had previously obtained in the same panel of cell lines33 and now exposed to naratuximab emtansine, we could not demonstrate a correlation between sensitivity to the ADC and sensitivity to the PI3Kδ inhibitor (supplemental Figure 25). Based on RNA-seq data,34 no mutation in the PIK3CD gene was present in Pfeiffer, Tokyo Medical and Dental university 8 (TMD8), and MEC-1, which had high naratuximab emtansine IC50 values and low idelalisib IC50 values.
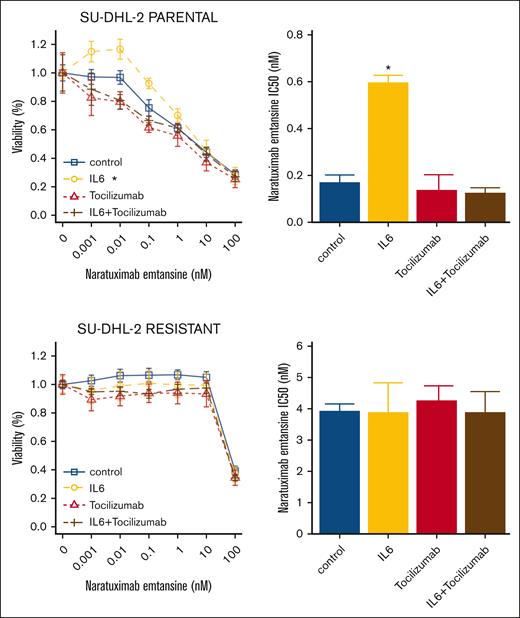
IL-6 can decrease the cytotoxic activity of naratuximab emtansine
We detected an increased expression of interleukin-6 (IL-6; log-fold change, 2.59; P < .01; false discovery rate < 0.01) in CD37– naratuximab emtansine–resistant SU-DHL-2 (supplemental Table 5). Transcripts more expressed in the resistant than parental cells were enriched in genes involved in cell cycle and cell proliferation and MYD88/IL6-signaling (supplemental Table 5). Based on this observation, we assessed whether recombinant IL-6 could reduce the cytotoxic activity of naratuximab emtansine. The parental and resistant SU-DHL-2 cells were treated with the ADC and exposed to recombinant IL-6, plus or minus the anti-IL-6 antibody tocilizumab (Figure 6). In the parental cells, IL-6 decreased the activity of naratuximab emtansine, and adding tocilizumab antagonized the effect. The latter also improved the cytotoxic effect of naratuximab emtansine in the parental cells. Due to the absence of CD37 on the cell surface, no changes were observed in the resistant SU-DHL-2 cells. To further investigate the role of IL-6 in the sensitivity to naratuximab emtansine, additional in vitro models, with or without the expression of (IL-6 receptor) IL6-R, were tested upon recombinant IL-6 and the anti-IL-6 antibody tocilizumab. Those lines with no expression of IL6-R (OCI-Ly1 and OCI-Ly7) showed no advantage upon stimulation with recombinant IL-6 nor after exposure to tocilizumab. However, in accordance with the role of IL-6 in resistance to naratuximab emtansine, recombinant IL-6 decreased sensitivity to naratuximab emtansine in those lines expressing IL6-R, including both ABC (Human diffuse large B-cell lymphoma [HBL-1] and RIVA) and GCB (SU-DHL-10 and (RRID:CVCL_8803) Ontario Cancer Institute - lymphoma-8 [OCI-Ly8]). Similar to what was observed in SU-DHL-2 cells, adding tocilizumab antagonized the effect (supplemental Figure 26).
IL-6 decreases the sensitivity of DLBCL SU-DHL-2 cells to naratuximab emtansine. Parental (top) and resistant (bottom) cells were exposed (72 hours) to increasing concentrations of naratuximab emtansine in the presence or absence of recombinant IL-6 (30 ng/mL), anti-IL-6 antibody tocilizumab (25 μg/mL), and IL-6 plus tocilizumab. Cell viability was determined by MTT assay. Bar plot corresponds to IC50 values. ∗P < .05.
IL-6 decreases the sensitivity of DLBCL SU-DHL-2 cells to naratuximab emtansine. Parental (top) and resistant (bottom) cells were exposed (72 hours) to increasing concentrations of naratuximab emtansine in the presence or absence of recombinant IL-6 (30 ng/mL), anti-IL-6 antibody tocilizumab (25 μg/mL), and IL-6 plus tocilizumab. Cell viability was determined by MTT assay. Bar plot corresponds to IC50 values. ∗P < .05.
Discussion
We have characterized the antitumor activity of CD37-targeting ADC naratuximab emtansine in a large panel of cell lines derived from DLBCL and other lymphomas, (1) identifying subtypes that might benefit more from the treatment, (2) showing a strong correlation with the expression of its target, and (3) showing that its pattern of activity differed from what was achieved with the standard R-CHOP therapy. We also identified 3 potential resistance mechanisms to naratuximab emtansine, driven by the genomic loss of the gene coding for its target, acquisition of somatic mutations activating PI3Kδ, or IL-6 production.
Extending its initial description,10 we demonstrated that naratuximab emtansine has potent in vitro cytotoxic activity in lymphomas, higher in B- than T-cell lymphomas. This aligns with the higher CD37 expression in B- than T-cell lymphomas, as demonstrated by our data and the literature.6,8-14 Moreover, we also observed that the in vitro activity of naratuximab emtansine was indeed correlated with the expression of its target, measured both at the protein level on the cell surface by FACS and at the RNA level using different platforms.
The cytotoxic activity of naratuximab emtansine was maintained in the presence of BCL2 or MYC translocations, and it was not cross-resistant with R-CHOP. The significance of the observed higher in vitro activity of naratuximab emtansine in TP53-inactive DLBCL cases, in the absence of a higher sensitivity to the payload and an increased expression of its target, is unclear. However, as a whole, these observations suggest that naratuximab emtansine, which has a favorable toxicity profile even in patients with severe comorbidities,45 could be explored in patients with DLBCL bearing such lesions, as well as in patients refractory to or relapsed after R-CHOP who are not chimeric antigen receptor T-cell candidates.
To understand the potential mechanisms of resistance that could occur in patients treated with naratuximab emtansine or other anti-CD37–directed therapies, we have kept 2 DLBCL cell lines under drug pressure for many months, leading to 2 different models of resistance to naratuximab emtansine, that nonetheless retain sensitivity to the payload DM1. The SU-DHL-4 resistant model, but not the SU-DHL-2 model, also showed resistance to the combination of the ADC with rituximab, which has promising early clinical data.30
One model, derived from the ABC-DLBCL SU-DHL-2, was sustained by the biallelic loss of the CD37 gene. This observation indicates that lymphoma cells can survive without CD37 expression and agrees with the report of CD37 loss of expression in up to 60% of patients with DLBCL9 and with a possible tumor suppressor role for CD37 itself.46 In mice, the lack of CD37 drives lymphomagenesis, inducing the constitutive activation of the IL-6 signaling pathway.46 Interestingly, after CD37 loss, we also observed an upregulation of IL-6 and other transcripts from MYD88/IL-6 signaling. Moreover, we demonstrated that even IL-6 alone could give resistance to naratuximab emtansine, and adding the anti-IL-6 antibody tocilizumab improves the cytotoxic activity of the ADC in CD37+ cells. Our data further identify IL-6 as a resistance mechanism to multiple treatments.44,47,48 Furthermore, they suggest the benefit of regimens including drugs that interfere with IL-6 signaling and/or production49-52 for CD37– lymphomas with high IL-6 production46 and for CD37+ in combination with CD37-targeting agents.
The second model of resistance, derived from the GCB-DLBCL SU-DHL-4, was sustained by the acquisition of a somatic mutation in the PIK3CD gene coding for PI3Kδ and a transcriptome profile, indeed, characterized by an enrichment of gene sets related to PI3K signaling and dysregulation of the BCL2 family genes. The PIK3CD N334T mutation was annotated as functionally relevant; it occurred in a hot spot for mutations occurring in individuals affected by activated PI3Kδ syndrome41,42 as well as in clinical specimens both from human38,39 and canine DLBCL40; it was functionally proven to give resistance to naratuximab emtansine when introduced in the otherwise naratuximab emtansine–sensitive parental SU-DHL-4 cells and in additional DLBCL models, derived from both ABC (SU-DHL-2) and GCB (OCI-Ly1). Our findings agree with the prosurvival role of activating PI3Kδ signaling downstream to CD37 and its blocking by PI3K inhibition in CLL cells.53 Moreover, the resistant derivative had also become more sensitive to PI3Kδ inhibition and BCL2 inhibition than its parental counterpart. The latter could be explained by the switch from MCL1 dependence in the parental cells to BCL2 dependence in the resistant derivative, as demonstrated functionally by BH3 profiling and by increased p(S70)-BCL2 observed upon the PIK3CD N334T mutation. Notably, adding idelalisib or venetoclax to naratuximab emtansine overcame resistance to the ADC in the resistant derivative. It improved the cytotoxic activity of the ADC in the parental cells, and it was beneficial in additional ABC- and GCB-DLBCL in vitro models. Similar results have been obtained by combining another CD37 targeting agent, the CD37 antibody BI 836826, with idelalisib.54,55 All these results suggest that the combination of naratuximab emtansine with BCL2 inhibitors or with a new generation of PI3Kδ inhibitors might be worthy of clinical evaluation in B-cell lymphoma, particularly in DLBCL.
The clinical relevance of somatic mutations leading to PI3Kδ activation in leading to resistance to naratuximab emtansine and possibly to other CD37-targeting antibody–based therapies will require the analysis of primary samples from clinical trials. We showed that the cell lines most resistant to naratuximab emtansine in our initial screen did not carry PIK3CD mutations, and there was no correlation between sensitivity to the ADC or to idelalisib across 34 B-cell lymphoma cell lines exposed to both compounds.
In conclusion, targeting B-cell lymphoma with the CD37-targeting ADC naratuximab emtansine showed pronounced antitumor activity as a single agent, which is evident also in models bearing genetic lesions associated with inferior outcomes, such as MYC translocations and TP53 inactivation, or resistance to R-CHOP. Our DLBCL resistance models identified active combinations of naratuximab emtansine with drugs targeting IL-6, PI3Kδ, and BCL2.
Acknowledgments
The study was partially supported by institutional research funds from ImmunoGen and the Gelu Foundation (F.B.) and National Institutes of Health (1R01CA266298-01A1; M.S.D.). N.M. was supported by a PhD Fellowship of the National Centre of Competence in Research (NCCR) RNA & Disease, a NCCR funded by the Swiss National Science Foundation (grant numbers 182880 and 205601).
Authorship
Contribution: A.J.A. developed resistant lines, performed experiments, analyzed and interpreted data, performed data mining, prepared figures, and cowrote the manuscript; S.N. performed genetic editing and interpreted data; E.G. performed experiments and analyzed and interpreted data; C.H. performed BH3 profiling; E.C. and C.T. performed experiments; R.P.B. and G.S. performed flow cytometry analyses; L.C. performed data mining; N.M. performed data mining and prepared figures; L.A. analyzed and interpreted data; J.S. and A.C. performed structural modeling of the PI3Kδ complex; A.R. performed genomics experiments; I.K. performed data mining; E.Z., A.S., and D.R. provided advice and edited the manuscript; C.S. and M.S.D. codesigned research and edited the manuscript; F.B. designed the study, interpreted data, and cowrote the manuscript; and all authors approved the final manuscript.
Conflict-of-interest disclosure: A.J.A. reports travel grant from AstraZeneca; and consultancy fees from Pentixapharm. E.G. is an employee of Floratek. C.H. reports honoraria from AbbVie, Janssen, Roche, Gilead, Takeda, and Daiichi; personal fees from AbbVie, Janssen, Roche, Gilead, and Takeda; and research funding from AbbVie and Takeda. C.T. reports travel grant from iOnctura. L.C. reports travel grant from HTG. I.K. and A.S. report institutional funding for clinical trials from Debiopharm, InnoMedica, AbbVie, ADC Therapeutics, Amgen, AstraZeneca, Bayer, Cellestia, Incyte, Loxo Oncology, Merck MSD, Novartis, Pfizer, Philogen, and Roche; institutional funding for consultancy/expert testimony/advisory board from Debiopharm, Janssen, AstraZeneca, Incyte, Eli Lilly, Novartis, Roche, and Loxo Oncology; and travel grant from Incyte and AstraZeneca. E.Z. reports advisory board fees from BeiGene, Bristol Myers Squibb, Curis, Eli/Lilly, Incyte, Janssen, Merck, Miltenyi Biomedicine, and Roche; research support from AstraZeneca, BeiGene, Bristol Myers Squibb/Celgene, Incyte, Janssen, and Roche; and travel grant from BeiGene, Janssen, Gilead, and Roche. D.R. reports honoraria from AstraZeneca, AbbVie, BeiGene, Bristol Myers Squibb/Celgene, and Janssen; and research funding from AstraZeneca, AbbVie, BeiGene, and Janssen. G.S. reports travel grants from Novartis, Celgene, and Roche; consultancy fee from Novartis; scientific advisory board fees from Bayer, Celgene, Janssen, and Novartis; and speaker fees from Gilead. C.S. is an employee of ImmunoGen. M.S.D. has received institutional research funding from AbbVie, AstraZeneca, Ascentage Pharma, Genentech, MEI Pharma, Novartis, Surface Oncology, and TG Therapeutics; and personal consulting income from AbbVie, Adaptive Biosciences, Aptitude Health, Ascentage Pharma, AstraZeneca, BeiGene, Bristol Myers Squibb, Celgene, Curio Science, Eli Lilly, Genentech, Genmab, Janssen, Merck, Nuvalent, Secura Bio, TG Therapeutics, and Takeda. F.B. reports institutional research funds from ADC Therapeutics, Bayer AG, BeiGene, Floratek Pharma, Helsinn, HTG Molecular Diagnostics, Ideogen AG, Idorsia Pharmaceuticals, Immagene, ImmunoGen, Menarini Ricerche, Nordic Nanovector ASA, Oncternal Therapeutics, and Spexis AG; consultancy fees from BIMINI Biotech, Helsinn, and Menarini; advisory board fees to institution from Novartis; expert statements provided to HTG Molecular Diagnostics; and travel grants from Amgen, AstraZeneca, BeiGene, InnoCare, and iOnctura. The remaining authors declare no competing financial interests.
The current affiliation for E.G. is Floratek Pharma, Aubonne, Switzerland.
The current affiliation for C.H. is Centre Hospitalier Universitaire de Montpellier, Montpellier, France.
The current affiliation for I.K. is BigOmics Analytics SA, Lugano, Switzerland.
Correspondence: Francesco Bertoni, Institute of Oncology Research, via Francesco Chiesa 5, 6500 Bellinzona, Switzerland; email: francesco.bertoni@ior.usi.ch.
References
Author notes
A.J.A. and S.N. contributed equally to this study.
Genomic data reported in this article have been deposited in the National Center for Biotechnology Information Gene Expression Omnibus (http://www.ncbi.nlm.nih.gov/geo) database (accession number GSE173984).
The full-text version of this article contains a data supplement.



![Acquired resistance to naratuximab emtansine in DLBCL cells. (A-D) MTT (3-[4,5-dimethylthiazol-2-yl]-2,5-dimethyltetrazolium bromide) assay (72 hours) in resistant and parental cells of SU-DHL-2 (A-B) and SU-DHL-4 (C-D) lines. Cell proliferation was evaluated in resistant and parental cells for naratuximab emtansine (Debio-1562) (left panels A and C) and its payload alone DM1 (right panels B and D). Bar plots correspond to IC50 values of resistant (red) and parental (blue) lines. (E-G) All data correspond to at least 3 independent experiments. Surface protein expression of CD37 by FACS in parental and naratuximab emtansine–resistant cell lines. ∗P < .05. MTT, 3-(4,5-dimethylthiazol-2-yl)-2,5-dimethyltetrazolium bromide.](https://ash.silverchair-cdn.com/ash/content_public/journal/bloodadvances/8/24/10.1182_bloodadvances.2023012291/2/m_blooda_adv-2023-012291-gr2.jpeg?Expires=1763477668&Signature=0r-cjpdwOC~QCp-abr-dtSAAvWUkiesL7ZWbEhw4igobL0ywLRj-2EZWRiy3KZI3Pme74chy6YvtaCJsDVz5yr1wK1RDm8n-Ka3C17qtJhYqerbl2AqZbKOE5I-u3VAa-msyeuwpkL7QMZvuZnOt03H0CPfDRJ7DThllKM29KsqD0CWtru3WaxVcP~0TMD7O5Z6kvDaEcWB3MuFGzK-RV~-mqzEiPZtfFBHn8Lu0JCFCA88wjZVTHea-Cn3ZEtMWtqTYloaoz4ugvnuWXrs5BFjDf56wGqlQFn4w~5eSkdAdMuk7OieKwfUAzNAJJdELRwqn5pOfG3nMqbqZyPRA-A__&Key-Pair-Id=APKAIE5G5CRDK6RD3PGA)

![Secondary resistance to naratuximab emtansine determines elevated p-AKT, p-BCL2, and MCL1 and increased sensitivity to idelalisib and venetoclax, which can also overcome the resistance to the ADC. (A) Immunoblotting for AKT/p-AKT, BCL2/p-BCL2, and MCL1 in SU-DHL-4 parental and resistant. Representative of 2 independent experiments. (B) Data on the bar plots represent the protein quantification (normalized to vinculin and dimethyl sulfoxide [DMSO]). (C) MTT assay (72 hours) in resistant and parental cells of SU-DHL-4 upon increasing doses of venetoclax (upper) or idelalisib (bottom). Bar plots correspond to IC50 values of resistant (red) and parental (blue) lines. ∗P < .05. (D) Annexin-V/PI staining by FACS obtained in naratuximab emtansine–resistant and parental SU-DHL-4 exposed to naratuximab emtansine (625 pM), venetoclax (25 nM), or idelalisib (625 nM). Representative MTT plots showing the combination of naratuximab emtansine with venetoclax (E) or idelalisib (F) in parental (left) and resistant (right) cells of SU-DHL-4. ∗P < .05. PI, Propidium Iodide.](https://ash.silverchair-cdn.com/ash/content_public/journal/bloodadvances/8/24/10.1182_bloodadvances.2023012291/2/m_blooda_adv-2023-012291-gr3de.jpeg?Expires=1763477668&Signature=gvoNO2W8jyrzkVaCTKEODRPLvWuzSvDr4tL180GTimrSR6emSPr2bEpTS1iBmg50rPITkQuMwOxXT270Y-9G1qO0~H1BEC0253t1pfttrsfUY4T40P6WOoCLbMQ6i47f4C4CwvqOHh3kMj98nGrrohcIHRNZ~Xkrvd3HGm0N-WFdxftzkRG8ecW9EAgeUiZACRrl1W3fAGw7Kti0X7A6GezbajLp2LAaKXEed0lr3yBpman5g5P5Jxv2No6M1TTkGTuZm8aegHj3cEAraR99T~lj~p7mr~fpWT0OexEiTSvprBwJLBq3ZImNQiTQQQ9Ri~ayCWXmafq9L3hE5GzJrQ__&Key-Pair-Id=APKAIE5G5CRDK6RD3PGA)