TO THE EDITOR:
We read with interest the article by Cogan et al,1 in which they report that 58% of adults with iron deficiency (ferritin <25μg/L), detected in primary and tertiary care centers across Minnesota, did not achieve resolution (ferritin >50 μg/L) within 3 years. We report similar data from a retrospective observational analysis of a longitudinal female cohort in Western Australia.
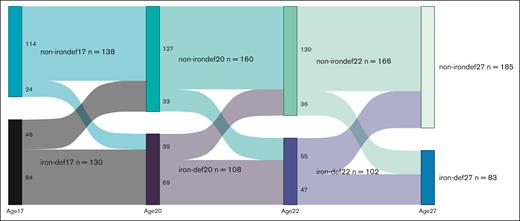
Data were obtained longitudinally from generation 2 of the Raine Study from 2007 until 2019.2 Of 268 women, mean ferritin at age 17 years was 36.5 ± 28.1 μg/L, and 49% were iron deficient (ferritin <30 μg/L), of which 92% were nonanemic. By age 20 years, mean ferritin was 43.4 ± 33.9 μg/L, and 40% were iron deficient. At age 22 years, mean ferritin was 44.2 ± 30.7 μg/L, with 38% being iron deficient. By age 27 years, mean ferritin was 57.2 ± 50.9 μg/L, and 31% of women were iron deficient (see figure).
Longitudinal changes in iron status. Data are reported as number of iron-deficient data sets (ferritin <30 μg/L) and non–iron-deficient data sets (ferritin ≥30 μg/L) at ages 17, 20, 22, and 27 years.
Longitudinal changes in iron status. Data are reported as number of iron-deficient data sets (ferritin <30 μg/L) and non–iron-deficient data sets (ferritin ≥30 μg/L) at ages 17, 20, 22, and 27 years.
Of 108 women with iron deficiency aged 17 years, 84 (78%) remained iron deficient by age 20 years, 58 women (53%) remained iron deficient till the age 22 years, and 35 women (32%) remained iron deficient through the age 27 years. New cases of iron deficiency developed between the ages 17 and 20 years in 24 of 138 women (17%), between the ages 20 and 22 years in 33 of 160 women (21%), and between the ages 22 and 27 years in 36 of 166 women (22%).
Iron deficiency appeared more common during the younger years. Similar to the US data,1 sustained iron deficiency was more common in the younger cohort, with over half of those with iron deficiency at age 17 years being iron deficient after 5 years. The cross-sectional study design limits our insight into the diagnosis and management of those with iron deficiency, however, our data combined highlight that unresolved iron deficiency is a common problem, particularly in younger adults, in both the United States and Australia.
Acknowledgments: The authors acknowledge the Raine Study participants and their families for their ongoing participation in the study and the Raine Study team for study coordination and data collection. The authors also thank the National Health and Medical Research Council (NHMRC) and the Raine Medical Research Foundation for their long-term contribution to funding the study over the last 30 years.
The core management of the Raine Study is funded by The University of Western Australia, Curtin University, Telethon Kids Institute, Women and Infants Research Foundation, Edith Cowan University, Murdoch University, and The University of Notre Dame Australia. Furthermore, the authors thank King Edward Memorial Hospital, Royal Perth Hospital, Telethon Kids Institute, WA Health (Future Health WA G06302 [Eastwood et al]), the National Heart Foundation (Mori et al, ID 102301), and the NHMRC (program grants, Stanley et al, ID 353514; Beilin et al, ID 403981; Adams et al, ID 634445; Mori et al, ID 1102106; and Eastwood et al, ID 1109057) for their roles in data collection and analysis specific to this study.
Contribution: B.M., J.L., and T.R. investigated research; M.A. conducted data analysis; and B.M prepared the manuscript.
Conflict-of-interest disclosure: The authors declare no competing financial interests.
Correspondence: Beth MacLean, The University of Western Australia, 35 Stirling Highway, Crawley, WA 6009, Australia; email: Beth.MacLean@research.uwa.edu.au.
References
Author notes
Data relating to the study are available upon reasonable request from the corresponding author, Beth MacLean (Beth.MacLean@research.uwa.edu.au), subject to approval from the Raine Study.