Key Points
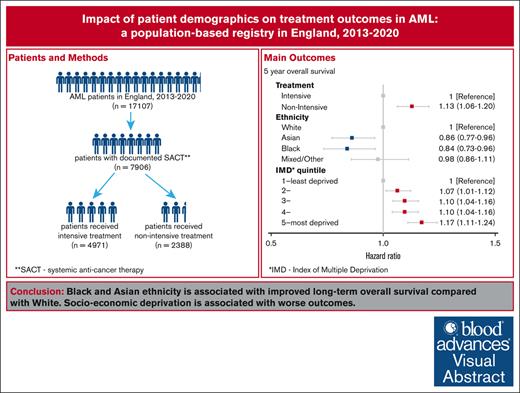
We report 1- and 5-year survival after AML diagnosis, and 30-day mortality after systemic treatments, using the English national registry.
Ethnicity and socioeconomic status affected outcomes in AML; 30-day mortality was higher for patients receiving intensive chemotherapy.
Visual Abstract
We report 1- and 5-year survival after acute myeloid leukemia (AML) diagnosis and early mortality within 30 days of systemic anticancer therapy (SACT) treatments, using national cancer registry data in England. Patients aged 18 to 99 years diagnosed between 2013 and 2020 were included. Overall survival (OS) was calculated using Kaplan-Meier methodology, and adjusted hazard ratios (aHRs; adjusted for intensity of treatment, age at diagnosis, sex, ethnicity, socioeconomic deprivation, comorbidity, and year of diagnosis) using Cox proportional hazards regression. Odds of 30-day mortality (adjusted odds ratios [aORs], adjusted for aforementioned characteristics), along with performance status and body mass index, were calculated using logistic regression. Among 17 107 patients identified, older age and comorbidity were associated with worse survival. Asian and Black patients had better survival than White patients: 5-year OS of 34.6%, 29.7%, and 17.8%, respectively; aHR of 0.86; (95% confidence interval [CI], 0.77-0.96) Asian vs White, and 0.84 (95% CI, 0.73-0.96) Black vs White. Socioeconomic deprivation was associated with worse survival. Overall, 7906 (46.2%) patients were documented as having received SACT. Thirty-day mortality was lower for patients receiving intensive rather than nonintensive SACT. After adjustment for cofactors, the risk was higher in those treated intensively (aOR, 0.74; 95% CI, 0.60-0.92). We show that ethnicity and socioeconomic status affects outcomes in AML. Further work is needed to understand how these effects may differ in different health care settings, and whether this because of effects on disease biology, responsiveness to treatment, or drug toxicity. Selection of intensive vs nonintensive treatment should be based on individual patient factors, balancing improved long-term survival against higher early mortality.
Introduction
Acute myeloid leukemia (AML) is the most common form of acute leukemia and may present at any age. Randomized controlled trials have provided the basis for testing interventions including chemotherapy aimed at cure and improving outcomes. However, patients recruited into trials may not be representative of the broad AML population, and patients may have multiple comorbidities affecting treatment choices, whereas those who present extremely unwell at diagnosis may be unable to tolerate intensive therapy. AML is among the most difficult cancers to treat with curative intent,1 given the need for intensive chemotherapy, which is, in turn, associated with a high early mortality, because of the underlying disease and complications of treatment.2 Many patients who are frail are only offered chemotherapy with palliative intent.3 The impact of ethnicity has not been well described, although studies from the United States suggest that Black ethnicity may be associated with a differing incidence of molecular subtypes of AML and worse outcomes even in genetically favorable-risk disease.4-7
The aim of this study was to report the outcomes in a national cohort of adult de novo AML using the population-based cancer registry in a publicly funded National Health Service (NHS) in England. Specific objectives of this real-world data set study were to (1) report 1- and 5-year overall survival (OS) and evaluate patient sociodemographics associated with survival after AML diagnosis; and (2) establish benchmarks of early mortality, within 30 days of systemic anticancer therapy (SACT), and explore associations between patient sociodemographics and the likelihood of dying ≤30 days after the initial SACT.
Methods
Data sources
Cancer data collection from all health institutions is a statutory requirement in NHS organizations in England. The National Cancer Registration Dataset (NCRD), 2013-2020; and the SACT Dataset, 2013-2021 were used for this study. The NCRD holds the population-based national cancer registry for England and is linked to other data sets for analysis purposes.8 The SACT Dataset is a population-based resource of all systemic treatments delivered in secondary and tertiary settings in England.9
Data for this study were collected and analyzed under the National Disease Registries Directions 2021, made in accordance with sections 254(1) and 254(6) of the 2012 Health and Social Care Act. Further ethical approval for this study was not required per the definition of research according to the United Kingdom Policy Framework for Health and Social Care Research.
Study population
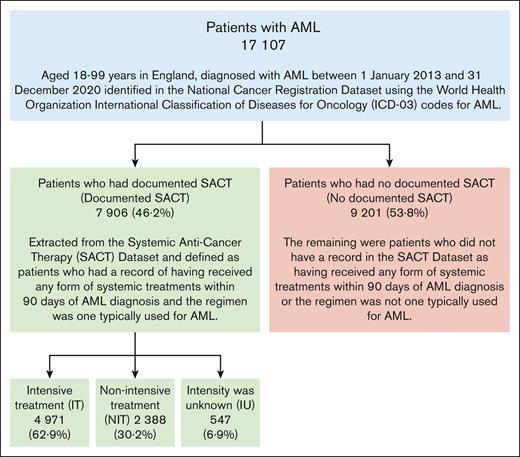
Patients aged 18-99 years in England, diagnosed with AML between 1 January 2013 and 31 December 2020, were identified in the NCRD using the World Health Organization International Classification of Diseases for Oncologycodes (supplemental Table 1).10 Any patient identified as having undergone a transformation event between 2013 and 2020 from a different type of hematological malignancy diagnosed between 1995 and 2020 was excluded from this analysis.11
The initial SACT (“Documented SACT”) data were extracted from the SACT Dataset and defined as those receiving systemic AML treatments within 90 days of AML diagnosis. The remaining patients were defined as “No Documented SACT.” SACT treatments were reviewed by a 2-person expert panel and defined as either intensive treatment (IT), nonintensive treatment (NIT), or intensity unknown (IU) (supplemental Appendix 1; supplemental Table 2).
Variables
Patient characteristics were analyzed after extraction from the NCRD or the SACT Datasets, including intensity of SACT treatment, age at diagnosis, sex, ethnicity (patient-reported from their health records), socioeconomic status (index of multiple deprivation [IMD]), comorbidity (total Charlson score), year of diagnosis, performance status (PS), and body mass index (BMI). Patients were grouped into 5 age groups as per the International Cancer Survival Standard.12 IMD is the official measure of relative deprivation for small areas in England.13 Patients were assigned to 1 of 5 quintiles, from least deprived to most deprived, according to their postcode of residence at diagnosis. The total Charlson score14 was collated from the Health Episode Statistics Datasets (HES)15 and based on lookback of 27 to 3 months before the AML diagnosis. The PS and BMI data were collected at the start of a regimen and were only available for patients documented as receiving SACT. PS was recorded using the Eastern Cooperative Oncology Group (ECOG) scale.16 BMI was categorized into underweight (BMI <18.5 kg/m2), normal weight (18.5 to <25.0 kg/m2), overweight (25.0 to <30.0 kg/m2), or obese (≥30.0 kg/m2).17 Occurrence of allogeneic stem cell transplant was identified using a combination of HES and SACT data.
Statistical analysis
Median survival time and 1- and 5-year overall survival (OS) with 95% confidence interval (95% CI) were calculated using Kaplan-Meier methodology from date of diagnosis of AML to the earliest date of death, fifth anniversary of diagnosis with AML, or loss to follow-up at the Personal Demographics Service,18 or the censor date on 31 December 2022. All patients had a full follow-up for at least 2 years. Unadjusted and adjusted hazard ratios (aHRs) with 95% CIs for 1- and 5-year OS were generated using Cox proportional hazards regression, with aHRs adjusted for intensity of SACT, age at diagnosis, sex, ethnicity, deprivation, comorbidity, and year of diagnosis. Information of patients’ remission status before transplant was lacking so allogeneic stem cell transplant was not included in multivariate analyses. Early mortality (within 30 days of the initial SACT) was calculated for the documented SACT. Unadjusted and adjusted odds ratios (aORs) with 95% CIs were generated using logistic regression to examine how patient sociodemographics were associated with the likelihood of dying within ≤30 days, with aORs adjusted for characteristics listed above, along with PS and BMI.
All statistical analyses were performed using Stata, version 17.0 (StataCorp LLC).
Results
Characteristics of patients included in analysis
We identified 17 107 patients diagnosed with de novo AML in 2013 to 2020, of whom 7906 (46.2%) were documented patients with SACT (Figure 1; Table 1; supplemental Table 3). The annual incidence of AML cases ranged from 2086 to 2210, and there was no temporal trend across 2013 to 2020 (P = .95). The median age at diagnosis of the overall cohort was 72 years. There were more males than females (56.3% vs 43.7%, P < .001), and White ethnicity was the most common (88.8%). Patients of non-White ethnicity were significantly younger than White patients: White patient mean age at diagnosis, 69.7 years (standard deviation [SD], 15.5) vs Asian 57.7 (SD, 19.4), P < .001; White vs Black 60.5 (SD, 17.4), P < .001; White vs mixed/other 55.6 (SD, 18.2), P < .001. Overall, 4.2% had incomplete data on ethnicity and the proportion was similar across all levels of treatment intensity and age groups. A higher proportion of Black and Asian patients were resident in the deprived areas (IMD quintiles 4 and 5) than in the nondeprived areas (quintiles 1 and 2): Asian 56.7% vs 24.2%, P < .001; Black 70.1% vs 12.3%, P < .001; mixed/other 46.4% vs 34.7%, P = .045; White 33.9% vs 45.1%, P < .001; overall, 35.3% vs 43.8%, P < .001. Patients from more deprived areas were overrepresented among patients aged 18 to 54 years (least deprived quintile [17.9%] vs most deprived quintile [22.6%], P < .05).
Characteristics of adults, aged 18 to 99 years, diagnosed with AML, National Cancer Registration Dataset 2013-2020
| . | IT (n = 4971) . | NIT (n = 2388) . | IU (n = 547) . | Documented SACT (total of IT, NIT, and IU) (n = 7906) . | No documented SACT (n = 9201) . | Total (n = 17 107) . |
|---|---|---|---|---|---|---|
| Median age at diagnosis, y (IQR) | 59 (48-67) | 76 (71-80) | 72 (62-78) | 66 (54-74) | 77 (68-84) | 72 (61-81) |
| Mean age at diagnosis, y (SD) | 56.0 (14.5) | 74.8 (8.6) | 68.5 (15.2) | 62.6 (15.7) | 74.3 (14.2) | 68.9 (16.0) |
| Age at diagnosis, y | ||||||
| 18-54 | 1914 (38.5%) | 61 (2.6%) | 84 (15.4%) | 2059 (26.0%) | 893 (9.7%) | 2952 (17.3%) |
| 55-64 | 1341 (27.0%) | 141 (5.9%) | 76 (13.9%) | 1558 (19.7%) | 863 (9.4%) | 2421 (14.2%) |
| 65-74 | 1489 (30.0%) | 831 (34.8%) | 149 (27.2%) | 2469 (31.2%) | 2012 (21.9%) | 4481 (26.2%) |
| 75-84 | 218 (4.4%) | 1150 (48.2%) | 194 (35.5%) | 1562 (19.8%) | 3270 (35.5%) | 4832 (28.2%) |
| 85-99 | 9 (0.2%) | 205 (8.6%) | 44 (8.0%) | 258 (3.3%) | 2163 (23.5%) | 2421 (14.2%) |
| Sex | ||||||
| Female | 2231 (44.9%) | 945 (39.6%) | 242 (44.2%) | 3418 (43.2%) | 4066 (44.2%) | 7484 (43.7%) |
| Male | 2740 (55.1%) | 1443 (60.4%) | 305 (55.8%) | 4488 (56.8%) | 5135 (55.8%) | 9 623 (56.3%) |
| Ethnicity | ||||||
| White | 4253 (85.6%) | 2199 (92.1%) | 496 (90.7%) | 6948 (87.9%) | 8247 (89.6%) | 15 195 (88.8%) |
| Asian | 230 (4.6%) | 44 (1.8%) | 15 (2.7%) | 289 (3.7%) | 231 (2.5%) | 520 (3.0%) |
| Black | 126 (2.5%) | 32 (1.3%) | 11 (2.0%) | 169 (2.1%) | 139 (1.5%) | 308 (1.8%) |
| Mixed/other | 204 (4.1%) | 31 (1.3%) | 7 (1.3%) | 242 (3.1%) | 118 (1.3%) | 360 (2.1%) |
| Unknown | 158 (3.2%) | 82 (3.4%) | 18 (3.3%) | 258 (3.3%) | 466 (5.1%) | 724 (4.2%) |
| IMD quintile | ||||||
| 1 (least deprived) | 1045 (21.0%) | 576 (24.1%) | 146 (26.7%) | 1767 (22.4%) | 1980 (21.5%) | 3 747 (21.9%) |
| 2 | 1063 (21.4%) | 552 (23.1%) | 118 (21.6%) | 1733 (21.9%) | 2005 (21.8%) | 3 738 (21.9%) |
| 3 | 1025 (20.6%) | 487 (20.4%) | 109 (19.9%) | 1621 (20.5%) | 1957 (21.3%) | 3 578 (20.9%) |
| 4 | 956 (19.2%) | 438 (18.3%) | 91 (16.6%) | 1485 (18.8%) | 1766 (19.2%) | 3 251 (19.0%) |
| 5 (most deprived) | 882 (17.7%) | 335 (14.0%) | 83 (15.2%) | 1300 (16.4%) | 1493 (16.2%) | 2 793 (16.3%) |
| Comorbidity (total Charlson score) | ||||||
| 0 | 4416 (88.8%) | 1711 (71.6%) | 439 (80.3%) | 6566 (83.1%) | 6344 (68.9%) | 12 910 (75.5%) |
| 1 | 316 (6.4%) | 289 (12.1%) | 55 (10.1%) | 660 (8.3%) | 1154 (12.5%) | 1 814 (10.6%) |
| 2 | 160 (3.2%) | 189 (7.9%) | 24 (4.4%) | 373 (4.7%) | 822 (8.9%) | 1 195 (7.0%) |
| ≥3 | 79 (1.6%) | 199 (8.3%) | 29 (5.3%) | 307 (3.9%) | 881 (9.6%) | 1 188 (6.9%) |
| Year of diagnosis | ||||||
| 2013 | 446 (9.0%) | 153 (6.4%) | 107 (19.6%) | 706 (8.9%) | 1467 (15.9%) | 2 173 (12.7%) |
| 2014 | 572 (11.5%) | 198 (8.3%) | 71 (13.0%) | 841 (10.6%) | 1322 (14.4%) | 2 163 (12.6%) |
| 2015 | 624 (12.6%) | 256 (10.7%) | 58 (10.6%) | 938 (11.9%) | 1272 (13.8%) | 2 210 (12.9%) |
| 2016 | 619 (12.5%) | 291 (12.2%) | 49 (9.0%) | 959 (12.1%) | 1167 (12.7%) | 2 126 (12.4%) |
| 2017 | 656 (13.2%) | 347 (14.5%) | 54 (9.9%) | 1057 (13.4%) | 1097 (11.9%) | 2 154 (12.6%) |
| 2018 | 714 (14.4%) | 361 (15.1%) | 25 (4.6%) | 1100 (13.9%) | 1000 (10.9%) | 2 100 (12.3%) |
| 2019 | 735 (14.8%) | 351 (14.7%) | 55 (10.1%) | 1141 (14.4%) | 954 (10.4%) | 2 095 (12.2%) |
| 2020 | 605 (12.2%) | 431 (18.0%) | 128 (23.4%) | 1164 (14.7%) | 922 (10.0%) | 2 086 (12.2%) |
| ECOG PS score∗ | ||||||
| 0 | 1802 (36.3%) | 487 (20.4%) | 90 (16.5%) | 2379 (30.1%) | ||
| 1 | 1085 (21.8%) | 841 (35.2%) | 148 (27.1%) | 2074 (26.2%) | ||
| 2 | 206 (4.1%) | 306 (12.8%) | 33 (6.0%) | 545 (6.9%) | ||
| 3/4 | 99 (2.0%) | 90 (3.8%) | 15 (2.7%) | 204 (2.6%) | ||
| Unknown | 1779 (35.8%) | 664 (27.8%) | 261 (47.7%) | 2704 (34.2%) | ||
| BMI∗ | ||||||
| Underweight (<18.5 kg/m2) | 96 (1.9%) | 47 (2.0%) | 11 (2.0%) | 154 (1.9%) | ||
| Normal weight (18.5 to <25.0 kg/m2) | 1501 (30.2%) | 596 (25.0%) | 109 (19.9%) | 2206 (27.9%) | ||
| Overweight (25.0 to <30.0 kg/m2) | 1586 (31.9%) | 654 (27.4%) | 138 (25.2%) | 2378 (30.1%) | ||
| Obese (≥30.0 kg/m2) | 1236 (24.9%) | 497 (20.8%) | 79 (14.4%) | 1812 (22.9%) | ||
| Unknown | 552 (11.1%) | 594 (24.9%) | 210 (38.4%) | 1356 (17.2%) |
| . | IT (n = 4971) . | NIT (n = 2388) . | IU (n = 547) . | Documented SACT (total of IT, NIT, and IU) (n = 7906) . | No documented SACT (n = 9201) . | Total (n = 17 107) . |
|---|---|---|---|---|---|---|
| Median age at diagnosis, y (IQR) | 59 (48-67) | 76 (71-80) | 72 (62-78) | 66 (54-74) | 77 (68-84) | 72 (61-81) |
| Mean age at diagnosis, y (SD) | 56.0 (14.5) | 74.8 (8.6) | 68.5 (15.2) | 62.6 (15.7) | 74.3 (14.2) | 68.9 (16.0) |
| Age at diagnosis, y | ||||||
| 18-54 | 1914 (38.5%) | 61 (2.6%) | 84 (15.4%) | 2059 (26.0%) | 893 (9.7%) | 2952 (17.3%) |
| 55-64 | 1341 (27.0%) | 141 (5.9%) | 76 (13.9%) | 1558 (19.7%) | 863 (9.4%) | 2421 (14.2%) |
| 65-74 | 1489 (30.0%) | 831 (34.8%) | 149 (27.2%) | 2469 (31.2%) | 2012 (21.9%) | 4481 (26.2%) |
| 75-84 | 218 (4.4%) | 1150 (48.2%) | 194 (35.5%) | 1562 (19.8%) | 3270 (35.5%) | 4832 (28.2%) |
| 85-99 | 9 (0.2%) | 205 (8.6%) | 44 (8.0%) | 258 (3.3%) | 2163 (23.5%) | 2421 (14.2%) |
| Sex | ||||||
| Female | 2231 (44.9%) | 945 (39.6%) | 242 (44.2%) | 3418 (43.2%) | 4066 (44.2%) | 7484 (43.7%) |
| Male | 2740 (55.1%) | 1443 (60.4%) | 305 (55.8%) | 4488 (56.8%) | 5135 (55.8%) | 9 623 (56.3%) |
| Ethnicity | ||||||
| White | 4253 (85.6%) | 2199 (92.1%) | 496 (90.7%) | 6948 (87.9%) | 8247 (89.6%) | 15 195 (88.8%) |
| Asian | 230 (4.6%) | 44 (1.8%) | 15 (2.7%) | 289 (3.7%) | 231 (2.5%) | 520 (3.0%) |
| Black | 126 (2.5%) | 32 (1.3%) | 11 (2.0%) | 169 (2.1%) | 139 (1.5%) | 308 (1.8%) |
| Mixed/other | 204 (4.1%) | 31 (1.3%) | 7 (1.3%) | 242 (3.1%) | 118 (1.3%) | 360 (2.1%) |
| Unknown | 158 (3.2%) | 82 (3.4%) | 18 (3.3%) | 258 (3.3%) | 466 (5.1%) | 724 (4.2%) |
| IMD quintile | ||||||
| 1 (least deprived) | 1045 (21.0%) | 576 (24.1%) | 146 (26.7%) | 1767 (22.4%) | 1980 (21.5%) | 3 747 (21.9%) |
| 2 | 1063 (21.4%) | 552 (23.1%) | 118 (21.6%) | 1733 (21.9%) | 2005 (21.8%) | 3 738 (21.9%) |
| 3 | 1025 (20.6%) | 487 (20.4%) | 109 (19.9%) | 1621 (20.5%) | 1957 (21.3%) | 3 578 (20.9%) |
| 4 | 956 (19.2%) | 438 (18.3%) | 91 (16.6%) | 1485 (18.8%) | 1766 (19.2%) | 3 251 (19.0%) |
| 5 (most deprived) | 882 (17.7%) | 335 (14.0%) | 83 (15.2%) | 1300 (16.4%) | 1493 (16.2%) | 2 793 (16.3%) |
| Comorbidity (total Charlson score) | ||||||
| 0 | 4416 (88.8%) | 1711 (71.6%) | 439 (80.3%) | 6566 (83.1%) | 6344 (68.9%) | 12 910 (75.5%) |
| 1 | 316 (6.4%) | 289 (12.1%) | 55 (10.1%) | 660 (8.3%) | 1154 (12.5%) | 1 814 (10.6%) |
| 2 | 160 (3.2%) | 189 (7.9%) | 24 (4.4%) | 373 (4.7%) | 822 (8.9%) | 1 195 (7.0%) |
| ≥3 | 79 (1.6%) | 199 (8.3%) | 29 (5.3%) | 307 (3.9%) | 881 (9.6%) | 1 188 (6.9%) |
| Year of diagnosis | ||||||
| 2013 | 446 (9.0%) | 153 (6.4%) | 107 (19.6%) | 706 (8.9%) | 1467 (15.9%) | 2 173 (12.7%) |
| 2014 | 572 (11.5%) | 198 (8.3%) | 71 (13.0%) | 841 (10.6%) | 1322 (14.4%) | 2 163 (12.6%) |
| 2015 | 624 (12.6%) | 256 (10.7%) | 58 (10.6%) | 938 (11.9%) | 1272 (13.8%) | 2 210 (12.9%) |
| 2016 | 619 (12.5%) | 291 (12.2%) | 49 (9.0%) | 959 (12.1%) | 1167 (12.7%) | 2 126 (12.4%) |
| 2017 | 656 (13.2%) | 347 (14.5%) | 54 (9.9%) | 1057 (13.4%) | 1097 (11.9%) | 2 154 (12.6%) |
| 2018 | 714 (14.4%) | 361 (15.1%) | 25 (4.6%) | 1100 (13.9%) | 1000 (10.9%) | 2 100 (12.3%) |
| 2019 | 735 (14.8%) | 351 (14.7%) | 55 (10.1%) | 1141 (14.4%) | 954 (10.4%) | 2 095 (12.2%) |
| 2020 | 605 (12.2%) | 431 (18.0%) | 128 (23.4%) | 1164 (14.7%) | 922 (10.0%) | 2 086 (12.2%) |
| ECOG PS score∗ | ||||||
| 0 | 1802 (36.3%) | 487 (20.4%) | 90 (16.5%) | 2379 (30.1%) | ||
| 1 | 1085 (21.8%) | 841 (35.2%) | 148 (27.1%) | 2074 (26.2%) | ||
| 2 | 206 (4.1%) | 306 (12.8%) | 33 (6.0%) | 545 (6.9%) | ||
| 3/4 | 99 (2.0%) | 90 (3.8%) | 15 (2.7%) | 204 (2.6%) | ||
| Unknown | 1779 (35.8%) | 664 (27.8%) | 261 (47.7%) | 2704 (34.2%) | ||
| BMI∗ | ||||||
| Underweight (<18.5 kg/m2) | 96 (1.9%) | 47 (2.0%) | 11 (2.0%) | 154 (1.9%) | ||
| Normal weight (18.5 to <25.0 kg/m2) | 1501 (30.2%) | 596 (25.0%) | 109 (19.9%) | 2206 (27.9%) | ||
| Overweight (25.0 to <30.0 kg/m2) | 1586 (31.9%) | 654 (27.4%) | 138 (25.2%) | 2378 (30.1%) | ||
| Obese (≥30.0 kg/m2) | 1236 (24.9%) | 497 (20.8%) | 79 (14.4%) | 1812 (22.9%) | ||
| Unknown | 552 (11.1%) | 594 (24.9%) | 210 (38.4%) | 1356 (17.2%) |
Data are n (%).
IQR, interquartile range.
PS and BMI data were collected at the start of a regimen and were only available for patients documented as receiving SACT.
Of patients documented as having received SACT, 4971 (62.9%) received IT, 2388 (30.2%) NIT, and 547 (6.9%) received SACT IU. The median age was 59 years for IT and 76 years for NIT. Overall, 30.1% of those treated were overweight and 22.9% were obese. ECOG PS score was 0 to 1 in 56.3%. The PS of the IT group was better than that of the NIT group (mean ECOG PS score, 0.6 [SD, 0.8] vs 1.0 [SD, 0.8]; P < .001). The total Charlson score of IT was lower than that of NIT (0.2 [SD, 0.6] vs 0.5 [SD, 1.0]; P < .001). The IU group had significantly higher proportion of incomplete data on PS and BMI than the IT and NIT groups: PS score, 47.7% vs 35.8% (P < .001) and 27.8% (P < .001); BMI, 38.4% vs 11.1% (P < .001) and 24.9% (P < .001). The proportion of the documented SACT increased year-on-year, and there was a trend of improvement in data completeness in PS and BMI over time (supplemental Figure 1). There were no differences in transplant use between different ethnic groups (supplemental Figure 2).
OS after AML diagnosis
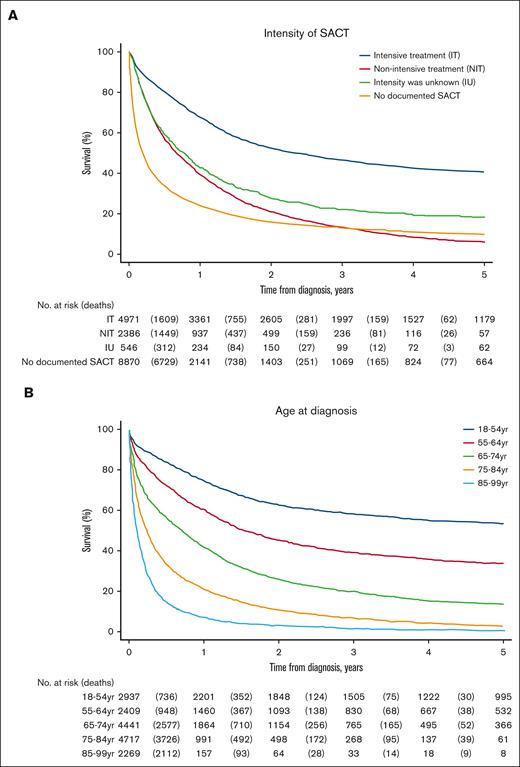
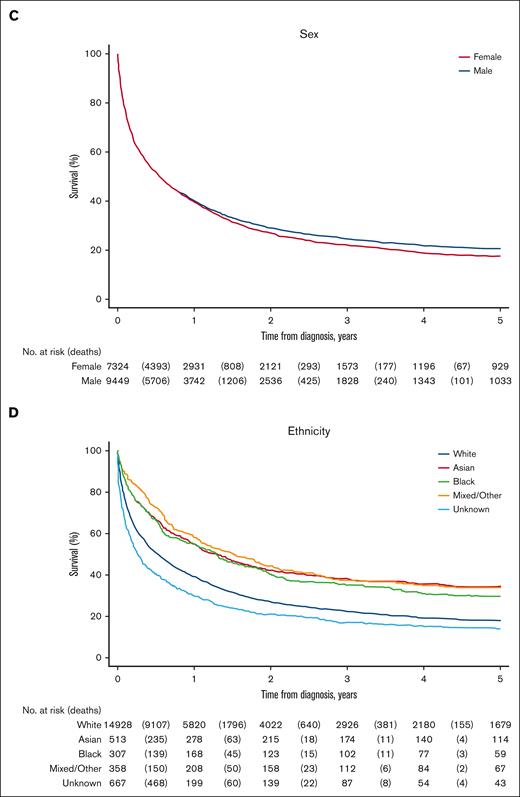
Survival analyses were based on 16 773 patients of the total cohort of 17 107 patients (Figure 2; Table 2; supplemental Tables 4 and 5). In total, 334 patients were excluded from survival analyses, of whom 331 had death certificate–only data, and 3 had an uncertain date of death.19
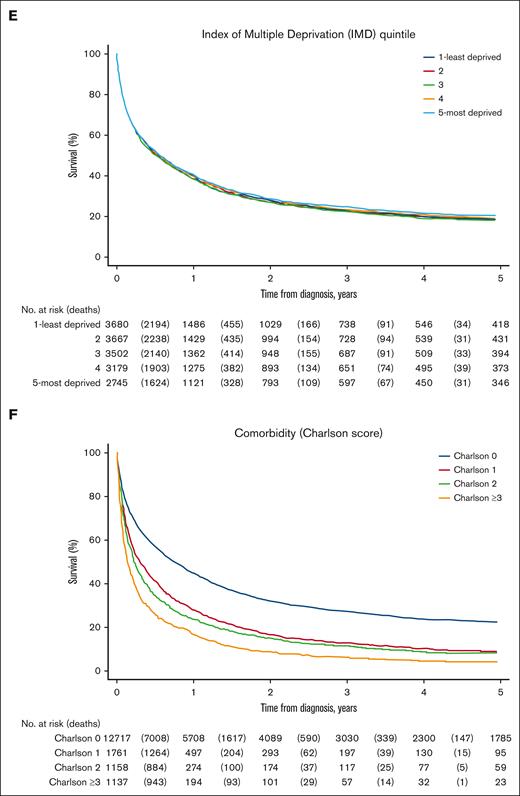
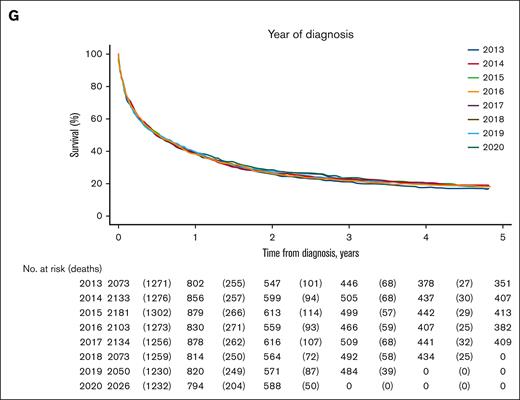
OS after AML diagnosis, by patient characteristic. (A) Intensity of SACT. (B) Age at diagnosis. (C) Sex. (D) Ethnicity. (E) Index of IMD quintile. (F) Comorbidity (Charlson score). (G) Year of diagnosis.
OS after AML diagnosis, by patient characteristic. (A) Intensity of SACT. (B) Age at diagnosis. (C) Sex. (D) Ethnicity. (E) Index of IMD quintile. (F) Comorbidity (Charlson score). (G) Year of diagnosis.
HR and 95% CI of patient characteristics associated with 1- and 5-year OS
| . | 1-y OS (n = 16 773∗) . | 5-y OS (n = 16 773∗) . | ||
|---|---|---|---|---|
| Unadjusted HR (95% CI) . | aHR† (95% CI) . | Unadjusted HR (95% CI) . | aHR† (95% CI) . | |
| Intensity of SACT | ||||
| IT | 1 [reference] | 1 [reference] | 1 [reference] | 1 [reference] |
| NIT | 2.23 (2.08-2.39) | 1.10 (1.01-1.18) | 2.27 (2.15-2.41) | 1.13 (1.06-1.20) |
| IU | 2.08 (1.84-2.34) | 1.31 (1.16-1.49) | 1.87 (1.69-2.07) | 1.26 (1.14-1.39) |
| No documented SACT | 4.07 (3.85-4.30) | 2.26 (2.12-2.40) | 3.19 (3.05-3.33) | 1.89 (1.80-1.99) |
| Age at diagnosis, y | ||||
| 18-54 | 1 [reference] | 1 [reference] | 1 [reference] | 1 [reference] |
| 55-64 | 1.74 (1.58-1.91) | 1.65 (1.50-1.82) | 1.75 (1.63-1.88) | 1.68 (1.56-1.81) |
| 65-74 | 3.04 (2.80-3.30) | 2.71 (2.49-2.95) | 3.11 (2.92-3.31) | 2.83 (2.66-3.02) |
| 75-84 | 5.49 (5.07-5.94) | 4.11 (3.77-4.48) | 5.39 (5.06-5.73) | 4.29 (4.01-4.60) |
| 85-99 | 9.48 (8.71-10.32) | 5.96 (5.44-6.53) | 9.17 (8.55-9.84) | 6.35 (5.89-6.85) |
| Sex | ||||
| Female | 1 [reference] | 1 [reference] | 1 [reference] | 1 [reference] |
| Male | 1.00 (0.96-1.04) | 0.98 (0.94-1.02) | 1.05 (1.01-1.09) | 1.02 (0.98-1.05) |
| Ethnicity | ||||
| White | 1 [reference] | 1 [reference] | 1 [reference] | 1 [reference] |
| Asian | 0.64 (0.56-0.72) | 0.86 (0.76-0.98) | 0.63 (0.56-0.70) | 0.86 (0.77-0.96) |
| Black | 0.63 (0.54-0.75) | 0.83 (0.70-0.98) | 0.68 (0.59-0.78) | 0.84 (0.73-0.96) |
| Mixed/other | 0.55 (0.47-0.65) | 0.93 (0.79-1.10) | 0.60 (0.53-0.69) | 0.98 (0.86-1.11) |
| Unknown | 1.35 (1.23-1.48) | 1.37 (1.25-1.51) | 1.27 (1.16-1.38) | 1.32 (1.21-1.44) |
| IMD quintile | ||||
| 1 (least deprived) | 1 [reference] | 1 [reference] | 1 [reference] | 1 [reference] |
| 2 | 1.04 (0.98-1.10) | 1.08 (1.02-1.14) | 1.03 (0.98-1.08) | 1.07 (1.01-1.12) |
| 3 | 1.04 (0.98-1.11) | 1.10 (1.03-1.16) | 1.04 (0.98-1.09) | 1.10 (1.04-1.16) |
| 4 | 1.01 (0.95-1.07) | 1.10 (1.04-1.17) | 1.00 (0.95-1.05) | 1.10 (1.04-1.16) |
| 5 (most deprived) | 0.99 (0.93-1.06) | 1.18 (1.11-1.26) | 0.98 (0.92-1.03) | 1.17 (1.11-1.24) |
| Comorbidity (total Charlson score) | ||||
| 0 | 1 [reference] | 1 [reference] | 1 [reference] | 1 [reference] |
| 1 | 1.57 (1.47-1.66) | 1.20 (1.13-1.28) | 1.57 (1.49-1.66) | 1.21 (1.15-1.28) |
| 2 | 1.79 (1.67-1.93) | 1.30 (1.21-1.39) | 1.73 (1.63-1.85) | 1.27 (1.19-1.35) |
| ≥3 | 2.29 (2.14-2.45) | 1.45 (1.35-1.55) | 2.25 (2.12-2.40) | 1.44 (1.35-1.54) |
| Year of diagnosis | ||||
| 2013 | 1.04 (0.97-1.13) | 0.91 (0.84-0.98) | 1.05 (0.98-1.12) | 0.95 (0.89-1.02) |
| 2014 | 1.01 (0.93-1.09) | 0.94 (0.87-1.01) | 1.00 (0.94-1.07) | 0.96 (0.90-1.03) |
| 2015 | 1.00 (0.92-1.08) | 0.96 (0.89-1.04) | 1.00 (0.93-1.07) | 0.98 (0.92-1.05) |
| 2016 | 1.04 (0.96-1.12) | 0.97 (0.90-1.05) | 1.04 (0.97-1.11) | 0.99 (0.93-1.06) |
| 2017 | 1 [reference] | 1 [reference] | 1 [reference] | 1 [reference] |
| 2018 | 1.04 (0.96-1.12) | 1.06 (0.98-1.14) | 1.02 (0.95-1.09) | 1.03 (0.97-1.11) |
| 2019 | 1.02 (0.94-1.10) | 1.04 (0.96-1.13) | 1.01 (0.95-1.08) | 1.04 (0.97-1.11) |
| 2020 | 1.04 (0.96-1.13) | 1.10 (1.02-1.20) | 1.00 (0.93-1.07) | 1.05 (0.98-1.13) |
| . | 1-y OS (n = 16 773∗) . | 5-y OS (n = 16 773∗) . | ||
|---|---|---|---|---|
| Unadjusted HR (95% CI) . | aHR† (95% CI) . | Unadjusted HR (95% CI) . | aHR† (95% CI) . | |
| Intensity of SACT | ||||
| IT | 1 [reference] | 1 [reference] | 1 [reference] | 1 [reference] |
| NIT | 2.23 (2.08-2.39) | 1.10 (1.01-1.18) | 2.27 (2.15-2.41) | 1.13 (1.06-1.20) |
| IU | 2.08 (1.84-2.34) | 1.31 (1.16-1.49) | 1.87 (1.69-2.07) | 1.26 (1.14-1.39) |
| No documented SACT | 4.07 (3.85-4.30) | 2.26 (2.12-2.40) | 3.19 (3.05-3.33) | 1.89 (1.80-1.99) |
| Age at diagnosis, y | ||||
| 18-54 | 1 [reference] | 1 [reference] | 1 [reference] | 1 [reference] |
| 55-64 | 1.74 (1.58-1.91) | 1.65 (1.50-1.82) | 1.75 (1.63-1.88) | 1.68 (1.56-1.81) |
| 65-74 | 3.04 (2.80-3.30) | 2.71 (2.49-2.95) | 3.11 (2.92-3.31) | 2.83 (2.66-3.02) |
| 75-84 | 5.49 (5.07-5.94) | 4.11 (3.77-4.48) | 5.39 (5.06-5.73) | 4.29 (4.01-4.60) |
| 85-99 | 9.48 (8.71-10.32) | 5.96 (5.44-6.53) | 9.17 (8.55-9.84) | 6.35 (5.89-6.85) |
| Sex | ||||
| Female | 1 [reference] | 1 [reference] | 1 [reference] | 1 [reference] |
| Male | 1.00 (0.96-1.04) | 0.98 (0.94-1.02) | 1.05 (1.01-1.09) | 1.02 (0.98-1.05) |
| Ethnicity | ||||
| White | 1 [reference] | 1 [reference] | 1 [reference] | 1 [reference] |
| Asian | 0.64 (0.56-0.72) | 0.86 (0.76-0.98) | 0.63 (0.56-0.70) | 0.86 (0.77-0.96) |
| Black | 0.63 (0.54-0.75) | 0.83 (0.70-0.98) | 0.68 (0.59-0.78) | 0.84 (0.73-0.96) |
| Mixed/other | 0.55 (0.47-0.65) | 0.93 (0.79-1.10) | 0.60 (0.53-0.69) | 0.98 (0.86-1.11) |
| Unknown | 1.35 (1.23-1.48) | 1.37 (1.25-1.51) | 1.27 (1.16-1.38) | 1.32 (1.21-1.44) |
| IMD quintile | ||||
| 1 (least deprived) | 1 [reference] | 1 [reference] | 1 [reference] | 1 [reference] |
| 2 | 1.04 (0.98-1.10) | 1.08 (1.02-1.14) | 1.03 (0.98-1.08) | 1.07 (1.01-1.12) |
| 3 | 1.04 (0.98-1.11) | 1.10 (1.03-1.16) | 1.04 (0.98-1.09) | 1.10 (1.04-1.16) |
| 4 | 1.01 (0.95-1.07) | 1.10 (1.04-1.17) | 1.00 (0.95-1.05) | 1.10 (1.04-1.16) |
| 5 (most deprived) | 0.99 (0.93-1.06) | 1.18 (1.11-1.26) | 0.98 (0.92-1.03) | 1.17 (1.11-1.24) |
| Comorbidity (total Charlson score) | ||||
| 0 | 1 [reference] | 1 [reference] | 1 [reference] | 1 [reference] |
| 1 | 1.57 (1.47-1.66) | 1.20 (1.13-1.28) | 1.57 (1.49-1.66) | 1.21 (1.15-1.28) |
| 2 | 1.79 (1.67-1.93) | 1.30 (1.21-1.39) | 1.73 (1.63-1.85) | 1.27 (1.19-1.35) |
| ≥3 | 2.29 (2.14-2.45) | 1.45 (1.35-1.55) | 2.25 (2.12-2.40) | 1.44 (1.35-1.54) |
| Year of diagnosis | ||||
| 2013 | 1.04 (0.97-1.13) | 0.91 (0.84-0.98) | 1.05 (0.98-1.12) | 0.95 (0.89-1.02) |
| 2014 | 1.01 (0.93-1.09) | 0.94 (0.87-1.01) | 1.00 (0.94-1.07) | 0.96 (0.90-1.03) |
| 2015 | 1.00 (0.92-1.08) | 0.96 (0.89-1.04) | 1.00 (0.93-1.07) | 0.98 (0.92-1.05) |
| 2016 | 1.04 (0.96-1.12) | 0.97 (0.90-1.05) | 1.04 (0.97-1.11) | 0.99 (0.93-1.06) |
| 2017 | 1 [reference] | 1 [reference] | 1 [reference] | 1 [reference] |
| 2018 | 1.04 (0.96-1.12) | 1.06 (0.98-1.14) | 1.02 (0.95-1.09) | 1.03 (0.97-1.11) |
| 2019 | 1.02 (0.94-1.10) | 1.04 (0.96-1.13) | 1.01 (0.95-1.08) | 1.04 (0.97-1.11) |
| 2020 | 1.04 (0.96-1.13) | 1.10 (1.02-1.20) | 1.00 (0.93-1.07) | 1.05 (0.98-1.13) |
Survival-related analyses were based on 16 773 patients of the total cohort of 17 107; 334 patients were excluded from survival analyses, of whom 331 had death certificate only data and 3 had an uncertain date of death.
Adjusted for intensity of SACT, age at diagnosis, sex, ethnicity, deprivation, comorbidity, and year of diagnosis.
Overall, the median survival time after AML diagnosis was 0.55 years (95% CI, 0.55-0.58), 1- and 5-year OS were 39.8% (95% CI, 39.1-40.5) and 18.8% (95% CI, 18.1-19.4) respectively. Of those receiving treatment, 1- and 5-year OS was 57.4% (95% CI, 56.3-58.4) and 29.0% (95% CI, 28.0-30.1), respectively. Survival was greater in those receiving IT than those receiving NIT (1-year OS: 67.6% vs 39.3%; aHR, 1.10; 95% CI, 1.01-1.18; 5-year OS: 40.6% vs 6.2%; aHR, 1.13; 95% CI, 1.06-1.20).
Survival outcome deteriorated with increasing age; the youngest age group (aged 18-54 years) had a 1- and 5-year OS of 74.9% (95% CI, 73.3-76.5) and 53.9% (95% CI, 52.0-55.7), respectively, which was better than for all older age groups. Asian and Black patients had better survival than White patients: Asian vs White (1-year OS: 54.2% vs 39.0%; aHR, 0.86; 95% CI, 0.76-0.98; 5-year OS: 34.6% vs 17.8%: aHR, 0.86; 95% CI, 0.77-0.96); Black vs White (1-year OS: 54.7% vs 39.0%; aHR, 0.83; 95% CI, 0.70-0.98; 5-year OS: 29.7% vs 17.8%; aHR, 0.84; 95% CI, 0.73-0.96). Survival for patients from the least deprived areas (IMD quintile 1) was better than for those from other areas (IMD quintiles 2-5): quintile 1 (1-year OS: 40.4%; 5-year OS: 18.8%) vs quintile 5 (1-year OS:, 40.8%: aHR, 1.18; 95% CI, 1.11-1.26; 5-year OS: 20.1%; aHR, 1.17; 95% CI, 1.11-1.24). Survival decreased with increasing Charlson score, from 1- and 5-year OS of 44.9% [95% CI, 44.0-45.8] and 22.3% [95% CI, 21.6-23.1], respectively, in the Charlson 0 group (no comorbidity), to 17.1% [95% CI, 14.9-19.3] and 4.3% [95% CI, 3.2-5.7], respectively, in the Charlson ≥3 group. People with no comorbidity had a better aHR of survival than those with comorbidity. Sex and year of diagnosis were not significantly associated with survival.
Early mortality, within 30 days of SACT
The 30-day mortality–related analyses were based on 7903 patients of the total 7906 documented as having received SACT (Table 3; supplemental Figure 3). Three patients (2 had death certificate–only vital status data, and 1 had an uncertain date of death) were excluded.
OR and 95% CI of patient characteristics associated with 30-day mortality after initial SACT
| . | Unadjusted OR (95% CI) (n = 7903∗) . | aOR† (95% CI) (n = 7903∗) . |
|---|---|---|
| Intensity of SACT | ||
| IT | 1 [reference] | 1 [reference] |
| NIT | 1.82 (1.56-2.13) | 0.74 (0.60-0.92) |
| IU | 1.94 (1.50-2.53) | 0.92 (0.68-1.25) |
| Age at diagnosis, y | ||
| 18-54 | 1 [reference] | 1 [reference] |
| 55-64 | 1.49 (1.12-1.98) | 1.41 (1.05-1.88) |
| 65-74 | 2.71 (2.14-3.44) | 2.47 (1.92-3.20) |
| 75-84 | 3.43 (2.67-4.39) | 2.91 (2.14-3.95) |
| 85-99 | 7.21 (5.10-10.19) | 4.99 (3.32-7.51) |
| Sex | ||
| Female | 1 [reference] | 1 [reference] |
| Male | 1.03 (0.89-1.20) | 0.98 (0.84-1.15) |
| Ethnicity | ||
| White | 1 [reference] | 1 [reference] |
| Asian | 0.71 (0.45-1.11) | 0.93 (0.58-1.50) |
| Black | 0.57 (0.30-1.08) | 0.72 (0.37-1.41) |
| Mixed/other | 0.60 (0.35-1.01) | 0.81 (0.47-1.41) |
| Unknown | 1.81 (1.29-2.54) | 2.00 (1.40-2.85) |
| IMD quintile | ||
| 1 (least deprived) | 1 [reference] | 1 [reference] |
| 2 | 1.20 (0.96-1.49) | 1.19 (0.94-1.50) |
| 3 | 1.11 (0.88-1.39) | 1.11 (0.87-1.41) |
| 4 | 0.95 (0.75-1.21) | 1.00 (0.77-1.28) |
| 5 (most deprived) | 1.15 (0.90-1.46) | 1.22 (0.94-1.57) |
| Comorbidity (total Charlson score) | ||
| 0 | 1 [reference] | 1 [reference] |
| 1 | 1.20 (0.92-1.55) | 0.99 (0.75-1.31) |
| 2 | 1.54 (1.13-2.09) | 1.21 (0.87-1.69) |
| ≥3 | 2.41 (1.80-3.23) | 1.58 (1.15-2.18) |
| Year of diagnosis | ||
| 2013 | 0.91 (0.66-1.26) | 0.78 (0.56-1.11) |
| 2014 | 0.78 (0.57-1.07) | 0.75 (0.54-1.05) |
| 2015 | 0.85 (0.63-1.14) | 0.91 (0.66-1.24) |
| 2016 | 0.96 (0.72-1.28) | 0.97 (0.71-1.31) |
| 2017 | 1 [reference] | 1 [reference] |
| 2018 | 1.01 (0.76-1.33) | 1.04 (0.78-1.39) |
| 2019 | 0.97 (0.74-1.29) | 1.01 (0.75-1.34) |
| 2020 | 1.09 (0.84-1.43) | 1.12 (0.84-1.49) |
| ECOG PS score | ||
| 0 | 1 [reference] | 1 [reference] |
| 1 | 1.64 (1.30-2.07) | 1.34 (1.05-1.71) |
| 2 | 4.61 (3.51-6.06) | 3.36 (2.52-4.47) |
| 3/4 | 12.46 (8.96-17.33) | 9.46 (6.69-13.36) |
| Unknown | 1.98 (1.60-2.46) | 1.53 (1.22-1.94) |
| BMI | ||
| Underweight (<18.5 kg/m2) | 1.04 (0.56-1.91) | 0.91 (0.48-1.73) |
| Normal weight (18.5 to <25.0 kg/m2) | 1 [reference] | 1 [reference] |
| Overweight (25.0 to <30.0 kg/m2) | 1.10 (0.89-1.37) | 1.06 (0.84-1.32) |
| Obese (≥30.0 kg/m2) | 1.21 (0.97-1.52) | 1.12 (0.89-1.42) |
| Unknown | 2.71 (2.20-3.35) | 2.17 (1.71-2.75) |
| . | Unadjusted OR (95% CI) (n = 7903∗) . | aOR† (95% CI) (n = 7903∗) . |
|---|---|---|
| Intensity of SACT | ||
| IT | 1 [reference] | 1 [reference] |
| NIT | 1.82 (1.56-2.13) | 0.74 (0.60-0.92) |
| IU | 1.94 (1.50-2.53) | 0.92 (0.68-1.25) |
| Age at diagnosis, y | ||
| 18-54 | 1 [reference] | 1 [reference] |
| 55-64 | 1.49 (1.12-1.98) | 1.41 (1.05-1.88) |
| 65-74 | 2.71 (2.14-3.44) | 2.47 (1.92-3.20) |
| 75-84 | 3.43 (2.67-4.39) | 2.91 (2.14-3.95) |
| 85-99 | 7.21 (5.10-10.19) | 4.99 (3.32-7.51) |
| Sex | ||
| Female | 1 [reference] | 1 [reference] |
| Male | 1.03 (0.89-1.20) | 0.98 (0.84-1.15) |
| Ethnicity | ||
| White | 1 [reference] | 1 [reference] |
| Asian | 0.71 (0.45-1.11) | 0.93 (0.58-1.50) |
| Black | 0.57 (0.30-1.08) | 0.72 (0.37-1.41) |
| Mixed/other | 0.60 (0.35-1.01) | 0.81 (0.47-1.41) |
| Unknown | 1.81 (1.29-2.54) | 2.00 (1.40-2.85) |
| IMD quintile | ||
| 1 (least deprived) | 1 [reference] | 1 [reference] |
| 2 | 1.20 (0.96-1.49) | 1.19 (0.94-1.50) |
| 3 | 1.11 (0.88-1.39) | 1.11 (0.87-1.41) |
| 4 | 0.95 (0.75-1.21) | 1.00 (0.77-1.28) |
| 5 (most deprived) | 1.15 (0.90-1.46) | 1.22 (0.94-1.57) |
| Comorbidity (total Charlson score) | ||
| 0 | 1 [reference] | 1 [reference] |
| 1 | 1.20 (0.92-1.55) | 0.99 (0.75-1.31) |
| 2 | 1.54 (1.13-2.09) | 1.21 (0.87-1.69) |
| ≥3 | 2.41 (1.80-3.23) | 1.58 (1.15-2.18) |
| Year of diagnosis | ||
| 2013 | 0.91 (0.66-1.26) | 0.78 (0.56-1.11) |
| 2014 | 0.78 (0.57-1.07) | 0.75 (0.54-1.05) |
| 2015 | 0.85 (0.63-1.14) | 0.91 (0.66-1.24) |
| 2016 | 0.96 (0.72-1.28) | 0.97 (0.71-1.31) |
| 2017 | 1 [reference] | 1 [reference] |
| 2018 | 1.01 (0.76-1.33) | 1.04 (0.78-1.39) |
| 2019 | 0.97 (0.74-1.29) | 1.01 (0.75-1.34) |
| 2020 | 1.09 (0.84-1.43) | 1.12 (0.84-1.49) |
| ECOG PS score | ||
| 0 | 1 [reference] | 1 [reference] |
| 1 | 1.64 (1.30-2.07) | 1.34 (1.05-1.71) |
| 2 | 4.61 (3.51-6.06) | 3.36 (2.52-4.47) |
| 3/4 | 12.46 (8.96-17.33) | 9.46 (6.69-13.36) |
| Unknown | 1.98 (1.60-2.46) | 1.53 (1.22-1.94) |
| BMI | ||
| Underweight (<18.5 kg/m2) | 1.04 (0.56-1.91) | 0.91 (0.48-1.73) |
| Normal weight (18.5 to <25.0 kg/m2) | 1 [reference] | 1 [reference] |
| Overweight (25.0 to <30.0 kg/m2) | 1.10 (0.89-1.37) | 1.06 (0.84-1.32) |
| Obese (≥30.0 kg/m2) | 1.21 (0.97-1.52) | 1.12 (0.89-1.42) |
| Unknown | 2.71 (2.20-3.35) | 2.17 (1.71-2.75) |
30-day mortality-related analyses were based on 7903 patients of the total 7906 documented as receiving SACT treatment. Three patients (2 had death certificate only vital status data and 1 uncertain date of death) were excluded.
Adjusted for intensity of SACT, age at diagnosis, sex, ethnicity, deprivation, comorbidity, year of diagnosis, PS, and BMI. The multivariate model had an area under receiver operating characteristic of 0.72 for predicting 30-day mortality.
The unadjusted 30-day mortality was 9.9% (95% CI, 9.3-10.6) overall, 7.8% (95% CI, 7.1-8.6) for the IT and 13.3% (95% CI, 12.0-14.8) for the NIT groups. After adjusting for covariates (the multivariate model had an area under receiver operating characteristic curve of 0.72 for predicting 30-day mortality),20 the risk of early mortality with different intensity of therapy was inverted: the patients who received NIT were less likely to die ≤30 days from receiving SACT than those receiving IT (aOR, 0.74; 95% CI, 0.60-0.92). All older patient groups were associated with an increased likelihood of dying ≤30 days from receiving SACT when compared with the youngest group (aged 18-54 years). Patients with a Charlson score of ≥3 had greater odds of dying ≤30 days from receiving SACT than patients with Charlson score of 0: aOR, 1.58 (95% CI, 1.15-2.18). Poorer PS was associated with higher 30-day mortality: ECOG PS score of 0 vs 1 (aOR, 1.34; 95% CI, 1.05-1.71); ECOG PS score of 0 vs 2 (aOR, 3.36; 95% CI, 2.52-4.47); and ECOG PS score of 0 vs 3/4 (aOR, 9.46; 95% CI, 6.69-13.36). Sex, known ethnicity, socioeconomic deprivation, year of diagnosis, and known BMI were not significantly associated with 30-day death after SACT.
Discussion
Our analysis on real-world outcomes of >17 000 patients in England diagnosed with AML has enabled us to explore the role of factors such as socioeconomic deprivation and ethnicity, which are harder to address in randomized control trials of AML because of selection bias and sample size. Overall, we found a 5-year survival of 18.8% (95% CI, 18.1-19.4), which was similar to the reported 17.5% (95% CI, 17.1-17.8) for all ages from 94 cancer registries in Europe (2000-2007)21 and 13.6% in a regional English registry, the Haematologicial Malignancy Research Network of 4 million patients from 2010 to 2019.22 However, our 5-year survival was much lower than the reported 31.7% (95% CI, 31.0-32.3) for AML of all ages based on the Surveillance, Epidemiology, and End Results (SEER) group data (2013-2019).23 This might be because of some limitations in the SEER data,24 for example, the population of patients recorded in the SEER database are more likely to be urban and medically insured. SEER data have previously been shown to have lower incidence rates of AML in older patients than a European registry,25 which could also contribute to the higher long-term survival seen. These comparisons must be interpreted with caution given that international registry data are often difficult to compare because of a lack of standardization of cohort definitions. Our AML cohort did not include any patient having undergone a transformation event from a different type of hematological malignancy (supplemental Table 1),11 which was not the same as in the European registries, the Haematologicial Malignancy Research Network, or SEER analysis.21-23
Our results suggest that patients from deprived backgrounds had worse survival outcomes. This is consistent with findings from other developed nations26-28 but, to our knowledge, the first time this has been demonstrated in England. It is unclear from this study whether deprivation in itself is a risk factor for developing leukemia. There is a known association between deprivation and shorter life expectancy in the general population.29 The over-representation of deprived patients in the younger leukemia demographic raises interesting questions about the relative roles of accelerated aging, comorbidities, or lifestyle factors in leukemogenesis. It would be important to explore whether adverse genetic subtypes, including those more commonly seen in older patients, such as secondary AML, are more prevalent in this patient group.
The median age at diagnosis in our cohort was younger for Black and Asian patients than for White patients. This is representative of demographic differences within England because ethnic minorities make up a smaller proportion of the population aged ≥65 years.30 However, survival of patients of Asian and Black ethnicity were far better than White patients and remained significant in multivariate analysis. This is in contrast to data from the United States. SEER data demonstrated that Black patients had a significantly shorter survival than White patients, particularly marked in those aged <60 years.4 Analysis of a much smaller cohort of Alliance/Cancer and Leukemia Group B trial data of adolescent and young Black adults (aged ≤39 years) similarly showed a decrease in OS (5-year OS: 22% vs 51%, P < .001) but with a higher early death rate (16% vs 3%, P = .02).5 No increase in early mortality was found in our study or in another study looking at all Cancer and Leukemia Group B trials.4
Evidence is emerging that the prevalence and prognostic information of molecular changes in AML may be influenced by ancestry. In Black patients, several studies now report lower incidences of NPM1 mutation, whereas mutations not previously implicated in leukemia have been identified.4,7 Furthermore, the impact of NPM1 and other favorable-risk mutations predict a less favorable outcome in US Black patients possibly mediated through less favorable leukemic stem cell gene expression profiles.7 Molecular and genetic results were lacking from our study to be able to explore the impact of these on outcomes in different ethnic groups.
A retrospective urban US study found that indicators of structural racism (assessed by census tract variables) were a stronger mediator of disparities in AML outcomes than molecular features, comorbidities, health care access, and treatment31; the study also demonstrated significantly lower transplant use in Black patients, which has also been reported in other US studies.32 We did not find a difference in the proportion of patients who received a transplant based on ethnicity in England.
Although our findings on the impact of ethnicity on outcomes are different than those from the United States, it is important to recognize that ethnicity exists at the intersection between biology and socioeconomics. Access to a universal, free health care system in England may help address some aspects of health inequality, for example, transplant use, but the over-representation of Black and Asian patients in deprived areas, and the associated reduced survival in socioeconomically deprived groups more generally shows that inequalities do persist. Therefore, further study is needed to understand better the determinants of outcomes for different ethnic groups.
The data from the NCRD and SACT Datasets confirmed that AML was a disease of older age and, as expected, patients documented as having received systemic treatment were younger and had fewer comorbidities. Patients receiving IT had a better chance of surviving for 1 and 5 years after AML diagnosis than patients receiving NIT. However, the overall benefit of IT comes at the risk of increased early treatment related mortality. There was no temporal trend in survival by year of diagnosis.
Our findings are strengthened by the completeness of case recording, given the requirements of mandatory reporting of all new cases of AML in NHS organizations in England, and thus provide a near-complete overview of the outcomes of a full cohort of all patients with AML aged 18 to 99 years.
There are limitations, including incomplete data in the NCRD and SACT Datasets. The proportion of those documented as having received treatment increased year-on-year and it is likely that some patients not recorded in the SACT Dataset will have received chemotherapy. However, the distribution of age, sex, ethnicity, deprivation, and comorbidity within the treated group did not differ for any year (supplemental Figure 1), suggesting that this incomplete reporting does not introduce a bias. In line with this, the proportion of patients receiving treatment in our cohort remains close to, but lower than, the figures reported worldwide.33 Addressing limitations within our data sets will be the focus of continued efforts for data completeness and quality control over the next few years. There is clear potential to extend the scope through improving data linkages to genetics laboratories, and other known determinants of outcomes including allogeneic transplant rates and additional demographic data (eg, marriage status).34 In addition, our analysis highlights a number of topics that need further research scrutiny. For example, our results did not suggest that obesity was associated with worse outcomes, and yet the full role of nutrition in modifying outcomes in hematological and other cancers, including immunomodulation, is unclear.35
Conclusions
Using a population data set of >17 000 patients, we identified better survival in Black and Asian groups than in White patients. Lower socioeconomic status was associated with lower survival. Older age, comorbidity, and poorer PS were negatively associated with outcomes. Our study highlights the importance of understanding the impact of ethnicity in more detail; including but not limited to disease biology, different responses to treatment, donor availability, transplantation rates, and the impact of cultural factors on treatment in different health care systems. Patients receiving intensive chemotherapy had lower early mortality, but after accounting for cofactors, the adjusted risk is higher than when compared with NIT. Selection of IT vs NIT should be based on individual patient factors, balancing improved long-term survival against higher early mortality. Our work highlights the importance of large population-based AML data sets alongside randomized trials.
Acknowledgments
The authors acknowledge the contributions of David Bowen, who was involved with the design of the study. Bowen led the assessment of the intensity of the initial SACT treatment. The authors acknowledge Craig Knott who quality assured the structured query language codes for data extraction from the SACT Dataset. This work uses data that have been provided by patients and collected by the National Health Service (NHS) England as part of their care and support. The data are collated, maintained, and quality assured by the National Disease Registration Service, which is part of NHS England. This article's independent research was conducted by staff at the National Disease Registration Service and in collaboration with clinicians at the NHS England.
S.J.S. reports funding from the National Institute for Health and Care Research (NIHR203334).
Authorship
Contribution: H.L., T.C., and S.J.S. designed the study; B.R. defined the AML cohort; H.L. extracted the data from the NCRD and the SACT Dataset; S.M. verified the structured query language codes for data extraction from the NCRD; H.L., T.C., and S.J.S. planned the analysis; H.L. conducted the analysis; S.M. verified the analysis program; H.L., T.C., S.J.S., M.B., and S.M. interpreted data; and all authors were involved in writing, reviewing, and editing drafts of the manuscript, and approving the manuscript for submission.
Conflict-of-interest disclosure: The authors declare no competing financial interests.
Correspondence: Thomas Coats, Royal Devon and Exeter Hospital, Wonford Site, Barrack Rd, Exeter EX2 5DW, United Kingdom; email: thomas.coats@nhs.net.
References
Author notes
Data were obtained from the National Cancer Registration Dataset and the Systemic Anti-Cancer Therapy Dataset, which belong to the National Disease Registration Service (NDRS), part of the National Health Service (NHS) England. All data included in this study are stored in the Cancer Analysis System database hosted by the NDRS. Any request for access to cancer registration data needs to go through NHS England data access request service via data.applications@nhsdigital.nhs.uk.
The full-text version of this article contains a data supplement.