Visual Abstract
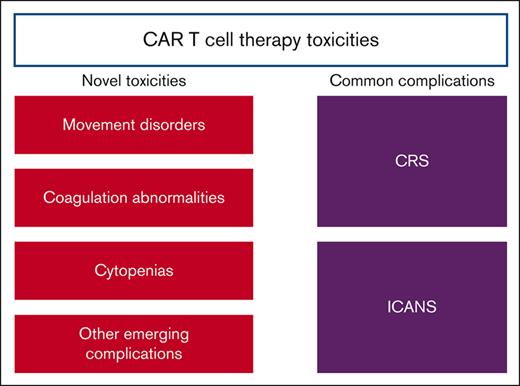
Multiple chimeric antigen receptor (CAR) T-cell therapies are US Food and Drug Administration–approved, and several are under development. Although effective for some cancers, toxicities remain a limitation. The most common toxicities, that is, cytokine release syndrome and immune effector cell–associated neurotoxicity syndrome, are well described. With increasing utilization, providers worldwide are reporting other emergent and often complicated toxicities. Given the evolving toxicity profiles and urgent need to catalog these emerging and emergent CAR T-cell toxicities and describe management approaches, the American Society of Hematology Subcommittee on Emerging Gene and Cell Therapies organized the first scientific workshop on CAR T-cell toxicities during the annual society meeting. The workshop functioned to (1) aggregate reports of CAR T-cell emergent toxicities, including movement disorders after B-cell maturation antigen CAR T cell, coagulation abnormalities, and prolonged cytopenia; (2) disseminate bedside-to-bench efforts elucidating pathophysiological mechanisms of CAR T-cell toxicities, including the intestinal microbiota and systemic immune dysregulation; and (3) highlight gaps in the availability of clinical tests, such as cytokine measurements, which could be used to expand our knowledge around the monitoring of toxicities. Key themes emerged. First, although clinical manifestations may develop before the pathophysiologic mechanisms are understood, they must be studied to aid in the detection and prevention of such toxicities. Second, systemic immune dysregulation appears to be central to these emergent toxicities, and research is needed to elucidate the links between tumors, CAR T cells, and microbiota. Finally, there was a consensus around the urgency to create a repository to capture emergent CAR T-cell toxicities and the real-world management.
Introduction
Chimeric antigen receptor (CAR) T-cell therapies are a novel treatment approach for hematologic malignancies. There are currently 6 CAR T-cell products that are approved by the US Food and Drug Administration for the treatment of pediatric and adult B-cell acute lymphoblastic leukemia, non-Hodgkin lymphoma, including diffuse large B-cell lymphoma, follicular lymphoma, mantle cell lymphoma, and multiple myeloma (MM). Despite the remarkable clinical response rates of patients treated with this technology, the associated toxicities remain a key limitation.
A number of guidelines, grading systems, and papers have been developed to help predict and provide clinical guidance on the management of the 2 most common side effects related to CAR T-cell therapy: cytokine release syndrome (CRS) and immune effector cell–associated neurotoxicity syndrome (ICANS).1-3 Nonetheless, there remains limited information on emerging and emergent CAR T-cell therapy–related toxicities beyond CRS and ICANS.
We collected information related to these novel toxicities and gathered experts with real-world experience with the use of CAR T-cell therapy and these emergent complications. The goal was to develop awareness and identify areas with the greatest need for research to better define the etiology of these complications and improve clinical guidance in the management of these nuanced CAR T-cell therapy–related toxicities. Here, we report the discussions that resulted from the first scientific workshop on CAR T-cell therapy toxicities organized by the American Society of Hematology Subcommittee on Emerging Cell and Gene Therapies that occurred in December 2022 during the annual American Society of Hematology meeting. The workshop functioned to (1) aggregate reports of CAR T-cell emergent toxicities, including movement disorders after B-cell maturation antigen (BCMA) CAR T-cell therapy, coagulation abnormalities, and prolonged cytopenia; (2) disseminate bedside-to-bench efforts to elucidate the pathophysiological mechanisms of CAR T-cell toxicities, including microbiota and systemic immune dysregulation; and (3) highlight gaps in the availability of clinical tests, such as cytokine measurements, which could be used to expand our knowledge base around the monitoring of toxicities.
On-target off-tumor effects, including neurotoxicity, associated with BCMA-directed CAR T cells
Neurologic events are a common complication of CAR T-cell therapy. By expert consensus, a readily recognizable constellation of neurologic clinical features called ICANS has been defined.1 ICANS consists of an acute, typically monophasic constellation of mental status changes, particularly language disturbances that may progress to more severe manifestations, such as seizures, coma, and cerebral edema.1 Reported risk factors include high tumor burden and a history of early onset and/or high-grade CRS.4 The type of CAR construct may also impact the severity of neurotoxicity.5-7 Pretreatment elevations in inflammatory markers, including interleukin-6 (IL-6), C-reactive protein (CRP), and fibrinogen, are associated with higher ICANS risk.8,9 After infusion, ICANS is associated with higher peak CRP, ferritin, and proinflammatory cytokines, such as interferon gamma (IFN-γ), IL-6, IL-1, IL-10, monocyte chemoattractant protein-1, markers of endothelial activation,9,10 and CAR T-cell expansion, compared with the levels before infusion.11-15 Currently available consensus guidelines and institution-specific interventions2,3,16-18 do not generally address the rarer neurologic complications observed after CAR T-cell therapy. As new CAR constructs enter clinical trials for different diseases, the neurotoxicity profile of CAR T-cell therapy continues to evolve.19-21
One such rare event is delayed neurotoxicity, which has been described in up to 5% of recipients of anti-BCMA CAR T-cell therapy for relapsed refractory MM in clinical trials. This rare toxicity is clinically distinct from ICANS, which occurs within the first few weeks after CAR T-cell infusion. In contrast, delayed neurotoxicity has a sporadic presentation, is not associated with CRS, usually occurs weeks to months after CAR T-cell therapy, is progressive, and is usually not responsive to treatment, including steroids, anticytokine directed agents, or cytotoxic therapy aimed at killing off the CAR T cells. Van Oekelen et al initially described a patient with this progressive and fatal course of delayed neurocognitive deterioration who presented with bradykinesia, tremor, and shuffling gait resembling parkinsonism after anti-BCMA CAR T-cell therapy.21 This neurologic complication was found to be associated with abnormally high levels of CAR T cells in the peripheral blood and cerebrospinal fluid (CSF) and on-target off-tumor effects dependent on the expression of BCMA protein in the neurons and microglia in the caudate nucleus of the patient.
On-target off-tumor effects after CAR T-cell therapy may trigger emergent and unexpected toxicities resulting from the inadvertent targeting of nonmalignant cells expressing the same or similar antigen, which represents a serious safety concern.22 Most target antigens that are currently used to redirect the specificity of CAR T cells in clinical development are tumor-associated antigens (TAA), normal proteins that are overexpressed on tumor cells and that do not derive from mutated areas of the genome, such as neoantigens with higher tumor-specificity. These molecules are expressed to some extent in normal tissues as well. CD19 expression is restricted to normal B cells, leading to transient B-cell aplasia upon CAR T-cell therapy. That is supportable with the administration of immunoglobulins. Conversely, on-target off-tumor toxicity represents a significant risk for other CAR T-cell therapies recognizing targets other than CD19 that are also expressed in vital normal organs of the body, posing significant risks in terms of toxicity (Table 1). For instance, unexpected cerebellar toxicity was described after the infusion of high-dose G protein–coupled receptor class C group 5 member D CAR T cells in patients with MM.27 In T-cell therapies targeting carcinoembryonic antigen, hemorrhagic colitis due to the expression of carcinoembryonic antigen in normal colon cells is a key limitation.28 In patients with renal carcinoma treated with engineered T cells recognizing carbonic anhydrase IX antigen, cholestasis develops due to the expression of this molecule in the gallbladder.23,29 Likewise, in patients with breast cancer treated with human epidermal growth factor receptor 2 CAR T cells, respiratory insufficiency due to the expression of human epidermal growth factor receptor 2 in normal lung cells has also been seen.30 These events highlight the need for the precise annotation of newly discovered target antigens in normal tissues. Some repositories relying on RNA expression levels, such as the the Genotype-Tissue Expression (GTEx) Portal, are publicly available, and others based on protein expression are under development.24,25
CAR target antigens with target-associated tumors and target-associated normal tissues, along with a description of toxicity and first reported patient cases
| CAR target . | Target-associated tumor . | Target-associated normal tissue . | Toxicity . | Onset . | First reported . |
|---|---|---|---|---|---|
| BCMA | MM | Basal ganglia (neurons and astrocytes) | Movement disorder (bradykinesia, postural instability, and tremor) | 3 mo | Van Oekelen et al 202121 |
| GPRC5D | MM | Cerebellum | Cerebellar toxicity (Dizziness, gait disturbance, and cerebellar atrophy) | 2-8 mo | Mailankody et al 202219 |
| Skin and keratinized tissue (nails and tongue) | Nail changes and loss, skin rash, and dysgeusia | 1-6 mo | |||
| CEA | Colorectal cancer | Colon crypt epithelial cells | Hemorrhagic colitis | 1 wk | Parkhurst et al 201123 |
| Carbonic anhydrase IX antigen | Renal cell carcinoma | Bile duct epithelial cells | Cholestasis and cholangitis | 2-7 d | Lamers et al 200624 |
| HER2 | Breast cancer | Lung epithelial cells | Respiratory insufficiency | During infusion | Morgan et al 201025 |
| EGFR | Biliary tract cancers | Epithelial cells | Mucositis, gastrointestinal hemorrhage, and desquamation | During infusion | Guo et al 201826 |
| Lung epithelial cells | Respiratory insufficiency | During infusion |
| CAR target . | Target-associated tumor . | Target-associated normal tissue . | Toxicity . | Onset . | First reported . |
|---|---|---|---|---|---|
| BCMA | MM | Basal ganglia (neurons and astrocytes) | Movement disorder (bradykinesia, postural instability, and tremor) | 3 mo | Van Oekelen et al 202121 |
| GPRC5D | MM | Cerebellum | Cerebellar toxicity (Dizziness, gait disturbance, and cerebellar atrophy) | 2-8 mo | Mailankody et al 202219 |
| Skin and keratinized tissue (nails and tongue) | Nail changes and loss, skin rash, and dysgeusia | 1-6 mo | |||
| CEA | Colorectal cancer | Colon crypt epithelial cells | Hemorrhagic colitis | 1 wk | Parkhurst et al 201123 |
| Carbonic anhydrase IX antigen | Renal cell carcinoma | Bile duct epithelial cells | Cholestasis and cholangitis | 2-7 d | Lamers et al 200624 |
| HER2 | Breast cancer | Lung epithelial cells | Respiratory insufficiency | During infusion | Morgan et al 201025 |
| EGFR | Biliary tract cancers | Epithelial cells | Mucositis, gastrointestinal hemorrhage, and desquamation | During infusion | Guo et al 201826 |
| Lung epithelial cells | Respiratory insufficiency | During infusion |
CEA, carcinoembryonic antigen; EGFR, epidermal growth factor receptor; GPRC5D, G protein–coupled receptor class C group 5 member D; HER2, human epidermal growth factor receptor 2.
Overall, these findings illustrate the need for a thorough work up of patients who develop complications upon novel CAR T-cell therapies.
Delayed neurotoxicity has been described with both anti-BCMA constructs, ciltacabtagene autoleucel (CARVYKTI) and idecabtagene vicleucel (ABECMA) and represents a key example of how bedside observations informed laboratory investigations. Although many patients are continuously described and awareness of this event increases, many questions remain open.
Whether certain patients are predisposed to complications remains unknown, and how patients can be screened to avoid significant complications is also unclear, particularly given their rare occurrence.
In retrospect, the aforementioned patient with delayed neurotoxicity and parkinsonism after BCMA CAR T-cell therapy was found to have punctate foci of T2-weighted-fluid-attenuated inversion recovery (T2-FLAIR) in the periventricular and subcortical white and given the physiological “scavenging” role of microglia in brain injury, perhaps imaging at screening, for example magnetic resonance imaging may be helpful in understanding whether pre-existing lesions predispose patients to delayed neurological complications. The patient also had aberrant persistence of CAR T cells beyond usual; perhaps, patients with circulating CAR T cells beyond 100 days are at higher risk and could be monitored more closely for neurological symptoms.31 Patients with neurological symptoms or signs, especially parkinsonism, may warrant referral to a movement disorder expert, if available.27 The work up should include imaging (magnetic resonance imaging) and CSF to rule out infection, leptomeningeal involvement, and CAR T-cell detection by flow, if possible. DaTSCAN (Ioflupane I 123 injection) is recommended as an adjunct to other diagnostic evaluations for striatal dopamine transporter visualization using single photon emission computed tomography brain imaging in adult patients with suspected Parkinsonian syndromes (unrelated to CAR T-cell therapy). A case report has demonstrated improvement in neurological symptoms with early use of chemotherapy;32 however, any immunosuppression should be used with caution, as secondary infection could lead to sepsis and worsen the overall outcome of the patient. Another emerging syndrome is localized tumor inflammation–associated neurotoxicity, termed TIAN.33 It is important to investigate the causative mechanisms of CAR-associated neurotoxicity, as careful and systematic monitoring of these side effects in clinical trials continues reporting of such cases.
Active research investigations toward the identification of suitable T-cell targets are also critical to develop effective and safe novel immune-based therapeutic interventions.22,24,25,34,35 Although the quest for better targets exclusively expressed on the tumor cells (tumor-specific target) remains open, combinatorial targeting platforms that use multispecific CAR T cells against 2 TAAs, neither of which is tumor specific, may help enhance specificity and decreasing toxicities.24,36-38
Cytokine profiling and CAR T-cell toxicities
The role of cytokines in CAR T-mitigated toxicities has been recognized since the advent of CAR T therapies.2,39-41 Real-time research–based measurement of cytokines in the first patients who received these therapies demonstrated that IL-6 levels were extremely high, and led to the targeted use of IL-6 blockade with tocilizumab for the treatment of CRS, which has become the mainstay of therapy for CRS (Table 2).1 However, clinical measurement of cytokines has only recently become available but is not uniformly accessible and is rapidly evolving. In many centers, clinical cytokines are only available as a “send out” test, with a turnaround time of several days which may limit real-time utilization of these results. With rapid improvements in technologies to automate and multiplex the measurement of cytokines, rapid and precise management of clinical cytokines in real time is becoming increasingly available.42 Serial measurement of cytokines is essential, as dynamic changes in cytokines are more important than the absolute levels, and there is high patient-level variability in individual cytokines. There is currently no standardization of cytokine measurements across clinical trials. A critical gap in our understanding of cytokine-driven toxicities is the standardization of measurement strategies, time points, and cytokine reporting across clinical trials.
Currently used interventions to mitigate CAR T-cell toxicities and relative mechanism of action and indications
| Targeted biological entities . | Therapeutic agents . | Mechanism of action . | Strategies . | Clinical trials . |
|---|---|---|---|---|
| Immune cell targeted | Corticosteroids (dexamethasone and methylprednisolone) | Glucocorticoid receptor agonist | Prophylactic: CRS/ICANS. Prophylactic dexamethasone 10 mg given on day 0, 1, and 2 after CAR infusion resulted in no grade 3 or higher CRS and a low rate of neurologic events in this study population.85 | NCT05459571, active not recruiting |
| Therapeutic: first line for treatment of CRS/ICANS. Grade 2-3 CRS/ICANS: dexamethasone 10 mg every 6-12 h (or methylprednisolone equivalent). Grade 4 CRS/ICANS: high-dose methylprednisolone 500 mg bid.3 | ||||
| IL-1 | Anakinra | IL-1 receptor antagonist | Prophylactic: CRS/ICANS. Under investigation, phase 2 results show a lower incidence of ICANS.95,96 There are active and recruiting trials ongoing. | NCT04359784, recruiting NCT04205838, recruiting NCT04148430, active not recruiting NCT04432506, active not recruiting |
| Therapeutic: steroid-refractory high-grade ICANS. Data are limited.86 | ||||
| IL-6 | Tocilizumab | IL-6 receptor antagonist | Prophylactic: CRS/ICANS. In ZUMA-1, tocilizumab used on day 2 may reduce the incidence of severe CRS but not the incidence of severe neurological events.97 | |
| Therapeutic: first line for CRS. Grade 2-4 CRS tocilizumab 8 mg/kg is administered >1 h (not to exceed 800 mg per dose). Repeat every 8 h if no improvement in CRS; limit to a maximum of 3 doses in 24 h and 4 doses total. Tocilizumab is FDA approved for use in CRS, but is not effective for isolated ICANS, and may be associated with worsening neurotoxicity.87 | ||||
| Siltuximab | IL-6 antagonist | Prophylactic: CRS/ICANS. Data from the phase 1 study showed no dose-limiting toxicities associated with single-dose siltuximab prophylaxis before CAR infusion.98 | ||
| Therapeutic: refractory CRS/ICANS, limited data during national tocilizumab shortage suggests use is safe and feasible.99 There is an active and recruiting trial ongoing for further investigation. | NTC04975555, recruiting | |||
| TNF-α | Etanercept | TNF-α blocking antibody | Therapeutic: data limited to case series; further studies are needed.100 | |
| IFN-γ | Emapalumab | IFN-γ– blocking antibody | Therapeutic: FDA approved for primary HLH. Limited data for CRS/ICANS/HLH to case series.88 | |
| TKI | Dasatinib | BCR-Abl, Src, c-Kit, among others, multikinase inhibitor | Prophylactic: CRS/ICANS. Data are limited to case report. There is an active and recruiting clinical trial investigating the combination of CD19/BCMA-targeted T cells combined with dasatinib. | NCT04603872, recruiting |
| Ibrutinib | BTK inhibitor: inhibits IL-2–induced TKIs | Prophylactic: CRS/ICANS. Data are limited to a pilot study. CLL patients treated with CAR therapy combined with ibrutinib were associated with lower CRS severity and lower serum concentrations of CRS-associated cytokines despite equivalent in vivo CAR T-cell expansion.89 | ||
| Ruxolitinib | JAK inhibitor: pathway signaling blockade of multiple cytokines | Therapeutic: grade 3-4 steroid-refractory CRS. Limited data from a case report and pilot study suggests ruxolitinib is active in severe CRS without impairing the antitumor effect.90,91 | ||
| Itacitinib | JAK inhibitor: pathway signaling blockade of multiple cytokines | Prophylactic: CRS/ICAN, limited data from a preclinical study and a phase 2 study suggest prophylactic itacitinib reduced the onset and severity of CRS and ICANS.92,101 (NCT04071366). There is an active and recruiting trial. | NCT05757219, recruiting | |
| T-cell targeted | Antithymocyte globulin | Direct T-cell targeting | Therapeutic: severe CRS/ICANS. Limited data from the ZUMA-2 trial of patient with severe grade 4 ICANS with cerebral edema which resolved after intervention including ATG.93 | |
| Cyclophosphamide | Alkylating agent, direct T-cell targeting | Therapeutic: severe refractory CRS/ICANS. Data are limited to case report of posterior reversible encephalopathy syndrome after CAR therapy.102 | ||
| CAR T-cell targeted | CAR constructs safety switches (iC9, HSV-TK, CD20, EGFRt, among others). | Suicide switches (iC9), truncated target receptors targeted by monoclonal antibodies | Therapeutic: limited clinical data for iC9 safety switch in haploidentical adoptive modified stem-cell transplant.103 Limited case report data for iC9 safety switch for the treatment of severe and steroid-refractory grade 4 ICANS.94 There are active and recruiting trials investigating CAR construct safety switches for the treatment of CRS/ICANS. | NCT03016377, recruiting NCT03696784, recruiting |
| Pan-cytokine targeted | Hemofiltration, plasmapheresis | Whole plasma | Therapeutic: severe refractory CRS/ICANS. Data are limited to case report.104 |
| Targeted biological entities . | Therapeutic agents . | Mechanism of action . | Strategies . | Clinical trials . |
|---|---|---|---|---|
| Immune cell targeted | Corticosteroids (dexamethasone and methylprednisolone) | Glucocorticoid receptor agonist | Prophylactic: CRS/ICANS. Prophylactic dexamethasone 10 mg given on day 0, 1, and 2 after CAR infusion resulted in no grade 3 or higher CRS and a low rate of neurologic events in this study population.85 | NCT05459571, active not recruiting |
| Therapeutic: first line for treatment of CRS/ICANS. Grade 2-3 CRS/ICANS: dexamethasone 10 mg every 6-12 h (or methylprednisolone equivalent). Grade 4 CRS/ICANS: high-dose methylprednisolone 500 mg bid.3 | ||||
| IL-1 | Anakinra | IL-1 receptor antagonist | Prophylactic: CRS/ICANS. Under investigation, phase 2 results show a lower incidence of ICANS.95,96 There are active and recruiting trials ongoing. | NCT04359784, recruiting NCT04205838, recruiting NCT04148430, active not recruiting NCT04432506, active not recruiting |
| Therapeutic: steroid-refractory high-grade ICANS. Data are limited.86 | ||||
| IL-6 | Tocilizumab | IL-6 receptor antagonist | Prophylactic: CRS/ICANS. In ZUMA-1, tocilizumab used on day 2 may reduce the incidence of severe CRS but not the incidence of severe neurological events.97 | |
| Therapeutic: first line for CRS. Grade 2-4 CRS tocilizumab 8 mg/kg is administered >1 h (not to exceed 800 mg per dose). Repeat every 8 h if no improvement in CRS; limit to a maximum of 3 doses in 24 h and 4 doses total. Tocilizumab is FDA approved for use in CRS, but is not effective for isolated ICANS, and may be associated with worsening neurotoxicity.87 | ||||
| Siltuximab | IL-6 antagonist | Prophylactic: CRS/ICANS. Data from the phase 1 study showed no dose-limiting toxicities associated with single-dose siltuximab prophylaxis before CAR infusion.98 | ||
| Therapeutic: refractory CRS/ICANS, limited data during national tocilizumab shortage suggests use is safe and feasible.99 There is an active and recruiting trial ongoing for further investigation. | NTC04975555, recruiting | |||
| TNF-α | Etanercept | TNF-α blocking antibody | Therapeutic: data limited to case series; further studies are needed.100 | |
| IFN-γ | Emapalumab | IFN-γ– blocking antibody | Therapeutic: FDA approved for primary HLH. Limited data for CRS/ICANS/HLH to case series.88 | |
| TKI | Dasatinib | BCR-Abl, Src, c-Kit, among others, multikinase inhibitor | Prophylactic: CRS/ICANS. Data are limited to case report. There is an active and recruiting clinical trial investigating the combination of CD19/BCMA-targeted T cells combined with dasatinib. | NCT04603872, recruiting |
| Ibrutinib | BTK inhibitor: inhibits IL-2–induced TKIs | Prophylactic: CRS/ICANS. Data are limited to a pilot study. CLL patients treated with CAR therapy combined with ibrutinib were associated with lower CRS severity and lower serum concentrations of CRS-associated cytokines despite equivalent in vivo CAR T-cell expansion.89 | ||
| Ruxolitinib | JAK inhibitor: pathway signaling blockade of multiple cytokines | Therapeutic: grade 3-4 steroid-refractory CRS. Limited data from a case report and pilot study suggests ruxolitinib is active in severe CRS without impairing the antitumor effect.90,91 | ||
| Itacitinib | JAK inhibitor: pathway signaling blockade of multiple cytokines | Prophylactic: CRS/ICAN, limited data from a preclinical study and a phase 2 study suggest prophylactic itacitinib reduced the onset and severity of CRS and ICANS.92,101 (NCT04071366). There is an active and recruiting trial. | NCT05757219, recruiting | |
| T-cell targeted | Antithymocyte globulin | Direct T-cell targeting | Therapeutic: severe CRS/ICANS. Limited data from the ZUMA-2 trial of patient with severe grade 4 ICANS with cerebral edema which resolved after intervention including ATG.93 | |
| Cyclophosphamide | Alkylating agent, direct T-cell targeting | Therapeutic: severe refractory CRS/ICANS. Data are limited to case report of posterior reversible encephalopathy syndrome after CAR therapy.102 | ||
| CAR T-cell targeted | CAR constructs safety switches (iC9, HSV-TK, CD20, EGFRt, among others). | Suicide switches (iC9), truncated target receptors targeted by monoclonal antibodies | Therapeutic: limited clinical data for iC9 safety switch in haploidentical adoptive modified stem-cell transplant.103 Limited case report data for iC9 safety switch for the treatment of severe and steroid-refractory grade 4 ICANS.94 There are active and recruiting trials investigating CAR construct safety switches for the treatment of CRS/ICANS. | NCT03016377, recruiting NCT03696784, recruiting |
| Pan-cytokine targeted | Hemofiltration, plasmapheresis | Whole plasma | Therapeutic: severe refractory CRS/ICANS. Data are limited to case report.104 |
ATG, antithymocyte globulin; BCR-Abl, Ph chromosome; bid, twice daily; BTK, Bruton tyrosine kinase; c-Kit, proto-oncogene receptor tyrosine kinase; CLL, chronic lymphocytic leukemia; EGFRt, epidermal growth factor receptor; FDA, US Food and Drug Administration; HLH, hemophagocytic lymphohistiocystosis; HSV-TK, herpes simplex virus thymidine kinase; iC9, inducible caspase 9; Src, proto-oncogene tyrosine-protein kinase; TKI, tyrosine kinase inhibitor; TNF-α, tumor necrosis factor-α; ZUMA-1, phase 1/2, single-arm, multicenter study of axicabtagene ciloleucel in patients with refractory large B-cell lymphoma.
Increased availability of clinical cytokines is crucial for the development of targeted therapies for refractory CRS and for identifying new therapies for ICANS. Despite excellent responses to IL-6 blockade or steroids in most patients, some patients still develop refractory, life-threatening CRS. Further understanding of cytokine biology and its relationship with CAR T-cell therapy efficacy has recently led to potential breakthroughs in refractory CRS management. Larson et al demonstrated that IFN-γ was necessary for CAR T-cell target killing in solid tumors, but not in leukemia.43 Targeted IFN-γ blockade with emapalumab is clinically available and approved for both pediatric and adult primary hemophagocytic lymphohistiocytosis.44 Emapalumab has been used previously in the treatment of severe refractory CRS, with effective blockade of IFN-γ and clinical improvement in some cases.45 The clinical availability of cytokine panels could enable the use of this medication, and to monitor the response to therapy, both by measuring IFN-γ directly, and by measuring IFN-γ responsive proteins, such as CXCL9. This strategy in combination with CAR T cells for lymphoma is further justified by evidence that IFN-γ secretion upon CD19 stimulation in vitro is inversely associated with a durable response46 and findings that chronic lymphoma tumor IFN-γ signaling before CAR T-cell treatment is associated with lower rates of durable remission, upregulation of checkpoint ligands, and suppressive myeloid cells.47 However, the impact of emapalumab on the long-term efficacy of CAR T cells and infection risk in this patient population has not been systematically examined. The safety and efficacy of emapalumab in the treatment or prevention of refractory CRS should be examined in prospective clinical trials.
Targeted therapies for ICANS remain a key area of unmet need in the field. Preclinical work has implicated the monocyte-produced protein, IL-1β , in the pathophysiology of ICANS. This has led to a clinical investigation of IL-1 receptor blockade with anakinra, with recent work demonstrating that anakinra may prevent the development of ICANS in adult lymphoma patients.48,49 High-throughput proteomic analyses of cytokines have identified IL-18, an IL-1 related protein, to be associated with the onset of ICANS symptoms in pediatric patients treated with CAR T cells against CD19 for B-cell acute lymphoblastic leukemia (B-ALL).50 IL-18 has also been implicated in the development of immune effector cell-associated hemophagocytic lymphohistiocytosis-like syndrome (IEC-HS) after CAR T-cell targeting CD22 in pediatric B-ALL.51
A review of 21 clinical trials across 60 articles that featured a US Food and Drug Administration–approved CAR T-cell construct or 1 of its predecessors highlighted substantial variability and limited reporting of the cytokine measurement platforms and panels used. Specifically, 28 (46.7%) did not report any cytokine data, representing 6 of 21 clinical trials (28.6%). Furthermore, the correlation of cytokines with ICANS, CRS, and CRS severity was limited. Considering the fundamental role of cytokines in CAR T-cell toxicity, this analysis further supports the need to establish standardization of cytokine measurements.52 The increased availability of accurate, high-throughput, and multiplexed measurements of cytokines has significantly expanded our ability to measure and understand cytokines after CAR T-cell therapy. Future research efforts should focus on prospective validation of clinical cytokine measurements to predict toxicities and evaluate targeted therapies such as emapalumab for refractory CRS and IL-1 and IL-18 blockade for the treatment of ICANS.
Coagulopathies of CAR T-cell therapy
A growing concern exists that disruption of the hemostatic system in patients treated with CAR T-cell therapy may have clinical significance. The fundamental link between inflammation and coagulation has been well described, including the development of the term immunothrombosis.53 This term describes how the interaction between these 2 systems is a vital property of the body’s defense against pathogens. Immunothrombosis refers to a bidirectional interaction process between the innate immune pathway and the coagulation system. The immune system can activate a hemostatic response to generate thrombin and fibrin to limit the spread of a pathogen. However, although this system is tightly regulated, the supraphysiologic immune activation by CAR T cells can disrupt this fine balance and lead to bleeding or clotting problems. As was further highlighted early in the COVID-19 pandemic, thrombosis from marked inflammation can lead to marked morbidity and mortality. It is now well established that CAR T-cell therapy can lead to marked systemic inflammation. Not surprisingly, if the inflammatory system becomes activated, the coagulation system will be stimulated as well, potentially leading to significant challenges.
Evidence now confirms that this marked inflammation leads to perturbations in the hemostatic system. Two studies that evaluated coagulation laboratory tests after CAR T-cell therapy demonstrated that approximately half of the patients had at least 1 abnormality in a clotting test, and 7 of 100 patients even had laboratory evidence of disseminated intravascular coagulation (DIC).54,55 These unusual laboratory findings typically occurred 6 to 20 days after infusion and were more likely to be seen in patients with more severe CRS. Another paper specifically looked at the fibrinolytic system and noted that the average plasma levels of plasminogen activator inhibitor 1 nearly doubled within 2 weeks of CAR T-cell infusion, suggesting the development of a hypercoagulable state.56 However, in these studies, although the coagulation laboratory studies were unusual, the authors did not note any clinical correlation. Several more recent studies are now reporting an increase in clinically meaningful complications. One group noted that among 148 consecutive patients receiving CD19 CAR T-cell infusion, 11% developed new thromboses.57 Alternatively, in a separate analysis of 127 patients treated with CAR T-cell therapy, 9.4% of patients developed bleeding issues, whereas 6.3% developed thrombotic complications.58 Most recently, a retrospective review between the 2 institutions reported 10 thrombotic events in 140 consecutive patients (7.14%).59
The coexistence of DIC and severe CRS is closely related to nonrelapsed deaths during the acute toxicity phase, and effective and timely treatment is key to reduce mortality in patients with DIC and severe CRS.60
Although these retrospective studies imply an increased risk of thrombosis, more data are clearly required to determine whether this issue is with all CAR T-cell products or if certain ones carry a higher risk. If this indeed represents a significant risk to patients, algorithms can be developed to help predict those at the highest risk so that strategies to prevent problems can be developed. Finally, and potentially most importantly, although this may be a rare complication, it is imperative that safe and effective strategies exist for the management of these complicated patients. Anticoagulation therapy can be challenging in patients with low platelets, whereas correcting bleeding complications in patients who may be prothrombotic can be difficult as well. Therefore, more studies are required to help ensure optimal care for patients.
Bone marrow dysfunction and cytopenia
Increasingly, attention has been paid to cytopenia occurring after CAR T-cell therapy. Early (days 0-30) and late (day >30) cytopenia after CAR T-cell therapy exhibits the highest cumulative incidence of severe adverse events.61 Pivotal trials and real-world data across various disease subtypes, target antigens, and CAR constructs consistently report high rates of CAR T-cell–related cytopenia, albeit with varying degrees and durations.62-66
After CAR T hematotoxicity, in general, prolongs hospital stays and increases the risk of infectious complications, contributing to nonrelapse mortality.67 The initial phase of cytopenia can be attributed to lymphodepleting chemotherapy, but low blood counts can persist for extended periods, ranging from weeks to years after CAR T infusion. The pathomechanism of late cytopenia is not fully understood, but systemic immune dysregulation and secondary inflammatory insults induced by transfused CAR T-cell infusion are believed to play a significant role.66,68,69
Neutrophil recovery after CAR T-cell therapy shows 3 distinct patterns: quick recovery (median duration of neutropenia [absolute neutrophil count [ANC] 500/μL is 5 days), intermittent recovery (with a second dip in ANC <1.0 G/L after day 21), and aplastic phenotype (continuous severe neutropenia, ANC <0.5 G/L, for >14 days).66 The intermittent recovery type is observed in >50% of patients, with an initial ANC rise often due to granulocyte colony-stimulating factor (G-CSF) administration. Retrospective studies suggest that early G-CSF application does not increase the incidence of higher-grade CRS/ICANS nor does it negatively impact CAR T-cell expansion.70,71
Infectious complications occur at a similar frequency and severity in patients with quick and intermittent recovery phenotypes with close management and therapeutic intervention.72 Unresponsiveness to G-CSF is associated with the aplastic phenotype and should prompt further diagnostics.72 The initial step in the work up involves defining the differential diagnosis, encompassing drug-induced cytopenia, vitamin deficiencies, infectious causes, sustained inflammatory stressors, relapse, and bone marrow disease.
Therapeutically, G-CSF should be continued in patients with prolonged neutropenia and thrombopoietin (TPO) agonists should be considered for prolonged thrombocytopenia. However, data supporting TPO agonist use in the CAR T-cell setting are limited and based on small retrospective reports.73 In patients with an autologous or allogeneic hematopoietic stem-cell backup, a conditioning-free boost has been deemed safe and feasible.74-76
Patients with an aplastic phenotype and prolonged neutropenia face a high risk of severe infection within the first 90 days. To identify patients at high risk for prolonged neutropenia, the CAR-HEMATOTOX score was developed.66 This score incorporates factors related to hematopoietic reserve (ANC, hemoglobin, and platelet count) and baseline inflammation (CRP and ferritin) and has been validated for severe neutropenia (ANC <500/μL) lasting >14 days during the first 60 days after CAR T-cell infusion.
Importantly, the parameters for the CAR-HEMATOTOX score are determined in adult patients treated with axicabtagene ciloleucel or tisagenlecleucel for relapsed/refractory large B-cell lymphoma before the start of lymphodepleting chemotherapy, enabling early risk stratification into high- vs low-risk for severe hematotoxicity. The CAR-HEMATOTOX score has also been shown to be applicable in MM and mantle cell lymphoma.77 Further clinical trials are imperative to assess whether a CAR-HEMATOTOX score–based risk stratification for early G-CSF application and/or antibiotic prophylaxis will reduce the duration of neutropenia, lower the incidence of neutropenic fever, and decrease relapse-free mortality. This should take into account the fact that many patients treated with CAR T cells receive this treatment after exposure to many prior lines of therapy, which results in low marrow reserve and moving CAR T cells use to patients who are earlier in their course of therapy, which will impact the proportion of patients who experience aplastic marrow.
CAR T cells and the intestinal microbiome
To interrogate host endogenous factors that mediate CAR T-cell activity, the intestinal microbiome has been probed. Smith et al reported that the intestinal microbiome influences both toxicity and efficacy after CAR T-cell therapy.78 In a large multicenter cohort, CD19 CAR T-cell recipients (n = 228) treated at the Memorial Sloan Kettering Cancer Center and the University of Pennsylvania were retrospectively analyzed. The authors assessed broad-spectrum antibiotics that target obligate anaerobes and are used for the treatment of neutropenic fever, specifically piperacillin/tazobactam, meropenem, or imipenem/cilastatin (P-I-M), 4 weeks before CAR T-cell therapy. Exposure to P-I-M was associated with worse progression-free and overall survival as well as increased ICANS. There was no increase in CRS in the P-I-M–exposed patients.
Additionally, the authors analyzed the fecal microbiome in a prospective cohort of CD19 CAR T-cell recipients from both centers (n = 48) using 16S and metagenomic shotgun sequencing. The fecal microbiome cohort included patients for whom a baseline fecal sample was collected before CAR T-cell infusion. These data indicate that patients treated with CD19 CAR T cells had an altered fecal microbiome before cell infusion, as measured by lower alpha diversity, increased frequency of bacterial dominance, and bacterial composition that was distinct from that of healthy volunteers.78 The authors also evaluated the relationship between the abundance of specific bacterial taxa and clinic outcomes, including efficacy and toxicity. Notably, using 16S sequencing, the untargeted analysis found that the abundance of genera, including Blautia, Ruminococcus, Bacteroides, and Faecalibacterium, was associated with no toxicity.78 Furthermore, metagenomic shotgun sequencing has identified several pathways associated with toxicity. Notably, the nonoxidative branch of the pentose phosphate pathway (nonoxipent PWY) was the most enriched pathway in patients who experienced CAR T-cell toxicity. Notably, this pathway produces pyridoxal 5'-phosphate, which among other key roles serves as a cofactor for enzymes involved in tryptophan metabolism in bacteria as well as the host.79
Subsequent studies of the intestinal microbiome and CD19 CAR T-cell therapy have substantiated the impact of broad-spectrum antibiotics on worse survival and increased ICANS80 and identified the abundance of some overlapping bacterial taxa with CAR T-cell efficacy.78,80,81 Nonetheless, additional research, particularly in preclinical models, is needed to further understand the mechanism by which the intestinal microbiome mediates its impact on CAR T-cell function.
Conclusions
The workshop functioned to (1) aggregate reports of CAR T cell emergent toxicities, including movement disorders after BCMA CAR T cells, on-target off-tumor toxicities, coagulation abnormalities, prolonged cytopenia, and microbiome-related effects; (2) disseminate bedside-to-bench research results pointing to pathophysiological mechanisms of CAR T-cell toxicities; and (3) highlight gaps in the availability of clinical tests, such as cytokine measurements, which could be used to expand our knowledge base around the monitoring of toxicities, in the lack of standards for preclinical screening for off-tumor toxicity when developing new therapies targeting novel TAAs that could predict toxicity before bringing new agents to the clinic.
Despite the longstanding recognition of CRS and ICANS as common toxicities after CAR T-cell therapy, we still have limitations in our understanding of their pathophysiology and few or no clinical tests available to predict or track their occurrence or resolution. Increasing recognition of cytopenia and more infrequent but significant emergent toxicities has opened up new avenues of research. Early reports of these emergent toxicities are opening up new areas of research aimed at understanding, prevention, and treatment, with the overall goal of improving the outcome of patients undergoing CAR T-cell therapy.
These complications add to the risk of hemophagocytic lymphohistiocytosis82 or IEC-HS83 and the risk of T-cell malignancies.84
Several themes arose across the presentations and discussions at the workshop. First, there was a consensus for a need to investigate the pathophysiologic mechanisms that occur before we see the clinical manifestations. Overall, there was a concern that current treatment strategies for CAR T toxicities may be too late; understanding the timing of insults leading to clinical CAR T-cell therapy toxicities will allow for better early detection and prevention tools.
Second, the concept of systemic and tumor immune dysregulation as an overarching paradigm in the pathophysiology of CAR T-cell toxicity was discussed at length. It was felt that additional research linking CAR T-cell phenotype and function, tumor genomics and gene expression, metabolomics, microbiome, and serum cytokines may help to uncover mechanistic insights into common and emergent CAR T-cell toxicities.
Finally, there was significant interest and urgency to create a new data repository to capture emergent CAR T-cell toxicities beyond CRS and ICANS, as well as their real-world management. This is especially critical given the rapid proliferation of new products coming to the market and the increasing recognition of emergent toxicities. Such a repository should be complementary to current activities within the CAR toxicity space (eg, the registry of the Center for International Blood and Marrow Transplant Research, particularly by cataloging the incidence of under-recognized CAR T-cell toxicities and allowing the community to draw on the registry to inform real-time clinical decision-making.
Acknowledgments
This work is supported by the American Society of Hematology Subcommittee on Emerging Cell and Gene Therapy.
The content of this publication does not necessarily reflect the views or policies of the Department of Health and Human Services, nor does mention of trade names, commercial products, or organizations imply endorsement by the US Government.
Authorship
Contribution: F.P. and N.N.S. developed the idea and supervised the work; and all authors wrote the manuscript.
Conflict-of-interest disclosure: The authors declare no competing financial interests.
Correspondence: Fabiana Perna, Department of Blood and Marrow Transplant and Cellular Immunotherapy, Moffitt Cancer Center, 12902 USF Magnolia Drive, Tampa, FL 33612; email: fabiana.perna@moffitt.org; and Nirali N. Shah, Pediatric Oncology Branch, Center for Cancer Research, National Cancer Institute, National Institutes of Health, Building 10, Room 1W-3750 9000 Rockville Pike MSC 1104, Bethesda, MD 20892; email: nirali.shah@nih.gov.
References
Author notes
F.L.L. and N.N.S. contributed equally to this study.