Key Points
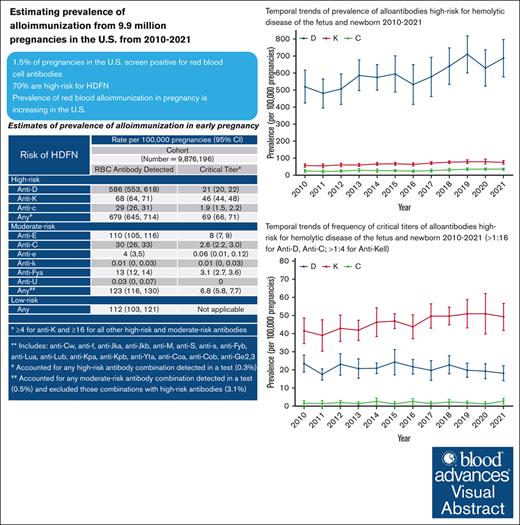
In this first national sample of RBC abs in pregnancies in the United States, 1.5% screened positive for RBC abs.
The prevalence of RBC abs increased from 2010 to 2021; RBC abs high risk for HDFN were identified in 74.3% of pregnancies.
Visual Abstract
Hemolytic disease of fetus and newborn (HDFN) is a life-threatening disease mediated by maternal alloimmunization to red blood cell (RBC) antigens. Studies of maternal alloimmunization prevalence in the United States lack national data. This study describes prevalence and trends in alloimmunization in pregnancy in the United States. RBC antibodies (abs) were identified in a large, nationwide, commercial laboratory database from 2010 through 2021. The cohort comprised pregnancies for which the year of laboratory collection and patient’s state of residence were available. Data were normalized based on US Centers for Disease Control and Prevention estimates of live births and weighted by year and US Census Division. Cochrane-Armitage tests assessed temporal trends of alloimmunization. Of 9 876 196 pregnancies, 147 262 (1.5%) screened positive for RBC abs, corresponding to an estimated prevalence of 1518 of 100 000 pregnancies. Of identified RBC abs, anti-D comprised 64.1% pregnancies (586/100 000). Prevalence of other high-risk RBC abs for HDFN included anti-K (68/100 000) and anti-c (29/100 000). Incidence of all 3 high-risk abs increased from 2010 to 2021 (all P < .001). Among almost 10 million pregnancies in the United States, comprising an estimated 14.4% of all pregnancies, 1.5% screened positive for RBC abs. Almost three-quarters (679/100 000 [74.3%]) of RBC abs identified were high risk for HDFN. Although prevalence of anti-D is difficult to interpret without the ability to distinguish alloimmunization from passive immunity, it remains problematic in HDFN, ranking second only to anti-K in critical titers. Given the sequelae of HDFN, new initiatives are required to reduce the incidence of alloimmunization in patients of reproductive potential.
Introduction
Maternal red blood cell (RBC) alloimmunization typically occurs in response to either blood transfusion or exposure to fetal RBC antigens during pregnancy.1 Hemolytic disease of the fetus and newborn (HDFN) remains a significant public health concern with an estimated incidence of 1.6 cases per 1000 live births.2 Rhesus (Rh) alloimmunization has been known to be a primary risk factor for HDFN since the 1940s.3 Subsequently, maternal antibodies (abs) to >50 non-ABO blood group antigens have been implicated with variable incidence and severity of HDFN.4 Most clinically significant cases result from exposure to antigens in the Rh, Kell, Duffy, Kidd, and MNS families.5,6 Over the past 60 years, routine administration of antenatal and postnatal anti-D immune-prophylaxis has dramatically reduced anti-D–associated HDFN in the United States.7,8 Other maternal abs are now emerging as significant contributors to HDFN, and there is no equivalent prophylactic strategy available for non-Rh(D) antigens.9 National prevalence of RBC abs has been estimated in several countries, ranging from 0.3% to 3.4% of pregnant individuals.10-18 In the United States, however, prevalence estimates of RBC abs in pregnancy have been confined to single-center reports, with limited applicability to a national population.19,20
In this study, we report prevalence and temporal trends in red cell alloimmunization in pregnancy in a large, national cohort in the United States.
Methods
Prenatal RBC abs screening test results during the years 2010 to 2021 were extracted from the database of a large commercial laboratory (Quest Diagnostics) that serves half of all prescribing physicians and hospitals in the United States. Data were collected from maternal blood specimens sent for an initial obstetric panel; this panel is routinely drawn at prenatal care intake and includes a type and screen. Test results were included for patients for whom age and state of residence were available. Primary payor was reported when available. Data were standardized and maintained at a central repository by data management staff at Quest Diagnostics.
RBC abs screening was performed using patient sera on the Capture-R Ready-Screen (Immucor, Norcross, GA), an automated solid-phase technology using RBC fragments from 3 donors precoated onto microtiter wells.21 Per manufacturer’s specifications, low-ionic-strength saline was used as a potentiating agent, and indicator RBCs coated with antihuman immunoglobulin G were used for reaction visualization. Screening results were recorded in binary form as positive or negative for RBC abs. Ab identification was performed using the same technology but with 11-cell panels (Capture-R Ready-ID; Immucor). Ab titers were determined using traditional hemagglutination techniques, performed in tube without potentiating agents, and recorded in whole numbers as the reciprocal of the lowest dilution at which hemagglutination could be observed macroscopically.22,23 All testing took place at Quest Diagnostics laboratories. Reagents, testing platforms, and standard operating procedures were consistent across sites. RBC abs were categorized as high, moderate, or low risk for HDFN based primarily on the 2015 Swedish national guideline, because there is no equivalent national guideline in the United States (Table 1).24
RBC abs and critical titers according to Swedish national guidelines 2015
| Risk for HDFN . | Types of RBC abs . |
|---|---|
| High risk | Anti-D |
| Anti-K | |
| Anti-c | |
| Moderate risk | Anti-C |
| Anti-e | |
| Anti-E | |
| Anti-k | |
| Anti-Fya | |
| Anti-U | |
| Low risk | Anti-Cw |
| Anti-f | |
| Anti-Jka | |
| Anti-Jkb | |
| Anti-M | |
| Anti-Kpa | |
| Anti-Kpb | |
| Anti-Yta | |
| Anti-Coa | |
| Anti-Cob | |
| Anti-Ge2,3 | |
| Titer | Management implication |
| 1-8 | Not critical for the fetus, but an indication for continued surveillance with antibody titers. The exception is anti-K where monitoring with Doppler interrogation of MCA PSV should start at titer ≥8. |
| 16-32 | Low risk of severe HDFN, but neonatal hyperbilirubinemia requiring phototherapy is possible. |
| ≥64 | Close monitoring, including Doppler interrogation of MCA PSV. Risk of need for neonatal exchange transfusion. |
| ≥128 | Close monitoring, including Doppler interrogation of MCA PSV. Intrauterine blood transfusion/neonatal exchange transfusion may be required. |
| Risk for HDFN . | Types of RBC abs . |
|---|---|
| High risk | Anti-D |
| Anti-K | |
| Anti-c | |
| Moderate risk | Anti-C |
| Anti-e | |
| Anti-E | |
| Anti-k | |
| Anti-Fya | |
| Anti-U | |
| Low risk | Anti-Cw |
| Anti-f | |
| Anti-Jka | |
| Anti-Jkb | |
| Anti-M | |
| Anti-Kpa | |
| Anti-Kpb | |
| Anti-Yta | |
| Anti-Coa | |
| Anti-Cob | |
| Anti-Ge2,3 | |
| Titer | Management implication |
| 1-8 | Not critical for the fetus, but an indication for continued surveillance with antibody titers. The exception is anti-K where monitoring with Doppler interrogation of MCA PSV should start at titer ≥8. |
| 16-32 | Low risk of severe HDFN, but neonatal hyperbilirubinemia requiring phototherapy is possible. |
| ≥64 | Close monitoring, including Doppler interrogation of MCA PSV. Risk of need for neonatal exchange transfusion. |
| ≥128 | Close monitoring, including Doppler interrogation of MCA PSV. Intrauterine blood transfusion/neonatal exchange transfusion may be required. |
Reproduced from Liu et al,24 with permission.
MCA, middle cerebral artery; PSV, peak systolic velocity.
Cohort demographic characteristics
| . | Pregnancies . | US birth certificate data . | ||
|---|---|---|---|---|
| (N = 10 252 880) . | (N = 46 423 127) . | |||
| Age, y | ||||
| <20 | 697 063 | 6.8% | 2 847 328 | 6.1% |
| 20-34 | 7 637 635 | 74.5% | 35 782 150 | 77.1% |
| ≥35 | 1 917 065 | 18.7% | 7 793 659 | 16.8% |
| Overall mean, y | 29.5 | 29 | ||
| Primary payor∗ | ||||
| Commercial insurer | 4 264 026 | 41.6% | 11 252 650 | 49.7% |
| Medicaid | 1 111 368 | 10.8% | 9 478 566 | 41.9% |
| Self-pay | 86 160 | 0.8% | 913 660 | 4.0% |
| Other | 1 823 790 | 17.8% | 973 690 | 4.3% |
| Census division | ||||
| New England | 415 265 | 4.1% | 1 772 902 | 3.8% |
| Mid Atlantic | 1 412 147 | 13.8% | 5 665 326 | 12.2% |
| South Atlantic | 2 260 046 | 22.0% | 8 832 494 | 19.0% |
| East South Central | 304 503 | 3.0% | 2 781 122 | 6.0% |
| West South Central | 1 372 830 | 13.4% | 6 419 230 | 13.8% |
| East North Central | 809 709 | 7.9% | 6 558 943 | 14.1% |
| West North Central | 471 243 | 4.6% | 3 190 253 | 6.9% |
| Mountain | 838 531 | 8.2% | 3 585 200 | 7.7% |
| Pacific | 1 991 922 | 19.4% | 7 617 667 | 16.4% |
| Calendar year | ||||
| 2010 | 900 589 | 8.8% | 3 999 386 | 8.6% |
| 2011 | 868 422 | 8.5% | 3 953 590 | 8.5% |
| 2012 | 848 041 | 8.3% | 3 952 841 | 8.5% |
| 2013 | 880 091 | 8.6% | 3 932 181 | 8.5% |
| 2014 | 879 959 | 8.6% | 3 988 076 | 8.6% |
| 2015 | 890 489 | 8.7% | 3 978 497 | 8.6% |
| 2016 | 852 857 | 8.3% | 3 945 875 | 8.5% |
| 2017 | 840 425 | 8.2% | 3 855 500 | 8.3% |
| 2018 | 844 965 | 8.2% | 3 791 712 | 8.2% |
| 2019 | 841 918 | 8.2% | 3 747 540 | 8.1% |
| 2020 | 802 106 | 7.8% | 3 613 647 | 7.8% |
| 2021 | 803 018 | 7.8% | 3 664 292 | 7.9% |
| . | Pregnancies . | US birth certificate data . | ||
|---|---|---|---|---|
| (N = 10 252 880) . | (N = 46 423 127) . | |||
| Age, y | ||||
| <20 | 697 063 | 6.8% | 2 847 328 | 6.1% |
| 20-34 | 7 637 635 | 74.5% | 35 782 150 | 77.1% |
| ≥35 | 1 917 065 | 18.7% | 7 793 659 | 16.8% |
| Overall mean, y | 29.5 | 29 | ||
| Primary payor∗ | ||||
| Commercial insurer | 4 264 026 | 41.6% | 11 252 650 | 49.7% |
| Medicaid | 1 111 368 | 10.8% | 9 478 566 | 41.9% |
| Self-pay | 86 160 | 0.8% | 913 660 | 4.0% |
| Other | 1 823 790 | 17.8% | 973 690 | 4.3% |
| Census division | ||||
| New England | 415 265 | 4.1% | 1 772 902 | 3.8% |
| Mid Atlantic | 1 412 147 | 13.8% | 5 665 326 | 12.2% |
| South Atlantic | 2 260 046 | 22.0% | 8 832 494 | 19.0% |
| East South Central | 304 503 | 3.0% | 2 781 122 | 6.0% |
| West South Central | 1 372 830 | 13.4% | 6 419 230 | 13.8% |
| East North Central | 809 709 | 7.9% | 6 558 943 | 14.1% |
| West North Central | 471 243 | 4.6% | 3 190 253 | 6.9% |
| Mountain | 838 531 | 8.2% | 3 585 200 | 7.7% |
| Pacific | 1 991 922 | 19.4% | 7 617 667 | 16.4% |
| Calendar year | ||||
| 2010 | 900 589 | 8.8% | 3 999 386 | 8.6% |
| 2011 | 868 422 | 8.5% | 3 953 590 | 8.5% |
| 2012 | 848 041 | 8.3% | 3 952 841 | 8.5% |
| 2013 | 880 091 | 8.6% | 3 932 181 | 8.5% |
| 2014 | 879 959 | 8.6% | 3 988 076 | 8.6% |
| 2015 | 890 489 | 8.7% | 3 978 497 | 8.6% |
| 2016 | 852 857 | 8.3% | 3 945 875 | 8.5% |
| 2017 | 840 425 | 8.2% | 3 855 500 | 8.3% |
| 2018 | 844 965 | 8.2% | 3 791 712 | 8.2% |
| 2019 | 841 918 | 8.2% | 3 747 540 | 8.1% |
| 2020 | 802 106 | 7.8% | 3 613 647 | 7.8% |
| 2021 | 803 018 | 7.8% | 3 664 292 | 7.9% |
Primary payor was only available in US birth certificate data from 2016 to 2021.
Estimates of prevalence were reported per 100 000 pregnancies. To estimate the prevalence of critical RBC abs titer for high- and moderate-risk RBC abs, we used a random sampling method to impute missing critical RBC ab titers for each ab in a calendar year.
Noting the potential for weighting to be skewed by data limitations, we developed 2 sensitivity analyses of our weighting method. The first (supplemental Figure 2) was undertaken to account for the possibility that twin and higher order multiples in the livebirth data may only have 1 record in the Quest Diagnostics data set. Using birth certificates from the US Natality Index from the years 2016 to 2021, we excluded second and subsequent births from the same delivery (US natality data from 2010-2015 did not include a variable allowing for the removal of multiple observations for the same delivery). We then recalculated the weights using the same approach as outlined above. The second sensitivity analysis (supplemental Figure 3) was performed in recognition that US Natality Index data only include pregnancies that result in live birth, in contrast to Quest Diagnostics data, which also include pregnancies ending in loss or termination after completion of the prenatal panel. To assess whether this affected our weights, we used the most recently available at the time of analysis (2012-2017) state-specific data regarding estimated number of total pregnancies from the Guttmacher Institute, a research and policy nongovernmental organization.31 We then compared weights for 2012 to 2017 observations by our live-birth-based methodology with those that would be generated using the total pregnancy methodology.
All estimates were calculated using methods accounting for weighting and stratification of the resulting data set and reported with 95% confidence intervals. Cochrane-Armitage tests based on linear regression were used to assess temporal trends in alloimmunization; P value < .05 was considered statistically significant. All statistical analyses were performed using Stata Statistical Software, version 17 (StataCorp, College Station, TX) and R Software, version 4.2.1 (https://www.R-project.org/). The study protocol was reviewed by Western Copernicus Group institutional review board and deemed exempt. Requests for access to the data sets used in this study should be addressed to the senior author.
Results
Of the 10.2 million pregnancies in our data set from 2010 through 2021, a total of 9.9 million met the inclusion criteria. Age was recorded for almost all patients (99.99%), state of residence for 9.9 million (96.3%), and primary payor for 7.0 million (71.1%). Mean patient age was 29.5 (standard deviation, 7.2) years, with 6.8% of patients aged <20 years, 74.5% aged 20 to 34 years, and 18.7% aged >35 years. During this period, birth certificate data confirmed 46.4 million births in the United States, corresponding to ∼71.4 million total pregnancies. Data describing the number of unique pregnancies from 2010 to 2021 were stratified by age, primary payor, calendar year, and all 9 US Census Divisions (Table 2).
From January 2010 to December 2021, of 9 876 196 pregnancies in our cohort, 147 262 (1.5%) had a positive ab screen, corresponding to a national estimate of 1518 per 100 000. Ab specificity was conclusively identified in 89 249 (60.6%) of these or 0.9% of total pregnancies, whereas the remainder had ab screens of uncertain specificity, for example, weak abs. Of identified RBC abs in the cohort, high-risk abs accounted for 74.3%, moderate-risk abs for 13.5%, and low-risk abs for 12.3% of cases. Anti-D was the most common ab, accounting for 64.1% of all RBC abs, corresponding to an estimated national rate of 586 per 100 000 pregnancies. The prevalence of other high-risk RBC abs for HDFN was 68 per 100 000 for anti-K and 29 per 100 000 for anti-c. Critical titers were observed in 10.2% of high-risk and 5.5% of moderate-risk abs; titers were missing in 5.2% of high-risk and 13.8% of moderate-risk abs. Most pregnancies (67.6%) with anti-K abs had critical titers; a small proportion of pregnancies with other high-risk RBC abs had critical ab titers (anti-D, 3.6%; anti-c, 6.6%). The overall prevalence of critical titers for anti-D was estimated at 21 per 100 000 pregnancies (Table 3).
Estimates of national prevalence of alloimmunization in early pregnancy
| Risk of HDFN . | Rate per 100 000 pregnancies (95% CI) . | |
|---|---|---|
| Pregnancies . | ||
| (n = 9 876 196) . | ||
| RBC ab detected . | Critical titer∗ . | |
| High risk | ||
| Anti-D | 586 (553-618) | 21 (20-22) |
| Anti-K | 68 (64-71) | 46 (44-48) |
| Anti-c | 29 (26-31) | 1.9 (1.5-2.2) |
| Any† | 679 (645-714) | 69 (66-71) |
| Moderate risk | ||
| Anti-E | 110 (105-116) | 8 (7-9) |
| Anti-C | 30 (26-33) | 2.6 (2.2-3.0) |
| Anti-e | 4 (3-5) | 0.06 (0.01-0.12) |
| Anti-k | 0.01 (0-0.03) | 0.01 (0-0.03) |
| Anti-Fya | 13 (12-14) | 3.1 (2.7-3.6) |
| Anti-U | 0.03 (0-0.07) | 0 |
| Any‡ | 123 (116-130) | 6.8 (5.8-7.7) |
| Low risk∗∗ | ||
| Any | 112 (103-121) | Not applicable |
| Risk of HDFN . | Rate per 100 000 pregnancies (95% CI) . | |
|---|---|---|
| Pregnancies . | ||
| (n = 9 876 196) . | ||
| RBC ab detected . | Critical titer∗ . | |
| High risk | ||
| Anti-D | 586 (553-618) | 21 (20-22) |
| Anti-K | 68 (64-71) | 46 (44-48) |
| Anti-c | 29 (26-31) | 1.9 (1.5-2.2) |
| Any† | 679 (645-714) | 69 (66-71) |
| Moderate risk | ||
| Anti-E | 110 (105-116) | 8 (7-9) |
| Anti-C | 30 (26-33) | 2.6 (2.2-3.0) |
| Anti-e | 4 (3-5) | 0.06 (0.01-0.12) |
| Anti-k | 0.01 (0-0.03) | 0.01 (0-0.03) |
| Anti-Fya | 13 (12-14) | 3.1 (2.7-3.6) |
| Anti-U | 0.03 (0-0.07) | 0 |
| Any‡ | 123 (116-130) | 6.8 (5.8-7.7) |
| Low risk∗∗ | ||
| Any | 112 (103-121) | Not applicable |
CI, confidence interval.
≥4 for anti-K and ≥16 for all other high-risk and moderate-risk abs.
Includes: anti-Cw, anti-f, anti-Jka, anti-Jkb, anti-M, anti-S, anti-s, anti-Fyb, anti-Lua, anti-Lub, anti-Kpa, anti-Kpb, anti-Yta, anti-Coa, anti-Cob, anti-Ge2,3.
Accounted for any high-risk antibody combination detected in a test (0.3%).
Accounted for any moderate-risk ab combination detected in a test (0.5%) and excluded those combinations with high-risk abs (3.1%).
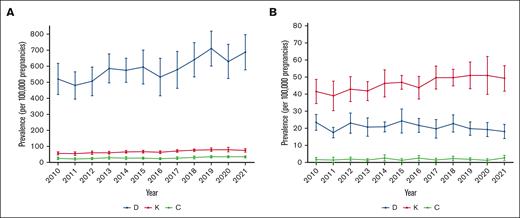
The prevalence of all 3 high-risk abs increased incrementally over the 12-year period for positive ab detection (all P < .001; Figure 1A). This was most notable for anti-D abs, in which the prevalence rose 43.0% from 481 per 100 000 pregnancies in 2011 to 688 per 100 000 in 2021. Similar rises occurred for the other high-risk abs over the same period (anti-c, 63.6%; anti-K, 36.4%). The prevalence of critical titers of both anti-K and anti-c increased, whereas that of anti-D decreased over the 12-year period (P < .001 for both anti-K and anti-D; P =.03 for anti-c; Figure 1B). The most significant change was for the critical titer of anti-K with its prevalence increased 25.6% from 39 per 100 000 in 2011 to 49 per 100 000 in 2021. It is also worth noting that the prevalence of the critical titer of anti-D decreased 21.7% from 23 per 100 000 in 2010 to 18 per 100 000 in 2021.
Temporal trends of prevalence of and critical titer of high-risk alloantibodies at initial prenatal visit from 2010 to 2021. (A) The temporal increase in positive detection of the 3 alloantibodies (anti-D, anti-c and anti-Kell) considered high-risk for alloantibodies over a 12-year period. This temporal trend was significant for all 3 alloantibodies (all P < .001) and most notable for anti-D, for which the prevalence rose 43.0% from 481 per 100 000 pregnancies in 2011 to 688 per 100 000 in 2021. (B) The frequency of critical titers for all 3 high-risk abs. These frequencies changed over the 12-year period (P < .001 for both anti-K and anti-D; P = .03 for anti-c). The prevalence of critical titer of anti-K increased 25.6% from 39 per 100 000 in 2011 to 49 per 100 000 in 2021, whereas that of anti-D decreased 21.7% from 23 per 100 000 in 2010 to 18 per 100 000 in 2021.
Temporal trends of prevalence of and critical titer of high-risk alloantibodies at initial prenatal visit from 2010 to 2021. (A) The temporal increase in positive detection of the 3 alloantibodies (anti-D, anti-c and anti-Kell) considered high-risk for alloantibodies over a 12-year period. This temporal trend was significant for all 3 alloantibodies (all P < .001) and most notable for anti-D, for which the prevalence rose 43.0% from 481 per 100 000 pregnancies in 2011 to 688 per 100 000 in 2021. (B) The frequency of critical titers for all 3 high-risk abs. These frequencies changed over the 12-year period (P < .001 for both anti-K and anti-D; P = .03 for anti-c). The prevalence of critical titer of anti-K increased 25.6% from 39 per 100 000 in 2011 to 49 per 100 000 in 2021, whereas that of anti-D decreased 21.7% from 23 per 100 000 in 2010 to 18 per 100 000 in 2021.
Our first sensitivity analysis accounting for multiple births at the same delivery found that the weights estimated by our original approach were extremely well correlated with weights based on the exclusion of multiple births from 2016 to 2021 US natality data. This suggested that our original weighting was unlikely to significantly alter our estimates of alloimmunization rates. These findings are presented in supplemental Figure 2. In our second sensitivity analysis, weights were higher when using Guttmacher pregnancy data, because there are more pregnancies than births, and thus, the Quest Diagnostics data are being asked to represent a larger number of pregnancies. However, our weights remained strongly correlated (R2 = 0.97), suggesting that using natality data was unlikely to significantly bias our estimates of the prevalence of alloimmunization. The findings are presented in supplemental Figure 3.
Discussion
In this large, nationwide study in the United States, estimated prevalence of positive RBC antibody screen was 1518 per 100 000 pregnancies at the initiation of prenatal care. Of RBC abs identified, anti-D was the most common, comprising more than half (64.1%). Most RBC abs identified (74.3%) are high risk for development of HDFN. The majority of anti-K ab results (67.6%) were at critical titer at the time of early prenatal care (time of initial obstetric panel testing).
The estimated prevalence of RBC abs was consistent with that of a previously reported rate from a single center in the United States.19 This is higher than the ab prevalence reported in another single-center US study (0.74%) or other high-income countries (HICs), including Spain (0.63%), Australia (0.73%), Sweden (0.38%), Norway (0.73%), Iceland (1.04%), and Canada (0.36%).13-15,17,18,20 Our data suggest that prevalence of maternal alloimmunization to all antigens at high risk for development of HDFN is rising in the United States. Passively acquired anti-D after Rh immunoglobulin (RhIg) administration may contribute but does not explain consistent increases in the prevalence of anti-Kell and anti-c.32,33 Possible explanations may include increasing ethnographic and genetic diversity in the United States, in prenatal antibody screening, in survival from congenital hemoglobinopathies requiring blood transfusion, and in maternal age giving rise to a longer period for potential antigen exposure before conception.34,35 In addition, although the use of blood transfusion in the United States has been declining in recent years, the use of allogeneic blood transfusion has been significantly higher in women than men, even when controlling for age and comorbidities.36-38,39
An unexpected result from this study was the particularly high rate of anti-D detected, inconsistent with reports from the other US-based or international reports from HICs.40 Given the inability to distinguish between passively acquired anti-D due to RhIg (anti-DRG) and patient-produced anti-D (also known as anti-D alloimmunization) with testing data alone, it is difficult to interpret the increasing prevalence of anti-D antibody observed in this study’s cohort. One possible explanation is the increased use of RhIg, leading to the detection of anti-DRG abs.41 In addition, the decrease in alloimmunization rates cited by other countries could be due to variations in screening or RhIg delivery practices over time. In several European countries, only Rh(D)-negative patients pregnant with cell-free fetal DNA–proven Rh(D)-positive fetuses are given RhIg, a possible cause of lower RhIg delivery resulting in less anti-DRG abs interfering with testing.42,43 Furthermore, some HICs have national patient databases allowing for more comprehensive tracking of RhIg delivery and other patient testing data.17,43 This level of granularity would allow for researchers to more accurately predict and report on active vs passive anti-D rates. Possible reasons for a true increase in anti-D alloimmunization rates in the United States would include the following: a more ethnically diverse patient population with varying rates in antigen expression allowing for increased incidence of antigen exposure in antigen negative individuals; a diverse socioeconomic patient population and lack of universal access to health care causing variable adoption of RhIg use at the ideal times in pregnancy; or an increase in immigrant populations from low-middle income countries with high rates of alloimmunization and limited access to RhIg before entry into the United States.31,36,35,39,44 Varied dose regimens of RhIg are unlikely to be a contributor, because the typical routine antenatal dosage given in Europe is the same or less than that in North America (300 μg [1500 IU] at 28-30 weeks).45 Although the overall trend in anti-D alloimmunization is unable to be adequately characterized in this cohort, the decreasing rates of anti-D critical titer cases, which almost certainly represent real alloimmunization cases, whereas cases of critical titer alloimmunization in anti-c and anti-K increase would suggest that rates of anti-D alloimmunization are declining.
Anti-K is the antibody most often associated with critical titers in our study. This is an expected finding, given the widespread use of K-incompatible blood in both child and adult transfusion and the lower critical titer threshold used for anti-K abs.46,47 More surprisingly, despite ongoing efforts to reduce alloimmunization, the overall prevalence of high-risk RBC abs and critical titers in the United States continues to rise. The true burden of RBC alloimmunization in the United States is poorly understood and understudied. It is established, however, that newborns with HDFN are more likely to require transfusion, cesarean delivery, neonatal intensive care admission, and longer length of stay than healthy and other sick newborns; neonates who are Black, female, and from the American South are disproportionately affected.2 In this context, several initiatives to reduce alloimmunization in the United States are worthy of consideration. In the Netherlands, routine national use of K-compatible blood has been shown to reduce the incidence of K alloimmunization from 67.9 to 20.2 per 100 000 pregnancies and the total number of pregnancies at high risk of HDFN from 9.7 to 4.2 per 100 000.48 This finding has been replicated for anti-c and anti-E in several studies.49-51
Strengths of our study include our large, nationwide cohort, representing nearly 10 million of all pregnancies in the United States from a wide spectrum of health insurers (primary payors) from 2010 to 2021. Given the absence of nationalized data, we believe, to our knowledge, this is by far the largest prenatal ab cohort reported in the United States to date, representing a wide geographic and socioeconomic sample of the US population. Our statistical weighting methods were also a strength, adjusting for potential regional and temporal variation in the proportion of pregnant patients using Quest Diagnostics services. Our sensitivity analyses using US birth certificate and state-specific pregnancy data demonstrated that, although multiple gestations and pregnancies that do not result in live birth are not distinguishable in our data set, the accuracy of our geographical and temporal weighting is unaffected.
This study has several significant limitations. Firstly, our sample, although large, may not be representative of the US population as a whole. Quest Diagnostics serves a full spectrum of both privately and publicly insured patients nationwide. The proportion of patients served by Quest Diagnostics, however, varies by geography and calendar year. Secondly, individual patient-level data on race, ethnicity, gestational age at time of initial presentation, gravidity, parity, medical comorbidities, and clinical course of pregnancy are unavailable, because these data are not made available to Quest Diagnostics at the time of client request. As a result, demographic data are limited only to patient’s age, address, primary payor, and calendar year in which the blood specimens were obtained. We acknowledge that lack of data on race and ethnicity in particular limits our ability to study important demographic differences in alloimmunization prevalence in the United States, given that recipient race is known to be independently predictive of RBC alloimmunization.2,52 In this regard, we noted that US Census data from 2020 demonstrate significant variation in race and ethnicity between the 9 US census divisions (supplementary Table 5).53 In 2020, up to 78.5% of people in West North Central Division (North Dakota, South Dakota, Minnesota, Iowa, Missouri, Nebraska, and Kansas) were White vs 47% in Pacific (Washington, Oregon, and California); 21.1% of people in South Atlantic (West Virginia, Delaware, Maryland, Virginia, North Carolina, South Carolina, Georgia, and Florida) were Black vs 4.0% in Mountain (Montana, Idaho, Wyoming, Nevada, Utah, Colorado, Arizona, and New Mexico); 14% of Pacific were Asian vs 1.6% in East South Central (Alabama, Mississippi, Tennessee, and Kentucky). Thus, we believe our geographically and temporally weighted estimates by calendar year and US Census Division represent the best available partial control both for varying proportions of patients served by year and geography and for regional variation in race and ethnicity.
Finally, we note that our data set includes all pregnancies whether culminating in live birth, miscarriage, termination of pregnancy, or fetal demise. By contrast, US Natality Index only includes pregnancies resulting in a live birth. There is also no way to definitively determine whether a second RBC abs screening panel on the same patient in the same year reflects repeat screening later in pregnancy or initial screening in a subsequent pregnancy, although our sensitivity analyses suggest the effect on our weighting is minimal. Thirdly, despite standardization, inherent limitations of RBC abs testing and reporting error remain. For example, in our cohort, only 60.6% of positive ab screens resulted in conclusive ab identification. Ab titers were missing in 5.2% of high-risk abs and 13.8% of moderate-risk abs, the majority due to the test not being performed or an insufficient quantity of patient specimen volume for titration. To that end, we used an imputation method for missing titers based on the distribution of observed titers for each ab by calendar year.
RBC alloimmunization increases burden of disease, maternal and fetal mortality and health care costs.54 We believe the results of our study should refocus national attention toward improved prenatal ab testing techniques and measures to prevent of RBC alloimmunization in the United States. Several initiatives to reduce alloimmunization merit further consideration, including development of the following: a national blood donor database for better allocation of antigen matched blood to patients undergoing chronic transfusions; routine extended prophylactic antigen matching for RhD, Rhc, and Kell in females aged <50 years; RhD antigen genotyping for patients with serologically weak D antigens to identify possible weak D variants, which would not require administration of RhIg; prenatal fetal RhD screening in RhD women to target prenatal RhIg prophylaxis; restrictions in the use of low-titer group O+ whole blood in females aged <50 years; routine transfusion of Kell-negative blood in females aged <50 years; and routine optimization of preoperative hemoglobin levels to reduce transfusion exposure.42,50,55-59 Lastly, prevention of trauma such as motor vehicle accidents and gun violence can play an important part in reducing the need for transfusion.44,60,61
Conclusion
Our findings suggest that the prevalence of alloimmunization as detected by screening in pregnancy in the United States may be higher than that in other HICs and has continued to rise since 2010. RBC abs conferring high risk of development of HDFN constitute the majority of RBC abs identified. Alloimmunization to RBC abs is an acquired and largely preventable condition that represents an ongoing challenge to transfusion, preconception, prenatal, and neonatal care. Given the significant sequelae for patients requiring transfusion of blood products and the risk of developing HDFN during pregnancy, new initiatives are required to reduce alloimmunization in the United States.
Acknowledgments
J.J.F. was supported by the Eunice Kennedy Shriver National Institute of Child Health and Human Development of the National Institutes of Health (award K12HD103083). The content is solely the responsibility of the authors and does not represent the official views of the National Institutes of Health.
Authorship
Contribution: J.Z.L. and Z.C. performed the primary data analytics; R.P.S. authored the initial and final draft; K.J.M., J.J.F., E.A., J.Z.L., Z.C., L.B., D.P.A., and H.W.K. edited and reviewed drafts and approved the submission; and all authors developed the study and statistical methods designs, and participated in the data review.
Conflict-of-interest disclosure: J.Z.L., Z.C., L.B., D.P.A., and H.W.K. are employees of Quest Diagnostics. Z.C., L.B., D.P.A., and H.W.K. own Quest Diagnostics stock. K.J.M. is a consultant and investigator for Jannsen Pharmaceuticals Inc; serves as the overall principal investigator for the phase 2 trial of nipocalimab (UNITY); has received funding from Momenta Pharmaceuticals Inc paid on his behalf to the McGovern Medical School-UTHealth, and from Janssen Pharmaceuticals Inc paid on his behalf to Dell Medical School at The University of Texas at Austin for a clinical trial on a monoclonal antibody for the treatment of hemolytic disease of fetus and newborn (HDFN); has served on the steering committees and advisory boards for clinical studies for Momenta Pharmaceuticals Inc and Janssen Pharmaceuticals but has not received funding for these activities; receives royalty funding from UpToDate Inc for authorship on various chapters; consulting fees from Health Management Associates Inc for consultation on the formation of fetal centers and BillionToOne Inc paid on his behalf to Dell Medical School at The University of Texas at Austin; honoraria from GLC Healthcare, Inc for podcast content on HDFN; and serves as a nonpaid consultant for Immunology for Janssen Pharmaceuticals Inc. The remaining authors declare no competing financial interests.
Correspondence: Ronan P. Sugrue, Obstetrics & Gynecology, Duke University Hospital, 2608 Erwin Rd, Ste 200, Durham, NC 27705; email: ronansugrue@mail.harvard.edu.
References
Author notes
Original data or search protocol are available on request from the corresponding author, Ronan P. Sugrue (ronansugrue@mail.harvard.edu).
The full-text version of this article contains a data supplement.