HCT can mitigate the possible negative effect of JAK2V617F mutation in patients with PMF and PPV-MF.
High allele burden in patients with PET-MF is associated with excess risk of NRM in the era of JAK inhibitors.
Visual Abstract
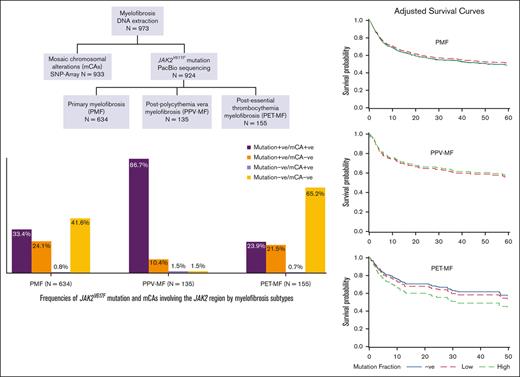
JAK2V617F is the most common driver mutation in primary or secondary myelofibrosis for which allogeneic hematopoietic cell transplantation (HCT) is the only curative treatment. Knowledge of the prognostic utility of JAK2 alterations in the HCT setting is limited. We identified all patients with MF who received HCT between 2000 and 2016 and had a pre-HCT blood sample (N = 973) available at the Center of International Blood and Marrow Transplant Research biorepository. PacBio sequencing and single nucleotide polymorphism–array genotyping were used to identify JAK2V617F mutation and associated mosaic chromosomal alterations (mCAs), respectively. Cox proportional hazard models were used for HCT outcome analyses. Genomic testing was complete for 924 patients with MF (634 primary MF [PMF], 135 postpolycythemia vera [PPV-MF], and 155 postessential thrombocytopenia [PET-MF]). JAK2V617F affected 562 patients (57.6% of PMF, 97% of PPV-MF, and 42.6% of PET-MF). Almost all patients with mCAs involving the JAK2 region (97.9%) were JAK2V617-positive. In PMF, JAK2V617F mutation status, allele burden, or identified mCAs were not associated with disease progression/relapse, nonrelapse mortality (NRM), or overall survival. Almost all PPV-MF were JAK2V617F-positive (97%), with no association between HCT outcomes and mutation allele burden or mCAs. In PET-MF, JAK2V617F high mutation allele burden (≥60%) was associated with excess risk of NRM, restricted to transplants received in the era of JAK inhibitors (2013-2016; hazard ratio = 7.65; 95% confidence interval = 2.10-27.82; P = .002). However, allele burden was not associated with post-HCT disease progression/relapse or survival. Our findings support the concept that HCT can mitigate the known negative effect of JAK2V617F in patients with MF, particularly for PMF and PPV-MF.
Introduction
Myelofibrosis (MF) is a BCR-ABL1–negative myeloproliferative neoplasm characterized by stem cell–derived clonal myeloproliferation and bone marrow fibrosis. It can either develop de novo (primary MF [PMF]) or secondary to polycythemia vera (PV) or essential thrombocythemia (ET).1 The median overall survival (OS) in MF is ∼5 years.2 However, prognosis is dismal in patients who progress to acute myeloid leukemia with an expected 98% mortality at a median of 2.5 months.3 Leukemic transformation is reported in ∼14% of PMF,4 8.2% of post-PV MF (PPV-MF), and 11.5% of post-ET MF (PET-MF).5 Other MF-associated comorbidities include cardiovascular complications, recurrent infections, and bleeding.6 The Dynamic International Prognostic Scoring System (DIPSS) and DIPSS-plus are widely used clinical prognostic algorithms for MF, primarily using information on blood counts, patient age, and constitutional symptoms for DIPSS, in addition to karyotypes, platelet counts and transfusion dependence for DIPSS-plus. Other MF molecular–based (with mutation ± cytogenetic information) prognostic tools include the MIPSS70-plus (Mutation-enhanced International Prognostic Score System for Transplant-age patients),7 GIPSS (Genetically Inspired Prognostic System),8 and the MYSEC-PM (MF secondary to PV and ET–prognostic model).9 These scores were developed to predict survival and were shown to guide treatment decisions for those patients.10-13
Several driver mutations in patients with MF (JAK2V617F the most common) have been linked to disease progression and clonal evolution, with suggested differences between PMF, PPV-MF, and PET-MF.14-18 This discovery led to the development of JAK inhibitors that were first introduced in 2012 and showed efficacy in palliating constitutional symptoms, and possibly improving OS.19,20 However, JAK inhibitors do not reverse bone marrow fibrosis or decrease the risk of leukemic transformation and could increase patient risk of nonmelanoma skin cancer and lymphoma.21,22
Cytogenetic abnormalities in MF are common, with unfavorable profile that includes deletions in chr 5/5q, 7/7q, 12p, or 17q, gain in chr8, inv(3), or 11q23 rearrangement.23 The full profile of known cytogenetic abnormalities in MF was reviewed by Hussein et al.24 The emergence of microarray chromosomal detection tools, such as single nucleotide polymorphism (SNP)-array, identified copy-neutral heterozygosity (CNLOH) changes commonly affecting chr9. Other detected CNLOHs in MF were seen on chr14, chr1, and chr1116. The prognostic value and clinical utility of array testing for chromosomal alterations in myeloid neoplasms has been discussed in a recent evidence-based review.25 For myeloproliferative neoplasms, chromosomal loss of 5q, 7q, 12p, and 17p and trisomy 8 carried the strongest evidence of poor prognosis. Some of the promising and emerging detected alterations for clinical applications include CNLOHs spanning MPL, EZH2, CUX, JAK2, and CBL25.
Allogeneic hematopoietic cell transplantation (HCT) is the only curative treatment modality for MF yet is usually reserved for patients in the intermediate- and high-risk group because of the risks of treatment-related morbidity and mortality. Despite improvements in post-HCT outcomes in recent years, OS is still unsatisfactory (5 years OS = 50%-60%),26,27 with relapse and graft-versus-host disease the main causes of death.26 There are limited data on the prognostic value of JAK2V617F mutation or associated chromosomal alterations in patients with MF undergoing HCT, and whether possible differences based on the disease subtypes exist. This is particularly important because results may guide clinical decisions related to the use of JAK inhibitors after HCT for patients with MF.
In this large study, we focused on JAK2 alterations because JAK2V617F mutation is the most common driver mutation in MF, and target therapy is widely used. The study aimed to (1) evaluate the relationship between JAK2V617F mutation status and post-HCT OS, nonrelapse mortality (NRM), and disease relapse/progression across MF subtypes and (2) explore if the presence of mosaic chromosomal aberrations (mCAs) spanning the JAK2 region modifies the detected associations.
Methods
MF cohort
We identified all patients who received allogeneic HCT for MF between 2000 and 2016 with clinical data and pre-HCT peripheral blood sample available at the Center for International Blood and Marrow Transplant Research (CIBMTR) registry and biorepository (N = 973 from 99 transplant centers). CIBMTR is a research collaboration between the National Marrow Donor Program/Be The Match and the Medical College of Wisconsin, where clinical data and biospecimens from the majority of unrelated donor HCT have accrued since 1987; sample collection for related donor HCT from select centers started in 2006. The CIBMTR ensures high data quality by actively auditing all participating transplant centers; https://www.cibmtr.org/DataManagement/AuditProgram/Pages/index.aspx The study was approved by the National Marrow Donor Program Institutional Review Board. All patients or their guardians provided written informed consent for the research use of their samples and clinical data.
Genomic studies
JAK2 PacBio sequencing for the study samples was originally completed as part of our recent genome-wide association study in MF, in which details of performed genomic studies were described.16 In brief, DNA from peripheral blood samples collected within 30 days before the start of HCT conditioning regimen was extracted using the Qiagen QIAsymphony kit. Targeted PacBio Single Molecule Real-Time sequencing was used to detect JAK2V617F mutation with an achieved average read depth of 7077 (median = 6629.5; minimum = 3155 and maximum = 11 927). mCAs involving JAK2 were identified using SNP-array genotype data generated by the Illumina Infinium Global Screening Array-24v1-0 using Mosiac Chromosomal Alterations software (https://github.com/freeseek/mocha) and BAFSegmentation software (http://baseplugins.thep.lu.se/wiki/se.lu.onk.BAFsegmentation). This method classifies the type of chromosomal alteration into gain, loss, or CNLOH and quantifies affected cell fraction.
Statistical analysis
We used the Kaplan-Meier estimator to calculate the probability of OS and the cumulative incidence estimator for relapse/disease progression and NRM, in which each was treated as a competing event for the other. Follow-up started at the day of transplantation and ended at outcome of interest, death, 5 years after HCT, or end of follow-up in January 2020. For the main analyses, we ended follow-up at 5 years to avoid unreliable estimates with small number of events in the later follow-up time (median follow-up of survivors = 60.5 months for PMF, 59.6 months for PPV-MF, and 52.6 months for PET-MF). Results including the total follow-up time is provided in the supplemental Material. Cox proportional hazard or cause-specific hazard models were used for multivariable analyses of OS or relapse/disease progression and NRM, respectively. Information on relapse was based on transplant center definition. The Schoenfeld residuals test was used to assess the proportional hazard assumption and stratification was used for variables not meeting the proportionality assumption. Clinical variables included in the final models were selected by a stepwise procedure with P = .15 for model entry and retention. Final models for OS were adjusted for patient age, year of HCT, splenectomy before HCT, DIPSS, recipient-donor cytomegalovirus serostatus match, and donor type. NRM models were adjusted for patient age, cytomegalovirus serostatus match, year of HCT, graft type, splenectomy, donor type, and conditioning intensity. Relapse/disease progression models were adjusted for splenectomy, conditioning intensity, DIPSS, and graft-versus-host disease prophylaxis and stratified based on the year of HCT. All analyses were conducted separately based on the MF disease subtype (PMF, PPV-MF, and PET-MF). We used the disease-specific median value rounded to the nearest 10 for simplicity as the study cut-off point to define high and low allele burden (60% for PMF and PET-MF because the median allele burden was 58% in PMF and 59% in PET-MF, and 90% for PPV-MF). HCT outcome analyses for PPV-MF were performed in mutation positives only (because only 4 patients were without mutation) with a focus on associations with allele burden. All statistical tests were two-sided, and P ≤ .01 was considered statistically significant to minimize the possibility of testing-related false discovery.
Results
The study included 924 patients with MF who had genomic information from both PacBio sequencing and SNP-array mCA analysis. JAK2V617F mutation was detected for 562 patients (60.8%), with noted differences based on the disease subtype: the frequencies of JAK2V617F mutation according to the MF subtypes were 57.6% in patients with PMF, 97% in PPV-MF, and 42.6% in PET-MF (P < .0001). Compared with those havingJAK2V617F mutation–negative results, patients with JAK2V617F mutation were older in age (P = .001) and were more likely to have received reduced intensity conditioning regimen (54.4% of those with mutation-positive status vs 48.6% of those with negative status; P = .02; Table 1). Although the majority of PMF cases were male (64.2%), 52.6% of PPV-MF and 56.1% of PET-MF were female (P < .0001). Also, as expected, the time between diagnosis and HCT was significantly longer for PPV-MF and PET-MF than for PMF (P < .0001; supplemental Table 1).
Patient demographics, disease- and transplant-related factors by JAK2V617Fmutation status
| . | Mutation negative N = 362 . | Mutation positive N = 562 . | P . |
|---|---|---|---|
| Recipient age (y) | .001 | ||
| <40 | 31 (8.56) | 21 (3.74) | |
| 40 to <50 | 58 (16.02) | 67 (11.92) | |
| 50 to <60 | 138 (38.12) | 218 (38.79) | |
| ≥60 | 135 (37.29) | 256 (45.55) | |
| Recipient sex | .10 | ||
| Male | 223 (61.60) | 316 (56.23) | |
| Female | 139 (38.40) | 246 (43.77) | |
| KPS | .32 | ||
| <90 | 145 (40.06) | 243 (43.24) | |
| 90-100 | 205 (56.63) | 308 (54.80) | |
| Missing | 12 (3.31) | 11 (1.96) | |
| Disease subtype | |||
| Primary | 269 (74.31) | 365 (64.95) | <.0001 |
| PPV-MF | 4 (1.10) | 131 (23.31) | |
| PET-MF | 89 (24.59) | 66 (11.74) | |
| Conditioning intensity | .02 | ||
| Myeloablative | 186 (51.38) | 245 (43.59) | |
| Reduced intensity/nonmyeloablative | 176 (48.62) | 317 (54.41) | |
| Conditioning regimen | .0003 | ||
| Flu + Bu ± other | 147 (40.61) | 261 (46.44) | |
| Flu + Mel ± other | 82 (22.65) | 167 (29.72) | |
| Flu + TBI ± other | 31 (8.56) | 35 (6.23) | |
| Others7 | 102 (28.18) | 99 (17.62) | |
| GVHD prophylaxis | .19 | ||
| CNI + MMF ± others | 68 (18.78) | 134 (23.84) | |
| CNI + MTX ± others | 224 (61.88) | 327 (58.19) | |
| Others | 70 (19.34) | 101 (17.97) | |
| DIPSS at transplant | .21 | ||
| Low | 26 (7.18) | 46 (8.19) | |
| Intermediate-1 | 74 (20.44) | 138 (24.56) | |
| Intermediate-2/high | 112 (30.94) | 142 (25.27) | |
| Missing | 150 (41.44) | 236 (41.99) | |
| Splenectomy before HCT | .30 | ||
| No | 185 (51.10) | 265 (47.15) | |
| Yes | 4 (1.10) | 12 (2.14) | |
| Unknown | 173 (47.79) | 285 (50.71) | |
| Time between diagnosis and HCT (mo) | .38 | ||
| <12 | 128 (35.56) | 185 (33.27) | |
| 12 to <24 | 58 (16.11) | 74 (13.31) | |
| 24 to <72 | 76 (21.11) | 139 (25.00) | |
| ≥72 | 98 (27.22) | 158 (28.42) | |
| Donor-recipient CMV serostatus | .68 | ||
| Positive-positive | 85 (23.48) | 150 (26.69) | |
| Positive-negative | 59 (16.30) | 76 (13.52) | |
| Negative-positive | 87 (24.03) | 141 (25.09) | |
| Negative-negative | 125 (34.53) | 186 (33.10) | |
| Missing | 6 (1.66) | 9 (1.60) | |
| Donor type | .41 | ||
| Unrelated | 304 (83.98) | 483 (85.94) | |
| Related | 58 (16.02) | 79 (14.06) | |
| Cytogenetics at transplant | .46 | ||
| Favorable normal | 110 (30.39) | 171 (30.43) | |
| Favorable other | 58 (16.02) | 70 (12.46) | |
| Adverse | 54 (14.92) | 86 (15.30) | |
| Missing | 140 (38.67) | 235 (41.82) | |
| Stem cell source | .31 | ||
| Bone marrow | 43 (11.88) | 55 (9.79) | |
| Peripheral blood | 319 (88.12) | 507 (90.21) | |
| Year at transplant | .65 | ||
| 2000-2004 | 22 (6.08) | 40 (7.12) | |
| 2005-2009 | 79 (21.82) | 111 (19.75) | |
| 2010-2016 | 261 (72.10) | 411 (73.13) |
| . | Mutation negative N = 362 . | Mutation positive N = 562 . | P . |
|---|---|---|---|
| Recipient age (y) | .001 | ||
| <40 | 31 (8.56) | 21 (3.74) | |
| 40 to <50 | 58 (16.02) | 67 (11.92) | |
| 50 to <60 | 138 (38.12) | 218 (38.79) | |
| ≥60 | 135 (37.29) | 256 (45.55) | |
| Recipient sex | .10 | ||
| Male | 223 (61.60) | 316 (56.23) | |
| Female | 139 (38.40) | 246 (43.77) | |
| KPS | .32 | ||
| <90 | 145 (40.06) | 243 (43.24) | |
| 90-100 | 205 (56.63) | 308 (54.80) | |
| Missing | 12 (3.31) | 11 (1.96) | |
| Disease subtype | |||
| Primary | 269 (74.31) | 365 (64.95) | <.0001 |
| PPV-MF | 4 (1.10) | 131 (23.31) | |
| PET-MF | 89 (24.59) | 66 (11.74) | |
| Conditioning intensity | .02 | ||
| Myeloablative | 186 (51.38) | 245 (43.59) | |
| Reduced intensity/nonmyeloablative | 176 (48.62) | 317 (54.41) | |
| Conditioning regimen | .0003 | ||
| Flu + Bu ± other | 147 (40.61) | 261 (46.44) | |
| Flu + Mel ± other | 82 (22.65) | 167 (29.72) | |
| Flu + TBI ± other | 31 (8.56) | 35 (6.23) | |
| Others7 | 102 (28.18) | 99 (17.62) | |
| GVHD prophylaxis | .19 | ||
| CNI + MMF ± others | 68 (18.78) | 134 (23.84) | |
| CNI + MTX ± others | 224 (61.88) | 327 (58.19) | |
| Others | 70 (19.34) | 101 (17.97) | |
| DIPSS at transplant | .21 | ||
| Low | 26 (7.18) | 46 (8.19) | |
| Intermediate-1 | 74 (20.44) | 138 (24.56) | |
| Intermediate-2/high | 112 (30.94) | 142 (25.27) | |
| Missing | 150 (41.44) | 236 (41.99) | |
| Splenectomy before HCT | .30 | ||
| No | 185 (51.10) | 265 (47.15) | |
| Yes | 4 (1.10) | 12 (2.14) | |
| Unknown | 173 (47.79) | 285 (50.71) | |
| Time between diagnosis and HCT (mo) | .38 | ||
| <12 | 128 (35.56) | 185 (33.27) | |
| 12 to <24 | 58 (16.11) | 74 (13.31) | |
| 24 to <72 | 76 (21.11) | 139 (25.00) | |
| ≥72 | 98 (27.22) | 158 (28.42) | |
| Donor-recipient CMV serostatus | .68 | ||
| Positive-positive | 85 (23.48) | 150 (26.69) | |
| Positive-negative | 59 (16.30) | 76 (13.52) | |
| Negative-positive | 87 (24.03) | 141 (25.09) | |
| Negative-negative | 125 (34.53) | 186 (33.10) | |
| Missing | 6 (1.66) | 9 (1.60) | |
| Donor type | .41 | ||
| Unrelated | 304 (83.98) | 483 (85.94) | |
| Related | 58 (16.02) | 79 (14.06) | |
| Cytogenetics at transplant | .46 | ||
| Favorable normal | 110 (30.39) | 171 (30.43) | |
| Favorable other | 58 (16.02) | 70 (12.46) | |
| Adverse | 54 (14.92) | 86 (15.30) | |
| Missing | 140 (38.67) | 235 (41.82) | |
| Stem cell source | .31 | ||
| Bone marrow | 43 (11.88) | 55 (9.79) | |
| Peripheral blood | 319 (88.12) | 507 (90.21) | |
| Year at transplant | .65 | ||
| 2000-2004 | 22 (6.08) | 40 (7.12) | |
| 2005-2009 | 79 (21.82) | 111 (19.75) | |
| 2010-2016 | 261 (72.10) | 411 (73.13) |
Bu, Busulfan; CMV, cytomegalovirus; CNI, calcineurin inhibitor; Flu, fludarabine; GVHD, graft-versus-host disease; KPS, Karnofsky Performance Status; Mel, melphalan; MMF, mycophenolate mofetil; MTX: methotrexate; TBI, total body irradiation.
Almost all patients with MF with mCAs involving the JAK2 region were found to test -positive for JAK2V617F mutation (366 out of 374; 97.9%). The frequencies of patients who tested positive for both JAK2V617F mutation and mCA were as follow: 33.34% for PMF, 86.66% for PPV-MF, and 23.87% for PET-MF. CNLOH was the most frequent JAK2 chromosomal alteration, observed in 160 of 634 (25.2%) PMF, 106 of 135 (78.5%) PPV-MF, and 25 of 155 (16.1%) PET-MF (supplemental Table 2). The median allele burden for JAK2V617F mutation was 58%, 90%, and 59%, and the median mCA cellular fraction was 54%, 84%, and 34% in PMF, PPV-MF, and PET-MF, respectively (supplemental Table 3). We found a high positive correlation between JAK2V617F mutation allele burden and mCA cellular fraction across disease subtypes (r = 0.70 in PMF and in PPV-MF [P < .0001]; r = 0.49 in PET-MF [P = .002]).
There were no statistically significant differences in HCT outcomes based on the MF subtype (P > .1 for all). The probabilities of 3-year post-HCT OS were 55% (95% confidence interval [CI], 51-58) for PMF, 59% (95% CI, 51-67) for PPV-MF and 59% (51-66) for PET-MF (supplemental Table 4; supplemental Figure 1). The corresponding 3-year post-HCT cumulative incidence of relapse was 31% (95% CI, 28-35) for PMF, 31% (95% CI, 24-40) for PPV-MF, and 33% (95% CI, 26-41) for PET-MF; and of NRM = 29% (95% CI, 26-33) for PMF, 25% (95% CI, 18-32) for PPV-MF, and 23% (95% CI, 17-30) for PET-MF (supplemental Table 4).
In multivariable analyses, neither JAK2V617F mutation positivity nor allele burden was associated with risk of posttransplant mortality, overall or by disease subtype (Table 2). Of note, all 4 patients with PPV-MF who tested negative for the mutation died in the first 12 months after HCT. Moreover, the detected hazard ratios (HRs) for post-HCT mortality across MF subtypes were not different between patients with JAK2V617F mutation only and those with combined JAK2V617F mutation and mCAs in the same region, suggesting mCAs in this region had no modifying effect on post-HCT survival (supplemental Table 5).
Association of JAK2V617F mutation positivity and allele burden with posttransplant outcomes in MF, overall and by disease subtype
| JAK2 status/Allele burden (%) . | OS . | NRM . | Relapse . |
|---|---|---|---|
| HR∗ (95% CI); P . | |||
| PMF | |||
| Positive vs negative | 0.96 (0.75-1.21); .72 | 1.0 (0.75-1.34); .97 | 1.06 (0.80-1.39); .70 |
| <60% vs negative | 0.92 (0.80-1.22); .57 | 1.03 (0.73-1.44); .87 | 0.94 (0.67-1.31); .79 |
| ≥60% vs negative | 1.0 (0.76-1.31); .98 | 0.98 (0.69-1.39); .91 | 1.19 (0.86-1.65); .21 |
| Allele frequency† | 1.0 (0.99-1.00); .71 | 1.0 (0.99-1.00); .44 | 1.0 (0.99-1.01); .26 |
| PPV-MF‡ | |||
| Positive vs negative | NA | NA | NA |
| ≥90% vs <90% | 0.99 (0.56-1.73); .95 | 0.70 (0.34-1.45); .34 | 1.59 (0.82-3.09); .17 |
| Allele frequency† | 0.99 (0.98-1.00); .13 | 0.98 (0.97-1.00); .04 | 1.00 (0.99-1.02); .47 |
| PET-MF | |||
| Positive vs negative | 1.31 (0.78-2.20); .31 | 1.59 (0.76-3.35); .22 | 1.47 (0.83-2.60); .19 |
| <60% vs negative | 1.17 (0.61-2.22); .63 | 0.89 (0.34-2.31); .81 | 1.42 (0.73-2.77); .30 |
| ≥60% vs negative | 1.48 (0.78-2.82); .23 | 2.90 (1.21-6.93); .01 | 1.54 (0.72-3.30); .26 |
| Allele frequency† | 1.1 (0.99-1.02); .34 | 1.03 (1.01-1.06); .004 | 0.99 (0.98-1.01); .39 |
| JAK2 status/Allele burden (%) . | OS . | NRM . | Relapse . |
|---|---|---|---|
| HR∗ (95% CI); P . | |||
| PMF | |||
| Positive vs negative | 0.96 (0.75-1.21); .72 | 1.0 (0.75-1.34); .97 | 1.06 (0.80-1.39); .70 |
| <60% vs negative | 0.92 (0.80-1.22); .57 | 1.03 (0.73-1.44); .87 | 0.94 (0.67-1.31); .79 |
| ≥60% vs negative | 1.0 (0.76-1.31); .98 | 0.98 (0.69-1.39); .91 | 1.19 (0.86-1.65); .21 |
| Allele frequency† | 1.0 (0.99-1.00); .71 | 1.0 (0.99-1.00); .44 | 1.0 (0.99-1.01); .26 |
| PPV-MF‡ | |||
| Positive vs negative | NA | NA | NA |
| ≥90% vs <90% | 0.99 (0.56-1.73); .95 | 0.70 (0.34-1.45); .34 | 1.59 (0.82-3.09); .17 |
| Allele frequency† | 0.99 (0.98-1.00); .13 | 0.98 (0.97-1.00); .04 | 1.00 (0.99-1.02); .47 |
| PET-MF | |||
| Positive vs negative | 1.31 (0.78-2.20); .31 | 1.59 (0.76-3.35); .22 | 1.47 (0.83-2.60); .19 |
| <60% vs negative | 1.17 (0.61-2.22); .63 | 0.89 (0.34-2.31); .81 | 1.42 (0.73-2.77); .30 |
| ≥60% vs negative | 1.48 (0.78-2.82); .23 | 2.90 (1.21-6.93); .01 | 1.54 (0.72-3.30); .26 |
| Allele frequency† | 1.1 (0.99-1.02); .34 | 1.03 (1.01-1.06); .004 | 0.99 (0.98-1.01); .39 |
CMV, cytomegalovirus; GVHD, graft-versus-host disease; NA, nonapplicable
Survival models: adjusted for patient age, year of HCT, splenectomy before HCT, DIPSS, recipient-donor CMV serostatus match, donor type; NRM models: adjusted for age, CMV serostatus match, year of HCT, graft type, splenectomy, donor type, and conditioning intensity; relapse models: adjusted for splenectomy, conditioning intensity, DIPSS, GVHD prophylaxis, and stratified on year of HCT
Allele frequency is a continuous variable and tested only in patients with positive JAK2 mutation.
Mutation negative patients were excluded from this analysis because of small number (N = 4; all died in the first 12 months)
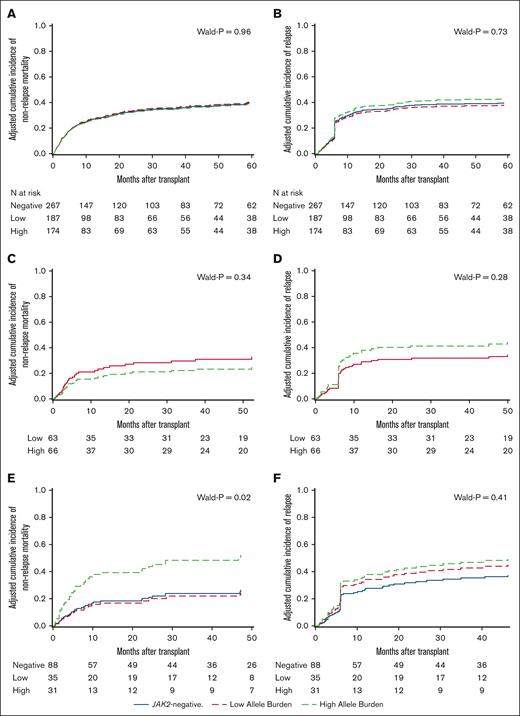
Multivariable analyses of risk of relapse or NRM in relation to JAK2V617F status showed no differences between patients positive and negative for JAK2V617F , overall or by disease subtype (Table 2). In analyses categorizing patients with JAK2V617F based on mutation allele burden and compared with those without the mutation, we observed a statistically significant association in patients with PET-MF between NRM and high mutation allele burden (≥60% vs negative; HR, 2.9; 95% CI, 1.21-6.93; P = .01) but not in those with low allele burden (<60% vs negative; HR, 0.89; 95% CI, 0.34-2.31; P = .81). Of note, almost all NRMs among those patients (PET-MF) occurred in the first year after HCT (N = 30 of 38 with NRM), with 60% of the death (N = 23) occurring in the first 6 months. This pattern was similar to that observed in PMF and PVT-MF with 60.8% and 68.6%, respectively, of NRM happened in the first 6 months after HCT. No statistically significant associations between allele burden and NRM were observed in patients with PMF or PPV-MF. For risk of relapse, no statistically significant associations by JAK2V617F allele burden were observed in any disease subtype (Figure 1; Table 2). Cause-of-death analyses did not show statistically significant associations with mutation allele burden (supplemental Tables 6 and 7).
Adjusted cumulative incidence of post-HCT NRM and relapse in MF patients by disease subtype. (A) NRM in PMF; (B) relapse incidence in PMF; (C) NRM in PPV-MF; (D) relapse incidence in PPV-MF; (E) NRM in PET-MF; (F) relapse incidence in PET-MF.
Adjusted cumulative incidence of post-HCT NRM and relapse in MF patients by disease subtype. (A) NRM in PMF; (B) relapse incidence in PMF; (C) NRM in PPV-MF; (D) relapse incidence in PPV-MF; (E) NRM in PET-MF; (F) relapse incidence in PET-MF.
Other factors associated with HCT OS in multivariable models for all patients with MF were patient age (P = .0004), calendar time (P = .0006), DIPSS (P = .005), and donor type (P = .04). Risk of NRM was associated with patient age (P < .0001), graft type (0.01), conditioning intensity (0.03), and calendar time (P = .0001). Risk of relapse was associated with DIPSS (0.005), and conditioning intensity (P = .03; supplemental Table 8). Similar trends were noted for all MF subtypes, which did not reach statistical significance in all cases, possibly owing to the small sample size.
We performed several secondary analyses (all multivariable) to confirm our JAK2 findings. First, to ensure adjustment for the possible residual confounders, we restricted the analyses to a subset of patients with comprehensive report forms (CRFs; N = 529), and a representative randomly selected a weighted sample whose detailed clinical information was collected, resulting in almost complete information on important clinical factors. Information on DIPSS was missing in only 8.3% of the CRF cohort as compared with in 41.7% of the full cohort. supplemental Table 9 summarizes the patient characteristics in the full and CRF cohorts. The result in this subset analysis was similar to that found in the main analyses indicating the robustness of the results of the full cohort (supplemental Table 10). Second, we reanalyzed the data using the total follow-up time (>10 years of data) with similar results to that of the main analyses ending at 5 years after HCT (supplemental Table 11). Finally, we stratified our analyses as per the calendar time of HCT (2000-2012 reflecting prephase and early phase of JAK inhibitors era and 2013 and later reflecting the era with expected high use of JAK inhibitors). For patients with PET-MF who underwent HCT in 2013 or later, analysis showed a threefold excess risk of NRM in patients with JAK2V617F compared with that in those without the mutation (HR, 3.53; 95% CI, 1.29-10.48; P = .02); this was particularly true for patients with high allele burden (HR, 7.65; 95% CI, 2.10-27.82; P = .002). There was no difference in NRM risk in patients with PET-MF who received transplant before 2013 by JAK2V617F mutation status or allele burden. Among patients with JAK2V617F-positive PET-MF, NRM due to infection-related causes (including acute respiratory distress syndrome) appeared to be more common in patients receiving HCT in the more recent era (N = 5 of 12 vs N = 2 of 11 in HCT performed 2013-2016 vs those before 2013, respectively; P = .26). The associations between HCT outcomes with JAK2V617F mutation for other MF subtypes were similar before and after 2013 (Table 3).
The association between HCT outcomes and JAK2V617F mutation allele burden in patients with MF by disease subtype before and after the introduction of JAK inhibitors (proxy year at HCT before 2013 and 2013+)
| . | OS∗ . | NRM† . | Relapse‡ . | |||
|---|---|---|---|---|---|---|
| HR1 . | P . | HR2 (95% CI) . | P . | HR3 (95% CI) . | P . | |
| PMF before 2013 | ||||||
| Positive vs negative | 1.22 (0.87-1.72) | .24 | 1.20 (0.79-1.82) | .38 | 1.01 (0.65-1.57) | .95 |
| <60% vs negative | 1.23 (0.82-1.81) | .32 | 1.47 (0.92-2.34) | .12 | 0.86 (0.49-1.52) | .61 |
| ≥60% vs negative | 1.22 (0.83-1.79) | .30 | 0.97 (0.59-1.60) | .97 | 1.15 (0.69-1.90) | .69 |
| PMF 2013+ | ||||||
| Positive vs negative | 0.82 (0.58-1.15) | .25 | 0.91 (0.59-1.40) | .68 | 1.02 (0.69-1.49) | .92 |
| <60% vs negative | 0.77 (0.51-1.15) | .20 | 0.74 (0.43-1.26) | .26 | 0.92 (0.59-1.43) | .73 |
| ≥60% vs negative | 0.88 (0.58-1.34) | .56 | 1.12 (0.68-1.85) | .64 | 1.16 (0.73-1.86) | .52 |
| PPV-MF before 2013§ | ||||||
| ≥90% vs <90% | 0.94 (0.39-2.24) | .89 | 1.15 (0.39-3.41) | .80 | 1.11 (0.38-3.23) | .85 |
| PPV-MF 2013+§ | ||||||
| ≥90% vs <90% | 0.98 (0.44-2.18) | .96 | 0.34 (0.12-0.99) | .05 | 1.82 (0.81-4.09) | .14 |
| PET-MF before 2013 | ||||||
| Positive vs negative | 1.12 (0.50-2.49) | .78 | 0.87 (0.25-3.04) | .83 | 2.19 (0.67-7.11) | .19 |
| <60% vs negative | 1.47 (0.52-4.15) | .46 | 0.93 (0.19-4.47) | .92 | 1.98 (0.49-8.06) | .34 |
| ≥60% vs negative | 0.94 (0.37-2.39) | .90 | 0.83 (0.21-3.35) | .80 | 2.37 (0.64-8.83) | .20 |
| PET-MF 2013+ | ||||||
| Positive vs negative | 1.78 (0.86-3.68) | .12 | 3.53 (1.29-10.48) | .02 | 1.62 (0.79-3.31) | .18 |
| <60% vs negative | 1.62 (0.70-3.77) | .26 | 1.99 (0.54-7.31) | .30 | 1.58 (0.69-3.61) | .27 |
| ≥60% vs negative | 2.04 (0.79-5.25) | .14 | 7.65 (2.10-27.82) | .002 | 1.69 (0.59-4.87) | .33 |
| . | OS∗ . | NRM† . | Relapse‡ . | |||
|---|---|---|---|---|---|---|
| HR1 . | P . | HR2 (95% CI) . | P . | HR3 (95% CI) . | P . | |
| PMF before 2013 | ||||||
| Positive vs negative | 1.22 (0.87-1.72) | .24 | 1.20 (0.79-1.82) | .38 | 1.01 (0.65-1.57) | .95 |
| <60% vs negative | 1.23 (0.82-1.81) | .32 | 1.47 (0.92-2.34) | .12 | 0.86 (0.49-1.52) | .61 |
| ≥60% vs negative | 1.22 (0.83-1.79) | .30 | 0.97 (0.59-1.60) | .97 | 1.15 (0.69-1.90) | .69 |
| PMF 2013+ | ||||||
| Positive vs negative | 0.82 (0.58-1.15) | .25 | 0.91 (0.59-1.40) | .68 | 1.02 (0.69-1.49) | .92 |
| <60% vs negative | 0.77 (0.51-1.15) | .20 | 0.74 (0.43-1.26) | .26 | 0.92 (0.59-1.43) | .73 |
| ≥60% vs negative | 0.88 (0.58-1.34) | .56 | 1.12 (0.68-1.85) | .64 | 1.16 (0.73-1.86) | .52 |
| PPV-MF before 2013§ | ||||||
| ≥90% vs <90% | 0.94 (0.39-2.24) | .89 | 1.15 (0.39-3.41) | .80 | 1.11 (0.38-3.23) | .85 |
| PPV-MF 2013+§ | ||||||
| ≥90% vs <90% | 0.98 (0.44-2.18) | .96 | 0.34 (0.12-0.99) | .05 | 1.82 (0.81-4.09) | .14 |
| PET-MF before 2013 | ||||||
| Positive vs negative | 1.12 (0.50-2.49) | .78 | 0.87 (0.25-3.04) | .83 | 2.19 (0.67-7.11) | .19 |
| <60% vs negative | 1.47 (0.52-4.15) | .46 | 0.93 (0.19-4.47) | .92 | 1.98 (0.49-8.06) | .34 |
| ≥60% vs negative | 0.94 (0.37-2.39) | .90 | 0.83 (0.21-3.35) | .80 | 2.37 (0.64-8.83) | .20 |
| PET-MF 2013+ | ||||||
| Positive vs negative | 1.78 (0.86-3.68) | .12 | 3.53 (1.29-10.48) | .02 | 1.62 (0.79-3.31) | .18 |
| <60% vs negative | 1.62 (0.70-3.77) | .26 | 1.99 (0.54-7.31) | .30 | 1.58 (0.69-3.61) | .27 |
| ≥60% vs negative | 2.04 (0.79-5.25) | .14 | 7.65 (2.10-27.82) | .002 | 1.69 (0.59-4.87) | .33 |
CMV, cytomegalovirus; GVHD, graft-versus-host disease.
Model: adjusted for patient age, year of HCT, splenectomy before HCT, DIPSS, recipient-donor CMV serostatus match, donor type.
Model adjusted for age, CMV serostatus match, year of HCT, graft type, splenectomy, donor type, and conditioning intensity.
Model adjusted for splenectomy, conditioning intensity, DIPSS, GVHD prophylaxis, and stratified on year of HCT.
Mutation negative patients were excluded because of small number (N = 4; all died in the first 12 months).
Discussion
We investigated the effect of JAK2V617F mutation and associated mCAs spanning the JAK2 region on post-HCT outcomes in real-world registry data from a large cohort of patients with primary or secondary MF. We observed that JAK2V617F mutation status, mutation allele burden, or JAK2 mCAs were not associated with risk of relapse, NRM, or OS after transplantation in PMF. Almost all patients with PPV-MF tested JAK2V617F positive, with no association between HCT outcomes and mutation allele burden. In contrast, high allele burden in patients with PET-MF was associated with excess risk of NRM, but not OS, in the recent era since JAK inhibitors became mainstream therapy.
Recent evidence suggests that MF subtypes are distinct clinical entities warranting tailored risk stratification tools and treatment modalities.18 In this study, focusing on JAK2V617F mutations, disease differences in frequencies and allele burden were noted. In agreement with previous reports in non-HCT settings, almost all patients with PPV-MF and half of the patients with PMF and PET-MF tested positive for the mutation.5,17,28JAK2V617F allele burden in our study was highest in patients with PPV-MF (90%), vs ∼60% in patients with PMF and PET-MF.
We showed that almost all patients with MF with mCAs involving JAK2 were also having JAK2V617F and that 40% of the patients carried both alterations. This supports our recent genome-wide association study findings indicating that mCAs are secondary events that selectively retain or duplicate the JAK2V617F mutation and promote rapid clonal expansion of mutated clones.16 However, our analyses showed similar HCT outcomes for patients carrying JAK2V617F mutation only and those with both alterations, for both primary and secondary MF. This finding suggested no modifying effect for mCAs involving the JAK2 region on the association between JAK2V617F mutation and HCT outcomes.
In line with MF disease subtype distinctiveness, 1 large study of 1099 patients (only 10% underwent HCT) reported that patients with PET-MF had better survival than those with PMF or PPV-MF (3 years OS reported in a large single center study = 69% in PET-MF, 63% in PPV-MF and 55% in PMF; P < .001).29 In this study, we showed similar post-HCT survival across the 3 disease entities (3 years OS of 55% in PMF and 59% in PPV-MF and PET-MF; P = .29) in contrast with a previous HCT report of 233 patients with MF showing a better survival in patients with secondary MF than those with PMF (HR, 0.62; P = .02).30 Differences in patient selection, disease status, or transplant factors could explain outcome differences.
The effects of JAK2V617F mutation on MF prognosis have been thoroughly investigated in non-HCT settings.31-33 However, its role in the HCT setting is still controversial.34-38 This is particularly noted in light of improved HCT survival in patients with CALR mutation (∼20% of patients with MF), which was used as a reference group in several studies and led to the conclusion that JAK2 mutation or triple negative status (negative for JAK2, CALR, and MPL) are associated with post-HCT survival disadvantage.34,35 The 6-year OS for those with CALR-positive status was 81% or 72% in reduced intensity or myeloablative regimens, respectively vs 58% or 55%, respectively, for JAK2-positives and 55% in either regimen for triple negative patients, respectively.35 In our study, we focused on MF disease subtype-specific associations and the presence or absence of JAK2 genomic alterations (JAK2V617F mutation, its allele burden, or associated mCAs) to possibly guide clinical decisions related to use of JAK inhibitors after transplantation. We found no evidence of associations between acquired JAK2 genomic alterations and post-HCT survival or disease relapse/progression in any MF disease subtype. Interestingly, these null associations were noted before or after JAK inhibitors became available, suggesting that the use of JAK inhibitors may not significantly affect survival or disease relapse after HCT. However, prospective randomized trials are warranted to directly answer this question.
The detected elevated risk of NRM in relation to the high allele burden of JAK2V617F mutation in PET-MF, but not other MF subtypes, needs further evaluation. Interestingly, the observed excess risk was restricted to HCTs performed after 2012. The NRM difference between MF disease subtypes is likely not explained by the disease severity profile or lag time between diagnosis and transplant because the same severity profile was noted for patients with PPV-MF but did not lead to an excess risk of NRM. The observed early NRM in PET-MF (60% in the first 6 months after HCT) may be attributed to a hyperinflammatory state associated with JAK2-mutation burden. MF is an oncoinflammatory disease model39 with known proinflammatory cytokine profile (reviewed in Gleitz et al40). Therefore, if JAK inhibitor use, schedule, and pre-HCT tapering was different between MF subtypes, this may explain the JAK2 associations with NRM in patients with PET-MF in which they might have received HCT in an active inflammation state. A future study with detailed JAK inhibitor practice is needed to answer this question.
We comprehensively investigated the impact of JAK2 alterations including JAK2V617F mutation status, allele burden, and associated mosaic chromosomal alterations on HCT outcomes in patients with MF, in a large real-world registry study. The large sample size and availability of biospecimens and clinical data for all 3 MF disease subtypes allowed for evaluating disease subtype-specific associations with separate analyses for PMF, PPV-MF, and PET-MF. The extended HCT calendar time (between 2000 and 2016) allowed us to stratify the analysis based on the pre- and post-JAK inhibitors era to indirectly evaluate their possible modifiable effect on HCT outcomes. We also recognize limitations associated with the sole investigation of JAK2 genomic alterations without assessing other MF driver genes (CALR and MPL) or high molecular risk mutations (mutations in ASXL1, SRSF2, EZH2, IDH1, or IDH2). In a recent study, mutations in CALR or MPL were associated with better survival than JAK2 or triple negatives, but patients with ASXL1-positive status had worse survival than those without this mutation in a cohort of patients with primary or secondary MF; possible differences based on the MF subtype were not tested.35 The reported relapse in this study was based on center definition which is known to be based on different clinical and molecular standard. Experts across the world are calling for standardization of HCT end point definitions (including relapse) for patients with MF.41 Similarly, causes of NRM lack standardized reporting practices across different centers. A previous large study showed that in 20% of the cases, causes of NRM were subject to reclassification after expert review.42
In conclusion, we showed that HCT outcomes in PMF and PPV-MF were not associated with JAK2V617F mutation status, mutation allele burden, or JAK2 mCAs. However, patients with PET-MF with high JAK2V617F mutation allele burden were at increased risk of NRM, which did not translate into a statistically significant survival disadvantage. These findings further support the concept that allogeneic HCT can mitigate the negative effect of JAK2V617F in patients with MF, particularly for PMF and PPV-MF. Future studies with comprehensive genomic assessments including a MF full mutational profile might identify important genes or variants that also could influence HCT outcomes.
Acknowledgments
The authors acknowledge the research contributions of the CGR Laboratory for their expertise, execution, and support of this research in the areas of project planning, wet-laboratory processing of specimens, and bioinformatics analysis of generated data. This work was supported by the Intramural Research Program of the Division of Cancer Epidemiology and Genetics, National Cancer Institute, National Institutes of Health. The CIBMTR is supported primarily by Public Health Service U24CA076518 from the National Cancer Institute, the National Heart, Lung, and Blood Institute, and the National Institute of Allergy and Infectious Diseases; HHSH250201700006C from the Health Resources and Services Administration; and N00014-21-1-2954 and N00014-23-1-2057 from the Office of Naval Research; support was also provided by Be The Match Foundation, the Medical College of Wisconsin, and the National Marrow Donor Program. The Cancer Genomics Research Laboratory is funded with federal funds from the National Cancer Institute, National Institutes of Health, under NCI contract number 75N910D00024. The content of this publication does neither necessarily reflect the views or policies of the Department of Health and Human Services, nor does the mention of trade names, commercial products, or organizations imply endorsement by the US Government.
Authorship
Contribution: S.M.G. and W.S. developed the concept of the study and designed it; W.S., M.H., S.R.S., T.W., S.J.L., Y.T.B., S.J.C., and A.S.M. were responsible for the acquisition of biological samples and clinical data; M.R., S.M.G., W.S., V.G., H.J.D., and Y.W. took part in data analysis and/or interpretation; D.W.B., W.Z., M.M., K.J., and W.L. were involved in genomic analysis and bioinformatics; M.R. and S.M.G. drafted the manuscript; M.R. and S.M.G. conducted the statistical analysis; and all the authors critically revised the manuscript for important intellectual content.
Conflict-of-interest disclosure: V.G. provided consultancy for Novartis, BMS Celgene, Sierra Oncology, AbbVie, Constellation Biopharma, and Pfizer; and participated on a data safety monitoring board or advisory board for BMS Celgene, Roche, AbbVie, and Pfizer. The remaining authors declare no competing financial interests.
Correspondence: Shahinaz Gadalla, Division of Cancer Epidemiology and Genetics, National Cancer Institute, National Institutes of Health, 9609 Medical Center Dr, Room 6E-452, Rockville, MD 20850-9772; email: gadallas@mail.nih.gov.
References
Author notes
SNP-array and JAK2 sequencing data used in this study are available in Database of Genotypes and Phenotypes (dbGaP) (accession number phs002635.v1.p1).
The data set used for this analysis will be available at https://cibmtr.org/CIBMTR/Resources/Publicly-Available-Datasets1#.
Other data are available on request from the corresponding author, Shahinaz M. Gadalla (gadallas@mail.nih.gov).
The full-text version of this article contains a data supplement.